Abstract
Aims
Recently, the association between anemia and diabetic microvascular complications has been studied. Diabetic peripheral neuropathy (DPN) is also a common complication of type 2 diabetes mellitus (T2DM), while the relationship between anemia and DPN is rarely investigated. The aim of this study is to evaluate the association between anemia and DPN in T2DM.
Methods
In this cross-sectional study, 1134 T2DM inpatients were enrolled. The diagnosis of DPN was based on neuropathy system score (NSS) and neuropathy disability score (NDS). Logistic regression was conducted to analyze the association between anemia and DPN.
Results
The proportions of anemia in DPN and non-DPN group were 25.4 and 15.2%, respectively. Compared with non-anemia group, the proportions of moderate/severe NSS (42.7 vs. 24.5%, P < 0.001) and moderate/severe NDS (51.5 vs. 38.0%, P < 0.001) were higher while the nerve conduction velocity (NCV) was lower in anemia group. Univariate logistic regression analysis showed patients with anemia possessed an increased risk of DPN [OR = 1.906, 95%CI: 1.416, 2.567, P < 0.001]. Multivariate logistic regression analysis suggested anemia was an independent risk factor of DPN in model 1 and model 2 [model 1: OR = 1.472, 95%CI: 1.047, 2.070, P = 0.026; model 2: OR = 1.448, 95%CI: 1.013, 2.071, P = 0.043].
Conclusions
Anemia is an independent risk factor of DPN in T2DM patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type 2 diabetes mellitus (T2DM) has been considered as a major public health issue throughout the world, and in a global context its prevalence is increasing rapidly including in China [1]. Diabetic peripheral neuropathy (DPN) is one of the most common complications of diabetes and may be present in nearly 50% of T2DM [2]. Hyperglycemia has been considered to be a major pathophysiologic factor in the development of DPN in T2MD. However, researchers have shown that some of the patients with DPN are still in a worse off condition even with strictly controlled blood glucose [3], which indicates that other factors are also involved in the development of DPN in T2DM apart from the chronic hyperglycemia.
Anemia is one of the most common hematologic disorders in the world, and the prevalence of anemia in diabetic patients was found to be two to three times higher than in general population [4]. Recently, the association of anemia and diabetic microvascular complications has been studied. Anemia has been considered as a frequent complication of diabetic nephropathy (DN) [5] and an independent risk factor that predicts adverse outcomes and mortality in patients with DN [6, 7]. Anemia was also identified as an independent risk factor of diabetic retinopathy (DR) [8, 9], and severer retinopathy was found in anemia patients than in non-anemia patients [10].
Peripheral neuropathy is also a chronic microvascular complication of T2DM, and risk factors of DPN were not fully understood. Bosman et al. [11] investigated the symptoms and signs of DPN in a total of 27 T1DM patients with DN and reported that the anemia group had severer impaired thermal perception compared with the non-anemia group. To the best of our knowledge, the relationship between anemia and DPN is rarely investigated in T2DM patients. The goal of this study is to evaluate the association between anemia and DPN in T2DM patients.
Materials and methods
Subjects
In this cross-sectional study, we enrolled 1134 T2DM inpatients at the First Affiliated Hospital of Chongqing Medical University (FAHCMU). The age ranged from 20 to 75 years old. T2DM was diagnosed according to American Diabetes Association standards. The exclusion criteria were as follows: (1) subjects who had other potential causes of neuropathy (i.e., alcohol abuse, connective tissue disease and thyroid disease); (2) subjects who had hemolytic anemia or aplastic anemia; (3) subjects who had peripheral vascular disease (ankle brachial index ≤0.9) or had a history of cerebral infraction, cervical spondylosis or lumbar spondylosis; (4) subjects who had advanced renal failure [eGFR <40 ml/min/1.73m2], heart failure or hepatic failure; and (5) subjects who suffered from malignant disease or in poor general condition. This study was approved by the Research Ethics Committee of Chongqing Medical University, and informed consent was obtained from all participants before the survey.
Data collection
The information on family history of diabetes and lifestyle information (including smoking behavior and alcohol consumption) were collected through physician interviews. Height, weight, heart rate, systolic and diastolic blood pressure (SBP and DPB) were measured by using standard apparatus during medical examinations. The body mass index (BMI) of each subject was calculated by dividing weight by the square of height (Kg/m2).
