Abstract
Aims
Women who had gestational diabetes mellitus (GDM) have a high risk of type 2 diabetes mellitus (T2DM) in the years following pregnancy. Most follow-up screening studies have been conducted in limited geographical areas leading to large variability in the results. The aim of our investigation was to measure how the publication of guidelines affected early screening for T2DM after a pregnancy with GDM during the period 2007–2013, in France.
Methods
We conducted a retrospective cohort study in a representative sample of 1/97th of the French population using data from the “National Health Insurance Inter-Regime Information System,” which collects individual hospital and non-hospital data for healthcare consumption.
Results
The sample included 49,080 women who gave birth in 2007–2013. In the following 3 months, only 18.49% of women with GDM had an oral glucose tolerance test or a blood glucose test in 2007. This rate had not significantly increased in 2013 (p = 0.18). The proportion of women with GDM who had the recommended glycemic follow-up at 3 months (20.30 vs. 21.58%, p = 0.19) and 6 months (32.48 vs. 37.16%, p = 0.08) was not significantly different before the guidelines (2008–2009) and after the guidelines (2012–2013). At 12 months, the difference was significant (46.77 vs. 54.05%, p = 0.009).
Conclusion
Postpartum screening has improved only slightly since the guidelines and remains largely insufficient, with less than 25% of women with GDM screened in the first 3 months. In the first year after delivery, less than 60% of women were screened for T2DM.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Aims
The prevalence of gestational diabetes mellitus (GDM) is similar in most high-income countries. In 2010, in the United States of America, 9.2% of pregnancies were complicated by GDM [1]. In 2011, in Europe, GDM was estimated at 2–6% [2], and it currently complicates about 8% of pregnancies in France [3].
GDM carries an immediate risk of adverse maternal, fetal and neonatal outcomes [4], and in the years following pregnancy, women who had GDM have a high risk of developing Type 2 Diabetes Mellitus (T2DM) [5,6,7,8]. Without intervention, most women develop T2DM within the first 10 years postpartum. Finally, 70% of women affected by GDM experience the emergence of T2DM in the 28 years postpartum [5]. The first years after pregnancy are essential as T2DM screening will not be proposed if women have no other risk factors and as T2DM is often diagnosed when major diabetes complications appear [9]. Early screening could reduce this late diagnosis. At the individual level, screening is important for initiating both drug therapy and the lifestyle interventions necessary to manage diabetes or impaired glucose tolerance [10]. Diabetes screening is also important for the performance of health systems. Appropriate screening leads to efficient prevention, which may help to diminish the human and financial burden of the unceasing increase in the incidence of diabetes.
Since the early 2000s, most high-income countries (Scotland in 2010, Denmark in 2009, UK-NICE in 2008, Italy in 2007, USA-ADA in 2003) have issued guidelines about the frequency of diabetes mellitus screening for women with a history of GDM [8, 11,12,13,14]. In 2010, the French guidelines also recommended T2DM screening, which should be performed at 6–10 weeks postpartum and every 1–3 years thereafter, depending on the risk factors [15].
Screening for diabetes following a pregnancy affected by GDM is generally reported to be low. Most follow-up-screening studies have been conducted in limited geographical areas leading to large variability in screening rates, which range from 6 to 80% [16,17,18,19,20,21,22,23,24]. To our knowledge, no study has been conducted using data for the overall population of large countries. Moreover, no study has assessed the evolution of screening for diabetes mellitus following the publication of guidelines. We hypothesized that the publication of guidelines would lead to an improvement in T2DM screening.
The aim of our study was to measure how the publication of updated guidelines in December 2010 affected early screening for T2DM after a pregnancy with GDM in France.
Methods
The principle of this retrospective cohort study was to examine data for women with GDM from 2007 to 2013. Our study involved a representative sample of 1/97th of the French population. This sample was made available for approved studies, from the “National Health Insurance Inter-Regime Information System” (SNIIRAM) which collects individual hospital and non-hospital data for healthcare consumption. These data correspond to automatically recorded healthcare consumption. Each biological test, treatment, medical transport or any other consumption is reimbursed by the French health insurance agency and therefore recorded in SNIIRAM.
