Abstract
Women with previous gestational diabetes (GDM) are a high-risk group for future development of diabetes, metabolic syndrome, and cardiovascular disease. The new International Association of Diabetes in Pregnancy Study Groups (IADPSG) criteria significantly increase the number of women diagnosed with GDM. The long-term metabolic outcome in these women is unknown. We set out to determine the prevalence of metabolic syndrome, using adult treatment panel-III criteria; and insulin resistance, using HOMA2-IR, in white European women with previous GDM. Using a cohort design, we invited women meeting IADPSG GDM criteria across four Irish antenatal centres between 2007 and 2010 to participate. Two hundred and sixty-five women with previous values meeting IADPSG criteria for GDM participated (44 % of the population eligible for participation). Mean age was 36.7 years (SD 5.0). These women were compared with a randomly selected control group of 378 women (mean age 37.6 years, SD 5.1) known to have normal glucose tolerance (NGT) in pregnancy during the same period. A total of 25.3 % of women with previous IADPSG-defined GDM met metabolic syndrome criteria, compared to 6.6 % of women with NGT [at 2.6 (SD 1.0) vs. 3.3 years (SD 0.7) post-partum]. The prevalence of HOMA2-IR >1.8 was higher in women with previous IADPSG-defined GDM (33.6 vs. 9.1 % with NGT, p < 0.001). Women with previous GDM by IADPSG criteria demonstrate a greater than threefold prevalence of metabolic syndrome compared to women with NGT in pregnancy. Efforts to prevent projected long-term consequences of this should focus on interventions both in the preconception and post-partum periods.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the first standardised diagnostic criteria were introduced in 1964, the post-partum sequelae of gestational diabetes mellitus (GDM) have been extensively described. Having a history of GDM has been associated with a greater post-partum risk of diabetes [relative risk (RR) of 7.7 vs. women with normal glucose tolerance (NGT) in pregnancy] [1], increased cardiovascular risk [hazard ratio (HR) 1.71 at 11.5 years] [2], and an increased prevalence of metabolic syndrome (up to threefold increase vs. women without GDM at 9 years) [3]. In 2010, the diagnostic criteria for GDM underwent their most significant change in over 40 years. The original 1964 O’Sullivan and Mahan criteria [4] (later adopted by the National Diabetes Data Group-NDDG) [5], and their modified form, the Carpenter–Coustan criteria [6], identified a cohort of women at greatly increased risk of type 2 diabetes [7]. The World Health Organisation (WHO) criteria for diagnosis of GDM simply represented values diagnostic of diabetes mellitus (1980–1999) [8] or impaired glucose tolerance (1999–2013) [9] in the non-pregnant population. However, none of these criteria were based on the pregnancy outcomes in women with GDM. In the light of this, the International Association for Diabetes in Pregnancy Study Groups (IADPSG) consensus panel met in 2008. Their recommendations included lowering the fasting and 1-h thresholds for GDM diagnosis [10], and also allowing a diagnosis to be made on the basis of a single abnormal value (rather than the two abnormal values required in the NDDG and Carpenter–Coustan criteria). Adoption of these criteria will lead to an increased proportion of pregnant women receiving a diagnosis of GDM (prevalence was as high as 25 % among some of the hyperglycaemia and adverse pregnancy outcome—HAPO-study centres) [11]. As the IADPSG recommendations are increasingly adopted by major bodies (the American Diabetes Association [12] and WHO [13] have endorsed the IADPSG diagnostic criteria at the time of writing), quantifying the future implications of this change in diagnostic criteria becomes essential. In particular, the metabolic and cardiovascular risk profile beyond the immediate post-partum period of women who meet the new IADPSG criteria remains unclear, and thus, the optimal clinical follow-up strategy cannot be determined.
Although the diagnostic utility of metabolic syndrome as a clinical entity has been questioned [14], it is beyond doubt that it does, at the very least, represent a clustering of cardiovascular risk factors. A diagnosis of metabolic syndrome is associated with several adverse outcomes: type 2 diabetes, (RR 3.53) [15] increased cardiovascular risk (RR 1.65) [16], and all-cause mortality (RR 1.27). Given the young age, and short post-partum duration, at which increased cardiovascular risk has been shown to emerge in women with previous GDM [2], identification of those at risk affords a unique opportunity to intervene in an attempt to ameliorate this excess risk. Our group has previously shown a prevalence of metabolic syndrome [using adult treatment panel-III (ATP-III) criteria] of 10.8 % at 12 weeks post-partum in women meeting IADPSG criteria for GDM [17], although this did not differ significantly from those women with normal glucose tolerance (NGT) in pregnancy (8.2 % prevalence; OR 1.12, 95 % CI 0.59–2.16). With this in mind, we set out to evaluate the prevalence of both the metabolic syndrome (ATP-III criteria) and insulin resistance (HOMA2-IR), as assessed by the HOMA computer model (homoeostatic model assessment) in a cohort of women meeting IADPSG criteria for previous GDM, and NGT controls, at medium-term follow-up (up to 5 years).