Laboratory measurements
After an overnight fasting, blood and urine samples of each subject were collected and sent to the medical examination center of the FAHCMU. Hemoglobin (Hb) level was measured by full automatic blood cell counter hematology analyser (SysmexXE-5000, Japan). The fasting plasma glucose (FPG) level and 2h postprandial plasma glucose (2h-PG) level were measured by a hexokinase assay (Olympus Diagnostics, Tokyo, Japan). Glycosylated hemoglobin (HbA1c) level was assessed by high-pressure liquid chromatography (Trinity Biotech, PremierHb9210, Ireland). The fasting serum total cholesterol (TC), triglyceride (TG), high-density lipoprotein cholesterol (HDL-C) and low-density lipoprotein cholesterol (LDL-C) were measured by an enzymatic assay (Wako Diagnostics, Tokyo, Japan).The serum creatinine (Cr) was determined by using enzymatic methods (Roche Diagnostic, Mannheim, Germany). High-sensitivity C-reactive protein (hs-CRP) was measured by a rate immune scatter turbidimetry method (Beckman Coulter). The estimated glomerular filtration rate (eGFR) level was calculated by using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation [12]. Urinary albumin and creatinine concentration were measured by turbidimetric immunoassay and enzymatic colorimetric method on an automatic analyser (Hitachi 7600, Tokyo, Japan).
Assessment of neuropathy
The diagnosis of DPN was based on the neuropathy system score (NSS) and neuropathy disability score (NDS) [13].
NSS: patients were asked about the feelings in their legs: numbness, burning or tingling (score 2), fatigue, cramping or aching (score 1). The exact position: the feet (score 2), the calves (score 1) and elsewhere (score 0). Time: daytime alone (score 0), both day and night (score 1), nocturnal exacerbation (score 2), waking the patient from sleep (score 3). Maneuvers of reducing the symptoms: sitting or lying down (score 0), standing (score 1), walking (score 2). According to scores, NSS has three ranks, 3–4 is mild, 5–6 is moderate and 7–9 is severe.
NDS: it includes ankle reflexes, 128 Hz tuning fork vibration, pinprick and temperature sensation at the hallux. Ankle reflexes: normal (score 0), present with reinforcement (score 1) or absent (score 2) per side. Sensation: present (score 0) or reduced/absent (score 1) for each side. According to scores, NDS has three ranks, 3-5 is mild, 6–8 is moderate and 9–10 is severe.
The criteria for DPN are as follows: (1) moderate/severe NDS. (2) mild NDS + moderate/severe NSS.
Nerve conduction velocity tests
Nerve conduction velocities (NCV) of tibial, peroneal and sural nerves (both sides of each subject) were assessed using Dantec Keypoint electromyogram system (Dantec Medical, Skovlunde, Denmark) by the same trained physician. The motor nerve conduction velocity (MNCV) on tibial and peroneus nerves as well as the sensory nerve conduction velocity (SNCV) on tibial and sural nerves was analyzed.
Diagnosis of anemia, hypertension, coronary heart disease (CHD), DR and DN
Based on the World Health Organization (WHO) standard (1999 version), anemia was defined as hemoglobin <12 g/dL for females and <13 g/dL for males. The patients were considered to be hypertensive if receiving antihypertensive medication (as documented in clinical records) or SBP ≥140 mm Hg or DBP ≥90 mm Hg. The patients were diagnosed as CHD according to diagnostic criteria established by American Heart Association. DR was assessed by professional ophthalmologist according to clinical symptoms and eye examination (fluorescent fundus angiography or ophthalmofundoscopy). Identification of DN was relied upon assessments of kidney function with estimated eGFR <60 ml/min/1.73 m2 or urinary albumin-to-creatinine ratio (ACR) >30 mg albumin per gram of creatinine (mg/g).
Statistical analyses
Analyses were performed using SPSS software (version 16.0; SPSS Inc., Chicago, IL, USA). One-sample Kolmogorov–Smirnov tests were performed to test whether distribution of variables was normal. Variables distributed normally were presented as mean ± SD, while variables with skewed distribution were presented as medians (interquartile range). Categorical variables were reported as frequencies and proportions. An independent sample t test was used to compare continuous variables between two groups. The Mann–Whitney U test was used for non-normally distributed variables. Chi-Square test was used to analyze the categorical date. We conducted univariate logistic regression analysis to identify potential variables associated with DPN. Multivariate logistic regression analysis was performed to detect the relationship between anemia and DPN. Several models were built to adjust for confounding factors, including variables which showed significantly difference in univariate logistic regression and other known confounders. The variance inflation factor (VIF) was used to check the multicollinearity of variables in logistic models. Three methods (forward elimination method, backward elimination method and enter method) were performed to select significant independent variables in logistic regression.