These data include all types of mandatory health insurance systems (the main health insurance, health insurance for agricultural workers and farmers, for the self-employed and 12 other specific health insurance schemes) covering more of 90% of French population, and our sample includes the main types of mandatory health insurance (the main health insurance, health insurance for agricultural workers and farmers, and the self-employed) covering more than 86% of the French population. The SNIIRAM sample was constructed at the national level, by the French health insurance agency, which manages its representativity. It was drawn randomly from a check digit of the beneficiary’s identification number.
Hospital data came from all public and private hospitals. These data are grouped in a national database called “The French Medical Information System Program in Medicine, Surgery and Obstetrics” (PMSI-MCO), before being transmitted and included in the SNIIRAM. To ensure the quality of hospital data, various quality control procedures were carried out on samples a posteriori by the Medical Information Departments of each healthcare establishment and by territorial medical inspectors, in accordance with a legislative text. For 20 years, hospital data have been used for medical research purposes and the quality of the French hospital database has been confirmed in recent studies. Our team has conducted many validation studies which showed the value of using these data in epidemiology [25,26,27,28,29]. In particular, a pilot study assessed the metrological quality of medico-administrative data for perinatal indicators in three university hospitals. The results showed that data from medical records and hospital data were in good agreement [30]. Medico-administrative data provide a huge amount of epidemiological information concerning hospitalized patients in France [31,32,33,34].
From a representative sample of the French population, the data allowed us to estimate follow-up while excluding the effects of the geographical area, health facility or practices.
In the hospital data, deliveries were identified by the codes Z37 (outcome of delivery) which were considered the most reliable and extensive. Among these women, the code O24.4 (diabetes mellitus arising in pregnancy) in the main or associated diagnosis according to International Classification of Diseases (ICD-10) was used to select women who had GDM. While GDM screening was offered to all pregnant women until 2010, it is now recommended in all women with a high risk of diabetes (maternal age ≥ 35 years, BMI ≥ 25 kg/m2, women who have first-degree relative with diabetes, prior history of GDM or delivery of large-for-gestational-age infant). Screening now involves a fasting blood glucose test at the initial prenatal visit and then an oral glucose tolerance test (OGTT) at 24–28 weeks of amenorrhea [15]. Since the 2010 guidelines, the threshold for fasting blood glucose to diagnose GDM in early pregnancy is above 0.92 g/l (5.1 mmol/l) and those for the 75 g-OGTT (75 g at 24–28 weeks) are 1.80 g/l (10.0 mmol/l) at 1 h and 1.53 g/l (8.5 mmol/l) at 2 h [4]. Before 2010, this screening was conducted in two time points. GDM was diagnosed using the 100 g-OGTT if two values were greater than or equal to 0.95 g/l 1 (5.3 mmol/l) at 0 h, 1.80 g/l (10.1 mmol/l) at 1 h, 1.55 g/l (8.7 mmol/l) at 2 h and 1.40 g/l (7.8 mmol/l) at 3 h.
To describe screening for T2DM in these women, we studied their epidemiological follow-up between the delivery and 2015, from non-hospital data.
Screening for T2DM was explored from the analyses of blood glucose levels: oral glucose tolerance test (OGTT) (codes 0412 and 0413), blood glucose test (BGT) (code 0552) and HbA1C (code 1577), from version 42 of the national table of biology. The code 0552 (BGT) refers to a blood glucose test, without specification. Even though we are not sure that BGT was systematically performed in a fasting state, physicians and biologists are strongly encouraged to perform this analysis in a fasting state in current medical practice in France (page 5, lines 126–128).
Although the OGTT is the most sensitive test, the BGT was included as it was recommended in the 2010 guidelines. As HbA1c is better accepted by women and physicians [35, 36] and actually recommended by the American Diabetes Association since 2014, this test was explored in order to ensure that the T2DM screening was not carried out using a test which has not been studied [37].
Statistical analysis
We determined the proportion of women who underwent glucose testing at least once in the 3, 6, 12 and 36 months after delivery. We used the Cochran–Armitage test to evaluate trends in these percentages over the years. The 36-month period relates women who gave birth until 2012.
The influence of new guidelines (updated in December 2010) was estimated by a before/after study which did not take into account the year preceding (2010) and the year following the French guidelines (2011). To test these comparisons, we used the Chi-squared test. SAS 9.3 software was used for analysis.