Methods
The methods of recruitment for this study, and the prevalence of abnormal glucose tolerance in this cohort, have been described previously [18]. Exclusion criteria were development of type 1 diabetes after the index pregnancy, current pregnancy, and non-white European ethnicity. The cohort screened in our original ATLANTIC-DIP study contained only 7.1 % of women of non-white ethnicity, but accounted for 16.7 % of GDM cases. To control for this effect, we limited this study to women of white European origin only. We recruited 270 women (44 % of 607 eligible participants identified) across four centres, who had a pregnancy with a date of delivery between January 2007 and December 2010, and who had values diagnostic of GDM when the IADPSG criteria were retrospectively applied (WHO 1999 GDM diagnostic criteria were in clinical use during the study). GDM was diagnosed using a 2 h 75 g OGTT with 0, 1, and 2 h values, carried out at 24–28 weeks gestation in the index pregnancy. This time period included an 18-month period of universal screening as part of our original study protocol [19]. Risk-factor-based screening was used for the remainder of the study period. The criteria in use at that time for risk-factor-based screening recommended testing for GDM using a 75-g oral glucose tolerance test (OGTT) if any one of the following risk factors were present; history of diabetes mellitus in a first-degree relative; a BMI ≥30 kg/m2; maternal age ≥40 years; previous unexplained perinatal death; glycosuria; long-term steroids; previous baby weighing ≥4.5 kg; a history of polycystic ovarian syndrome; polyhydramnios or macrosomia on ultrasound in the current pregnancy, and ethnicity. A control group, consisting of 388 women (24 % of 1,610 eligible participants identified by random selection) who had attended for universal screening during this period, but met IADPSG criteria for NGT, was also invited to participate. Local ethics committee approval was obtained for the study, and informed consent was obtained from all participants.
In addition to evaluation of glucose tolerance using a 75 g OGTT and haemoglobin A1c (HbA1c), results of which have been described in a previous paper [18], participants underwent anthropometric (weight, height, waist circumference) and blood pressure measurements. Blood samples were also drawn for determination of serum low-density lipoprotein (LDL), high-density lipoprotein (HDL), total cholesterol, triglycerides, fasting insulin levels, and C-peptide levels. Participants also completed a questionnaire detailing risk factors for both GDM and type 2 diabetes.
Plasma glucose was determined using the hexokinase method (Roche Modular Analytics <P> Chemistry Systems). The between-run coefficient of variation (CV) for glucose at mean concentrations of 2.56, 7.11, and 16.7 mmol/L was 1.1, 0.9, and 1.0 %, respectively. Insulin and C-peptide were analysed using solid-phase, 2-site electrochemiluminescent immunometric assays (Roche E170 Modular Analytics Immunoassay Systems). The between-run CVs for insulin at mean concentrations of 127, 367, and 880 pmol/L were 1.8, 1.9, and 1.1 %, respectively, and for C-peptide, at mean concentrations of 398, 1,310, and 2,750 pmol/L were 1.3, 1.2, and 1.3 %, respectively. Haemoglobin A1c was determined using the Menarini HA8160 automated analyser. The method principle is based on reverse phase cation exchange chromatography and is fully traceable to the International Federation of Clinical Chemistry (IFCC) standard. Total and HDL-cholesterol, and serum triglycerides were determined using the Roche Modular Analytics <P> Chemistry Systems. The methodology employed is based on the use of enzymes, while LDL-cholesterol was calculated using the Friedwald equation.
The HOMA2-IR computer model was used to estimate both insulin resistance and beta-cell function. Insulin concentrations were entered to determine values for HOMA2-IR where possible, and when insulin levels were unavailable (n = 24), C-peptide concentrations were used to calculate this instead. Values for beta-cell function (HOMA-%B) were calculated using C-peptide concentrations where possible, and insulin levels (n = 4) when C-peptide was unavailable. These recommendations are in line with the principles outlined by the authors in describing the recommended use of the HOMA2-IR computer model [20]. Varying HOMA2-IR cut-offs for insulin resistance have been described in populations with different age profiles [21–24], and from higher-risk ethnic groups [25]. For this study, the 90th percentile in the reference population (women with previous NGT in pregnancy) was used to determine the cut-off value to define insulin resistance, corresponding to a HOMA2-IR value of 1.8.