Results
A total of 1134 T2DM inpatients were analyzed in this study. Among them, 574 (50.6%) were identified with DPN and 560 (49.4%) were not. The overall prevalence of anemia was 20.4% (231/1134). The demographic, clinical and biological characteristics between DPN group and non-DPN group are summarized in Table 1.
Compared with patients without DPN, patients with DPN had higher proportion of anemia (25.4 vs. 15.2%, P < 0.001). Lower hemoglobin levels were found in both males (13.96 ± 1.54 vs. 14.65 ± 1.48 g/dL, P < 0.001) and females (12.40 ± 1.47 vs. 12.9 ± 1.29 g/dL, P < 0.001) of DPN group. The age, duration of diabetes and SBP were higher (all P < 0.001), while eGFR (P < 0.05) was lower in DPN group. Additionally, compared with the non-DPN group, the prevalence of hypertension, DR, DN and CHD was higher in DPN group (all P < 0.05). No significant difference was found in BMI, FPG, 2h-PG or HbA1c levels between DPN group and non-DPN group (Table 1).
Comparison of symptoms and signs of DPN between the anemia group (231 patients) and non-anemia group (903 patients) is displayed in Table 2. The prevalence of DPN (63.2 vs. 47.4%, P < 0.001) was significantly higher in the patients with anemia. Compared with non-anemia group, the proportion of moderate/severe NSS (43.0 vs. 24.5%, P < 0.001) and moderate/severe NDS (51.5 vs. 38.0%, P < 0.001) was significantly higher in anemia group. To be specific, proportions of absent ankle reflex, reduced/absent sensation of vibration, pinprick and temperature were higher in anemia group compared with non-anemia group (all P < 0.05).
Comparison of electrophysiological characteristics between anemia group and non-anemia group is shown in Table 3. The MNCV of tibial and peroneal nerves, and the SNCV of tibial and sural nerves were all lower in T2DM patients with anemia, but only the differences of MNCV of left tibial nerve (41.71 ± 5.40 vs. 43.80 ± 4.46, P < 0.001), SNCV of left tibial nerve (distal) (39.86 ± 4.98 vs. 41.41 ± 5.70, P = 0.008), SNCV of right tibial nerve (distal) (40.13 ± 5.75 vs. 41.78 ± 5.39, P = 0.005) and SNCV of right tibial nerve (proximal) (41.98 ± 5.69 vs. 43.34 ± 5.38, P = 0.021) between the two groups reached statistical significance.
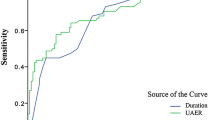
Table 4 shows the association between anemia and DPN. Univariate logistic regression analysis (model crude) showed patients with anemia possessed an increased risk of DPN [OR = 1.906, 95%CI: 1.416, 2.567, P < 0.001]. Except for anemia, the following variables also reached significance in univariate logistic regression: gender, age, height, duration of diabetes, SBP, DBP, TC, LDL-c, eGFR, hypertension, CHD, DR and DN (see Online Resource 1). In multivariate logistic regression analysis, gender, age, height, duration of diabetes, HbA1c, eGFR, SBP, DBP, TC and LDL-c were adjusted in model 1; gender, age, height, duration of diabetes, HbA1c, eGFR, SBP, DBP, TC, LDL-c, hypertension, metformin exposure, coronary heart disease, diabetic retinopathy and diabetic nephropathy were adjusted in model 2. All factor in models has VIF value <5. The results of multivariate logistic regression suggested anemia was an independent risk factor of DPN in both model 1 and model 2 [model 1: OR = 1.472, 95%CI: 1.047, 2.070, P = 0.026; model 2: OR = 1.448, 95%CI: 1.013, 2.071, P = 0.043].
Discussion
In this cross-sectional study, we have provided evidence of an association between anemia and DPN in T2DM. Of note, this relationship was independent of known risk factors of DPN, including age, height, duration of diabetes, HbA1c, dyslipidemia, hypertension, CHD, DN and DR [14,15,16].
According to our study, above half of T2DM subjects had DPN, which is in accordance with domestic and foreign researches [17, 18]. Nearly 20% of T2DM patients had anemia, which is consistent with other study [4]. Patients with DPN had significantly lower hemoglobin levels in both male and female and had higher proportion of anemia compared with non-DPN, which is consistent with the finding of He et al. [9].