Results
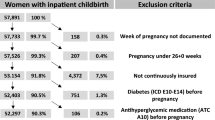
The SNIIRAM sample included 49,080 women who gave birth from 2007 to 2013. Among these, 238 women in 2007 (3.75%) and 548 women in 2013 (7.38%) had GDM. Almost one-third of women with GDM were 35 years of age or older, and about 7.83–18.06% of women with GDM had a pre-pregnancy body mass index (BMI) greater than or equal to 30 kg/m2 (Table 1).
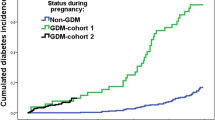
Early T2DM screening is presented in Fig. 1. In 2007, only 18.4% of women with GDM had an OGTT or a BGT in the first 3 months following delivery. This rate did not significantly increase from 2007 to 2013 (p = 0.18). Less than 7% of all women with GDM were tested with the OGTT.
Concerning the first 6 months after delivery, the proportion of all women with GDM screened for T2DM increased significantly from 31.9% in 2007 to 39.4% in 2013 (p = 0.04), but remained less than 40%.
In the 12 months after delivery, the proportion of women with GDM screened for T2DM increased significantly from 48.3% in 2007 to 56.3% in 2013 (p = 0.008).
The percentage of women with GDM screened in the 36 months following delivery was relatively stable, 77.31% in 2007 and 77.26% in 2012.
HbA1C alone was performed in less than 3.5% of women with GDM, with no significant difference post-guidelines.
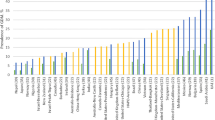
Before the guidelines (2008–2009), the proportion of women with GDM who had the recommended glycemic tests (OGTT or BGT) in 2010 was 18.93% at the first 3 months, 32.98% at the first 6 months and 47.48% within a period of 12 months. After the guidelines (2012–2013), this proportion did not significantly increase at 3 months (21.58%, p = 0.21) or 6 months (37.16%, p = 0.08). However, the proportion of women with GDM who had the recommended glycemic follow-up within a period of 12 months increased significantly (54.05%, p = 0.01) (Table 2).
From 2007 to 2012, the proportion of women who actually fulfilled the recommendations (screened at 6–12 weeks postpartum and again every 1 or 3 years) was 5.88% in 2007, 10.32% in 2008 and about 9% from 2009 to 2013 (Fig. 2). The differences were not significant (p = 0.36). Considering the periods before (2009) and after (2012) the guidelines, there was no significant difference in the proportion of women who actually fulfilled the recommendations: 9.1% in 2009 and 9.3% in 2012 (p = 0.93).
Discussion
For several years, GDM has been acknowledged as a risk factor for developing T2DM in the years following pregnancy. In high-income countries, guidelines include systematic early screening for T2DM, but the impact of these guidelines on screening has not been assessed. Our study over 7 years showed that the introduction of guidelines in 2010 hardly affected T2DM screening, even though a slight increase in DT2 screening was observed in the year following a pregnancy affected by GDM.
The strength of this study lies in fact that it was based on national data; it thus excluded the effects of the geographical area, health facility or medical practices. In fact, French hospital data are able to identify deliveries with a difference of 0.3% compared with the national civil registry, which records all births in France [21]. Then, the hospital data allowed us to select women who had GDM. In 2011, using French hospital data and SNIIRAM data, Billionnet et al. [38] reported a prevalence of GDM of 6.4%. In our study, in 2011, we found a prevalence of GDM of 6.02% using only diagnosis ICD-10 codes recorded in hospital discharge abstracts. The data for T2DM screening tests in the study population are rather exhaustive as national health insurance is compulsory and a free health insurance exists for people with the lowest income.
We acknowledge that the present study may have some limitations. First, the selection of women with gestational diabetes was conducted using diagnostic codes from hospital data. However, a prior study showed a positive predictive value for gestational diabetes in hospital data of 88.9% [CI: 74.3–100] as compared to medical records in three university hospitals [30]. Second, some specific health insurance schemes which represent 4% of the population covered by French health insurance were not included in our sample.
An important result of our study is the lack of screening in the postpartum period. After the guidelines, postpartum screening within the 3 months following delivery did not improve, with less than 25% of women following the recommendation for screening within 6–12 weeks. In this period, other studies have identified the lack of time spent on self-care and the impossibility to plan baby’s demands as an obstacle to T2DM screening [22, 39]. In contrast, in Denmark, Olesen et al. [22] reported high compliance with screening (80.5%) at 3 months thanks to visits to the general practitioner, who did the screening test at the time of the consultation.