The proportion of DPN was increased in anemia group compared with non-anemia group. The anemia group had severer impaired temperature sensation comparing with non-anemia group, which is consistent with the finding from Bosman et al. [11]. What’s more, there was evidence of severer impaired ankle reflex, vibration sensation and pinprick sensation in anemia group. Additionally, it was easy to find individuals with anemia in T2DM have lower MNCV and SNCV of some nerves compared with non-anemia patients. Although the most common type of DPN is distal symmetric polyneuropathy [2], there are still some patients’ clinical symptoms are asymmetric and atypical in our study. That’s why there was the difference between left and right tibialis in MNCV while the similarity between left and right tibialis in SNCV, when we made comparison of NCV between anemia and non-anemia group.
Some explanations were needed to be clarified for our main findings. Although anemia is often severer and occurs earlier in patients with DN than in patients without DN [19], we found the association between anemia and DPN was independent of DN in T2DM patients without overt neuropathy. Our finding may be explained by Symeonidis’ study which reported that even though patients with advanced renal failure typically develop anemia because of the impaired production of erythropoietin (EPO) [20], there was no relationship between EPO and Hb levels in T2DM patients without overt nephropathy [21]. Further studies are required to determine the relationship between DN and anemia in T2DM without advanced renal failure. Metformin exposure may also be a cause for exacerbation of DPN for metformin was reported to decrease the level of serum vitamin B12. Moreover, severer peripheral neuropathy was present in patients with metformin exposure than patients without metformin exposure [22]. However, we didn’t find significant association between metformin exposure and DPN. In addition, in current study, compared with the non-DPN group, the DPN group had lower levels of TC and LDL-C, which could probably be explained by the fact that the DPN patients had early intervention of antihyperlipidemic agents and better management of lipid profiles.
Anemia is a common complication in T2DM patients. Although the cause of anemia in T2DM is not fully understand, EPO deficiency has been considered as a major one [4]. Early study suggested that EPO has neuroprotective effects in the central nervous system and peripheral nerves in rats with streptozotocin-induced diabetes [23]. Recent study reported that in nerve crush injury, EPO treatment promoted myelin formation and protected myelin from the effects of nitric oxide exposure. EPO may exert a primary influence on myelin status to promote functional recovery [24]. Other study showed EPO may promote peripheral nerve repair in rat model through the upregulation of insulin-like growth factor-1 (IGF-1) expression [25]. Therefore, we hypothesized EPO deficiency may be a mechanism linking anemia and DPN in T2DM.
Anemia has been reported to induce organ hypoxia. It is possible that anemia could cause renal tissue hypoxia, which contributes to the progression of kidney disease to end stage [7]. Anemia-induced retinal hypoxia was considered as the reason for the development or worsening of DR [8,9,10]. Similarly, the role of anemia in the exacerbation of endoneurial hypoxia might be a possible explanation for the association between anemia and DPN. The vitality of peripheral nerve axons depends on the nerve microenvironment which includes blood supply, oxygenation and nutrition. Reduced microvascular blood flow and oxygenation may result in endoneurial hypoxia [26]. Any factor which exacerbates endoneurial hypoxia is considered to accelerate nerve injury. For instance, in patients with asymmetrical peripheral vascular disease, severer impairment of nerve function was found in the leg which suffered heavier ischemia [27]. In our study, participants with anemia had severer neuropathy than those without anemia. We hypothesized that anemia-induced low oxygen carrying capacity may cause endoneurial hypoxia, which strongly correlates with the severity of nerve-fiber pathology [28] and may increase the risk of DPN.
Reportedly, anemia is considered to be associated with oxidative stress [29] which is also an important mechanism of DPN [30]. Erythrocytes represent as an important component of the antioxidant capacity of blood, which mainly include superoxide dismutase, catalase and the glutathione system. Circulating erythrocytes are mobile free radical scavengers and provide antioxidant protection to other tissues and organs [31]. The antioxidant system is markedly weakened by anemia, resulting in increased free radical production. The imbalance between free radicals and antioxidant may lead to oxidative stress and result in endothelial dysfunction which plays a key role in the development of DPN [26, 28]. Thus, oxidative stress may be another mechanism linking anemia with DPN in T2DM. Clinical studies of raising erythrocyte level or improving anemic status are required to determine whether it is good for inhibition of oxidative stress and preventing the development or progression of DPN.