Our study also pointed out the delay in screening for diabetes prior to pregnancy, as the proportion of screened women almost doubled between three and 6 months after delivery. We found that in 2009 only 31.3% of women with GDM were screened in the first 6 months after pregnancy and this increased to 35.9% in 2010. These results are consistent with those of Cosson et al. [40], who, in the same period (2009–2010), found a rate of T2DM screening of 33.3% at the four largest maternity units in the area.
To our knowledge, our study is the first to have determined the evolution of screening for diabetes mellitus after the publication of guidelines in 2010. By comparing T2DM screening before and after 2010, we showed that the guidelines led to a statistically significant increase in the testing rate in the year following GDM. However, from a clinical point of view, the impact of the guidelines seems to be rather low since just over half of the women with GDM were screened for T2DM in the first year after pregnancy. Moreover, after the guidelines, less than 10% of women with history of GDM were screened as recommended: first T2DM screening at 6–12 weeks postpartum, second screening at 1 or 3 years after the first test and then every 1 or 3 years thereafter. Despite a substantial increase in diabetes prevalence and growing awareness of the scale of this health problem, screening for T2DM after a history of GDM remains clearly inadequate. Guidelines alone do not seem to be sufficient to meet the goal of effective screening.
In the literature, even though there have been no large-scale evaluations of the evolution of screening for diabetes mellitus after the publication of guidelines, many authors have focused on the impact of health interventions. Several studies have concluded that a health intervention increased the rate of screening in women who had GDM [22, 40,41,42,43,44]. Although the rates of T2DM screening remain low in routine practice, active care and reminders for physicians and women seem to increase the proportion of women screened for T2DM. For example, in Canada, Clark et al. studied the impact of sending reminders to physicians and/or women. When reminders were not sent, only 14.3% of women were screened by OGTT. This proportion increased to 51.6% when only physicians received a reminder, 55.3% when a reminder was sent to the women only and 60.5% when women and physicians received reminders [43]. In France, Cosson et al. showed that a mobilization campaign (multidisciplinary meetings in maternity units, documents for women, prescription of OGTT and a letter to each caregiver, particularly to improve collaboration) led to a greater proportion of women screened in the first 6 months postpartum (48.9 vs. 33.3%, odds ratio 1.7, 95% CI [1.1–2.5]) [40].
Conclusion
Despite a slight improvement in T2DM screening in the year following a pregnancy with GDM following the 2010 guidelines, screening practices fall far short of the guidelines and this problem needs to be dealt with urgently to tackle the diabetes epidemic. Taking into account the results of intervention studies, we have to find the best way to make pregnancy a key opportunity to involve of all of the actors (private general practitioners, hospital-based physicians and women) in screening as specified in guidelines.
References
DeSisto CL, Kim SY, Sharma AJ (2014) Prevalence estimates of gestational diabetes mellitus in the United States, pregnancy risk assessment monitoring system (PRAMS), 2007–2010. Prev Chronic Dis 11:E104
Buckley BS, Harreiter J, Damm P et al (2012) Gestational diabetes mellitus in Europe: prevalence, current screening practice and barriers to screening. A review. Diabet Med J Br Diabet Assoc 29(7):844–854
Regnault N, Salanave B, Castetbon K et al (2016) Gestational diabetes in France in 2012: screening, prevalence and treatment modalities during pregnancy. Bull Epidémiol Hebd 9:164–173
HAPO Study Cooperative Research Group, Metzger BE, Lowe LP et al (2008) Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 358(19):1991–2002
Kim C, Newton KM, Knopp RH (2002) Gestational diabetes and the incidence of type 2 diabetes: a systematic review. Diabet Care 25(10):1862–1868
Rayanagoudar G, Hashi AA, Zamora J et al (2016) Quantification of the type 2 diabetes risk in women with gestational diabetes: a systematic review and meta-analysis of 95,750 women. Diabetologia 59(7):1403–1411
Köhler M, Ziegler AG, Beyerlein A (2016) Development of a simple tool to predict the risk of postpartum diabetes in women with gestational diabetes mellitus. Acta Diabetol 53(3):433–437
Noctor E, Crowe C, Carmody LA et al (2015) ATLANTIC-DIP: prevalence of metabolic syndrome and insulin resistance in women with previous gestational diabetes mellitus by International Association of Diabetes in Pregnancy Study Groups criteria. Acta Diabetol 52(1):153–160
American Diabetes Association (2010) Standards of medical care in diabetes-2010. Diabetes Care 33(Suppl 1):S11–S61
Barry E, Roberts S, Oke J et al (2017) Efficacy and effectiveness of screen and treat policies in prevention of type 2 diabetes: systematic review and meta-analysis of screening tests and interventions. BMJ 356:i6538
Scottish Intercollegiate Guidelines NetworK. Healthcare Improvement Scotland. Management of diabetes. Quick Reference GuideMarch 2010. [Internet]. Disponible sur. http://www.sign.ac.uk/pdf/qrg116.pdf
Damm P, Ovesen P, Andersen LL et al. Clinical guidelines for gestational diabetes mellitus. [Internet]. Disponible sur. http://www.endocrinology.dk/kliniske%20retningslinier%20-%20GDM.pdf
Simmons D, McElduff A, McIntyre HD, Elrishi M (2010) Gestational diabetes mellitus: NICE for the US? A comparison of the American Diabetes Association and the American College of Obstetricians and Gynecologists guidelines with the U.K. National Institute for Health and Clinical Excellence guidelines. Diabetes Care 33(1):34–37
De Micheli A (2008) Italian standards for diabetes mellitus 2007: executive summary : diabete Italia, AMD associazione medici diabetologi, SID Società Italiana di Diabetologia. Acta Diabetol 45(2):107–127
Collège National des Gynécologues et Obstétriciens Français (2010) Société francophone du diabète. [Gestational diabetes]. J Gynecol Obstet Biol Reprod (Paris) 39(8 Suppl 2):S139, S338–S342
Carson MP, Frank MI, Keely E (2013) Original research: postpartum testing rates among women with a history of gestational diabetes—systematic review. Prim Care Diabetes 7(3):177–186
Nielsen KK, Kapur A, Damm P, de Courten M, Bygbjerg IC (2014) From screening to postpartum follow-up—the determinants and barriers for gestational diabetes mellitus (GDM) services, a systematic review. BMC Pregnancy Childbirth 14:41
Kim C, Tabaei BP, Burke R et al (2006) Missed opportunities for type 2 diabetes mellitus screening among women with a history of gestational diabetes mellitus. Am J Public Health 96(9):1643–1648
Shah BR, Lipscombe LL, Feig DS, Lowe JM (2011) Missed opportunities for type 2 diabetes testing following gestational diabetes: a population-based cohort study. BJOG Int J Obstet Gynaecol 118(12):1484–1490
Chamberlain C, McLean A, Oats J et al (2015) Low rates of postpartum glucose screening among indigenous and non-indigenous women in Australia with gestational diabetes. Matern Child Health J 19(3):651–663
Hunt KJ, Conway DL (2008) Who returns for postpartum glucose screening following gestational diabetes mellitus? Am J Obstet Gynecol 198(4):404.e1–404.e6
Olesen CR, Nielsen JH, Mortensen RN et al (2014) Associations between follow-up screening after gestational diabetes and early detection of diabetes—a register based study. BMC Public Health 14:841
Blatt AJ, Nakamoto JM, Kaufman HW (2011) Gaps in diabetes screening during pregnancy and postpartum. Obstet Gynecol 117(1):61–68
Clark HD, van Walraven C, Code C, Karovitch A, Keely E (2003) Did publication of a clinical practice guideline recommendation to screen for type 2 diabetes in women with gestational diabetes change practice? Diabetes Care 26(2):265–268
Quantin C, Benzenine E, Fassa M et al (2012) Evaluation of the interest of using discharge abstract databases to estimate breast cancer incidence in two French departments. J Int Assoc Off Stat 28:73–85
Quantin C, Benzenine E, Ferdynus C et al (2013) Advantages and limitations of using national administrative data on obstetric blood transfusions to estimate the frequency of obstetric hemorrhages. J Public Health Oxf Engl 35(1):147–156