The present study had several limitations. Firstly, several other confounding influencing factors on DPN were not excluded, such as insufficient serum folic acid and vitamin B12 deficiency. Secondly, as a cross-sectional study, we could not prove the causality between anemia and development of DPN. Thirdly, according to the exclusion criteria, the group of our study may not necessarily represent DPN patients in general (for example, we exclude patients with ABI index below 0.9 or subjects who had advanced renal failure). Finally, the patients involved were from one single center, bias of selection and information could not be avoided.
In conclusion, our findings suggested anemia is an independent risk factor of DPN in T2DM patients. T2DM patients with anemia had severer neurological symptoms and signs, and lower NCV of some nerves compared with non-anemia counterparts. More attention should be paid to anemia; early screening for signs and symptoms of DPN may be necessary in T2DM patients with anemia. Prospective and multi-center studies are required to explore whether anemia plays a direct role in the development, progression or adverse outcomes of DPN.
References
Bi Y, Xu Y, Ning G (2014) Prevalence of diabetes in Chinese adults–reply. JAMA 311(2):200–201. doi:10.1001/jama.2013.283143
Pop-Busui R, Boulton AJ, Feldman EL et al (2017) Diabetic neuropathy: a position statement by the american diabetes association. Diabetes Care 40(1):136–154. doi:10.2337/dc16-2042
Charles M, Ejskjaer N, Witte DR, Borch-Johnsen K, Lauritzen T, Sandbaek A (2011) Prevalence of neuropathy and peripheral arterial disease and the impact of treatment in people with screen-detected type 2 diabetes: the addition-denmark study. Diabetes Care 34(10):2244–2249. doi:10.2337/dc11-0903
Thomas MC, MacIsaac RJ, Tsalamandris C, Power D, Jerums G (2003) Unrecognized anemia in patients with diabetes: a cross-sectional survey. Diabetes Care 26(4):1164–1169
Ritz E (2006) Anemia and diabetic nephropathy. Curr Diabetes Rep 6(6):469–472
Joss N, Patel R, Paterson K, Simpson K, Perry C, Stirling C (2007) Anaemia is common and predicts mortality in diabetic nephropathy. QJM: Mon J Assoc Phys 100(10):641–647. doi:10.1093/qjmed/hcm080
Mohanram A, Zhang Z, Shahinfar S, Keane WF, Brenner BM, Toto RD (2004) Anemia and end-stage renal disease in patients with type 2 diabetes and nephropathy. Kidney Int 66(3):1131–1138. doi:10.1111/j.1523-1755.2004.00863.x
He BB, Wei L, Gu YJ et al (2012) Factors associated with diabetic retinopathy in chinese patients with type 2 diabetes mellitus. Int J Endocrinol 2012:157940. doi:10.1155/2012/157940
He BB, Xu M, Wei L et al (2015) Relationship between anemia and chronic complications in chinese patients with type 2 diabetes mellitus. Arch Iranian Med 18(5):277–283
Qiao Q, Keinanen-Kiukaanniemi S, Laara E (1997) The relationship between hemoglobin levels and diabetic retinopathy. J Clin Epidemiol 50(2):153–158
Bosman DR, Winkler AS, Marsden JT, Macdougall IC, Watkins PJ (2001) Anemia with erythropoietin deficiency occurs early in diabetic nephropathy. Diabetes Care 24(3):495–499
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612
Young MJ, Boulton AJ, MacLeod AF, Williams DR, Sonksen PH (1993) A multicentre study of the prevalence of diabetic peripheral neuropathy in the United Kingdom hospital clinic population. Diabetologia 36(2):150–154
Tesfaye S, Chaturvedi N, Eaton SE et al (2005) Vascular risk factors and diabetic neuropathy. N Engl J Med 352(4):341–350. doi:10.1056/NEJMoa032782
Bansal D, Gudala K, Muthyala H, Esam HP, Nayakallu R, Bhansali A (2014) Prevalence and risk factors of development of peripheral diabetic neuropathy in type 2 diabetes mellitus in a tertiary care setting. J Diabetes Investig 5(6):714–721. doi:10.1111/jdi.12223
Smith AG, Singleton JR (2013) Obesity and hyperlipidemia are risk factors for early diabetic neuropathy. J Diabetes Complicat 27(5):436–442. doi:10.1016/j.jdiacomp.2013.04.003