Quantin C, Benzenine E, Velten M et al (2013) Self-controlled case series and misclassification bias induced by case selection from administrative hospital databases: application to febrile convulsions in pediatric vaccine pharmacoepidemiology. Am J Epidemiol 178(12):1731–1739
Aboa-Eboulé C, Mengue D, Benzenine E et al (2013) How accurate is the reporting of stroke in hospital discharge data? A pilot validation study using a population-based stroke registry as control. J Neurol 260(2):605–613
Quantin C, Cottenet J, Vuagnat A et al (2014) Quality of perinatal statistics from hospital discharge data: comparison with civil registration and the 2010 National Perinatal Survey. J Gynecol Obstet Biol Reprod (Paris) 43(9):680–690
Goueslard K, Revert M, Pierron A et al (2016) Evaluation of the metrological quality of medico-administrative data for perinatal indicators: a pilot study. J Community Med Health Educ 6:437
Abdulmalak C, Cottenet J, Beltramo G et al (2015) Haemoptysis in adults: a 5-year study using the French nationwide hospital administrative database. Eur Respir J 46(2):503–511
Lainay C, Benzenine E, Durier J et al (2015) Hospitalization within the first year after stroke: the Dijon stroke registry. Stroke 46(1):190–196
Lorgis L, Cottenet J, Molins G et al (2013) Outcomes after acute myocardial infarction in HIV-infected patients: analysis of data from a French nationwide hospital medical information database. Circulation 127(17):1767–1774
Goueslard K, Cottenet J, Mariet A-S et al (2016) Early cardiovascular events in women with a history of gestational diabetes mellitus. Cardiovasc Diabetol 15:15
Tovar A, Chasan-Taber L, Eggleston E, Oken E (2011) Postpartum screening for diabetes among women with a history of gestational diabetes mellitus. Prev Chronic Dis 8(6):A124
Wilkinson SA, Lim SS, Upham S et al (2014) Who’s responsible for the care of women during and after a pregnancy affected by gestational diabetes? Med J Aust 201(3 Suppl):S78–S81
American Diabetes Association (2014) Standards of medical care in diabetes—2014. Diabetes Care 37(Suppl 1):S14–S80
Billionnet C, Weill A, Ricordeau P et al (2014) Diabète gestationnel et grossesse: données de la population française 2011. Diabetes Metab 40(1):A15
Bennett WL, Ennen CS, Carrese JA et al (2011) Barriers to and facilitators of postpartum follow-up care in women with recent gestational diabetes mellitus: a qualitative study. J Womens Health 20(2):239–245
Cosson E, Bihan H, Vittaz L et al (2015) Improving postpartum glucose screening after gestational diabetes mellitus: a cohort study to evaluate the multicentre IMPACT initiative. Diabet Med J Br Diabet Assoc 32(2):189–197
Keely E, Clark H, Karovitch A, Graham I (2010) Screening for type 2 diabetes following gestational diabetes: family physician and patient perspectives. Can Fam Phys Med Fam Can 56(6):558–563
Chittleborough CR, Baldock KL, Taylor AW et al (2010) Long-term follow-up of women with gestational diabetes mellitus: the South Australian Gestational Diabetes Mellitus Recall Register. Aust N Z J Obstet Gynaecol 50(2):127–131
Clark HD, Graham ID, Karovitch A, Keely EJ (2009) Do postal reminders increase postpartum screening of diabetes mellitus in women with gestational diabetes mellitus? A randomized controlled trial. Am J Obstet Gynecol 200(6):634.e1–634.e7
Yarrington C, Zera C (2015) Health systems approaches to diabetes screening and prevention in women with a history of gestational diabetes. Curr Diabetes Rep 15(12):114
Acknowledgements
This work was supported by the Public Health Research Institute (Institut de Recherche en Santé Publique: IRESP) in 2017.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard
This study was approved by the French Institute of Health Data (IDS) (registration number 114, 3 February 2015).
Informed consent
Written consent was not needed for this study since this study used an anonymized database and had no influence on patients care.
Additional information
Managed by Massimo Porta.
Rights and permissions
About this article
Cite this article
Goueslard, K., Cottenet, J., Mariet, AS. et al. Early screening for type 2 diabetes following gestational diabetes mellitus in France: hardly any impact of the 2010 guidelines. Acta Diabetol 54, 645–651 (2017). https://doi.org/10.1007/s00592-017-0986-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-017-0986-x