Tesfaye S, Boulton AJ, Dyck PJ et al (2010) Diabetic neuropathies: update on definitions, diagnostic criteria, estimation of severity, and treatments. Diabetes Care 33(10):2285–2293. doi:10.2337/dc10-1303
Lu B, Yang Z, Wang M et al (2010) High prevalence of diabetic neuropathy in population-based patients diagnosed with type 2 diabetes in the Shanghai downtown. Diabetes Res Clin Pract 88(3):289–294. doi:10.1016/j.diabres.2010.02.002
Symeonidis A, Kouraklis-Symeonidis A, Psiroyiannis A et al (2006) Inappropriately low erythropoietin response for the degree of anemia in patients with noninsulin-dependent diabetes mellitus. Ann Hematol 85(2):79–85. doi:10.1007/s00277-005-1102-9
Radtke HW, Claussner A, Erbes PM, Scheuermann EH, Schoeppe W, Koch KM (1979) Serum erythropoietin concentration in chronic renal failure: relationship to degree of anemia and excretory renal function. Blood 54(4):877–884
Spallone V, Maiello MR, Kurukulasuriya N et al (2004) Does autonomic neuropathy play a role in erythropoietin regulation in non-proteinuric Type 2 diabetic patients? Diabetic Med 21(11):1174–1180. doi:10.1111/j.1464-5491.2004.01306.x
Wile DJ, Toth C (2010) Association of metformin, elevated homocysteine, and methylmalonic acid levels and clinically worsened diabetic peripheral neuropathy. Diabetes Care 33(1):156–161. doi:10.2337/dc09-0606
Bianchi R, Buyukakilli B, Brines M et al (2004) Erythropoietin both protects from and reverses experimental diabetic neuropathy. Proc Natl Acad Sci USA 101(3):823–828. doi:10.1073/pnas.0307823100
Sundem L, Chris Tseng KC, Li H, Ketz J, Noble M, Elfar J (2016) Erythropoietin enhanced recovery after traumatic nerve injury: myelination and localized effects. J Hand Surg 41(10):999–1010. doi:10.1016/j.jhsa.2016.08.002
Wang W, Li D, Li Q et al (2015) Erythropoietin promotes peripheral nerve regeneration in rats by upregulating expression of insulin-like growth factor-1. Arch Med Sci: AMS 11(2):433–437. doi:10.5114/aoms.2015.50976
Nukada H (2014) Ischemia and diabetic neuropathy. Handb Clin Neurol 126:469–487. doi:10.1016/B978-0-444-53480-4.00023-0
Veves A, Donaghue VM, Sarnow MR, Giurini JM, Campbell DR, LoGerfo FW (1996) The impact of reversal of hypoxia by revascularization on the peripheral nerve function of diabetic patients. Diabetologia 39(3):344–348
Tesfaye S (2011) Recent advances in the management of diabetic distal symmetrical polyneuropathy. J Diabetes Investig 2(1):33–42. doi:10.1111/j.2040-1124.2010.00083.x
Grune T, Sommerburg O, Siems WG (2000) Oxidative stress in anemia. Clin Nephrol 53(1 Suppl):S18–22
Albers JW, Pop-Busui R (2014) Diabetic neuropathy: mechanisms, emerging treatments, and subtypes. Curr Neurol Neurosci Rep 14(8):473. doi:10.1007/s11910-014-0473-5
Siems WG, Sommerburg O, Grune T (2000) Erythrocyte free radical and energy metabolism. Clin Nephrol 53(1 Suppl):S9–17
Acknowledgements
The authors thank the First Affiliated Hospital of Chongqing Medical University. This research was supported by National Key Clinical Specialties Construction Program of China (Grant Number: 2011-170) and National Natural Science Foundation of China Grants (Grant Number: 81200588). Rong Li has full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analyses.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Fan Wu, Yuanyuan Jing, Xiaojun Tang, Dai Li, Lilin Gong, Hongyan Zhao, Li He, Qifu Li and Rong Li declare that they have no conflict of interest.
Ethical standard
The ethical committee of Chongqing Medical University approved this study. The approved number is 20130024. All procedures followed were performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent disclosure
Informed consent was obtained from all individual participants included in the study.
Additional information
Managed by Massimo Porta.
Fan Wu and Yuanyuan Jing are co-first authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wu, F., Jing, Y., Tang, X. et al. Anemia: an independent risk factor of diabetic peripheral neuropathy in type 2 diabetic patients. Acta Diabetol 54, 925–931 (2017). https://doi.org/10.1007/s00592-017-1025-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-017-1025-7