Metabolic syndrome in this study was defined by the presence of 3 out of 5 of the following criteria; waist circumference >88 cm; HDL-cholesterol <1.3 mmol/L; serum triglycerides ≥1.7 mmol/L; blood pressure ≥130/85 mmHg; fasting glucose ≥5.6 mmol/L. These, the ATP-III criteria have been used in previous studies from our group on this cohort of women and are also in line with the current consensus criteria recommended by the World Health Organisation (WHO) [26].
SPSS version 19 (IBM, New York, NY) was used for statistical analysis. Differences between sample proportions were determined using the chi-square test, and differences between continuous variables were determined using the unpaired two-tailed t test (parametric) or Kolmogorov–Smirnov test (non-parametric). The Bonett–Price method was used to estimate confidence intervals for the difference between sample medians.
Results
Of 270 women with previous GDM, 265 had sufficient data available to make or exclude a diagnosis of metabolic syndrome, while of 388 with NGT in pregnancy, 378 had sufficient data to make or exclude a diagnosis of metabolic syndrome. Baseline characteristics for these participants are shown in Table 1.
Metabolic syndrome
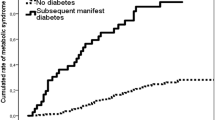
Metabolic syndrome by ATP-III criteria was present in 25.3 % of women with previous GDM at a mean of 2.6 years post index pregnancy, compared with 6.6 % of women with NGT in pregnancy (p < 0.001), despite a longer time lapse since the index pregnancy in NGT women (3.3 years in the NGT group; Table 2). The prevalence of each component of metabolic syndrome by glucose status in the index pregnancy (NGT and GDM) is shown in Fig. 1. Waist circumference of greater than 88 cm was the most common metabolic syndrome criterion present in both groups, with 55 % of women with previous GDM and 31 % of women with NGT meeting the criterion, and also showed (analysed as a continuous variable) the strongest individual correlation (correlation coefficient 0.523) with a diagnosis of metabolic syndrome. After adjustment for obesity, an excess of risk for metabolic syndrome in women with previous GDM remains evident. Among obese women, those with IADPSG-defined GDM had an odds ratio (OR) of 3.9 (95 % CI 2.0, 7.9, p < 0.01) for a diagnosis of metabolic syndrome by ATP-III criteria (prevalence 54.7 vs. 23.4 %, p < 0.001) compared to obese women with previous NGT in pregnancy (Fig. 2). However, the prevalence of metabolic syndrome was similar in non-obese women in both groups (5.7 vs. 3.2 %, p = 0.15), with an OR of 1.8 (95 % CI 0.7, 4.6, p = 0.20).
Prevalence of metabolic syndrome (ATP-III criteria), obesity (BMI > 30 kg/m2), and insulin resistance (HOMA2-IR >1.8) by glycaemic status during index pregnancy. Figures represent percentages, p < 0.001 between groups for all characteristics. GDM gestational diabetes by IADPSG criteria, NGT normal glucose tolerance by IADPSG criteria
Insulin resistance and beta-cell function
Insulin resistance data were available for 256 women (97 % of cohort) with previous GDM and 363 women (94 % of cohort) with NGT in pregnancy. The median HOMA2-IR (Table 2) differed significantly between the groups—0.9 in women with NGT compared to 1.4 in women with previous GDM (p < 0.001). Beta-cell function (HOMAB%), as measured using the HOMA-2IR computer model (Table 2), did not differ significantly between the two groups (median 144 % in women with previous GDM vs. 139 % in women with NGT in pregnancy, p = 0.11). The prevalence of HOMA2-IR >1.8 (Table 2; Fig. 2) in this population was 33.6 % in women with previous GDM, compared to 9.1 % in women with previous NGT in pregnancy [p < 0.01, OR 5.1 (95 % CI 3.6, 7.9)]. The log transformation (carried out due to a non-normal distribution) of HOMA2-IR also correlated significantly (r = 0.520, p < 0.01) with a diagnosis of metabolic syndrome.
Metabolic features during index pregnancy
Weight gain following the index pregnancy has been identified as a significant contributor to increased risk of progression to diabetes following GDM on longer-term follow-up [27]. We do not have data on maternal weight prior to the index pregnancy, or complete data on BMI during the index pregnancy for the total cohort. However, 90 % of our previous GDM cohort had a weight available from the index pregnancy, and 84 % of our NGT cohort had a weight available from the index pregnancy (at mean 27 weeks vs. at 26 weeks gestation, respectively, p = 0.001). Based on this subset, BMI during pregnancy was 31.4 kg/m2 in women with GDM versus 27.0 kg/m2 in women with NGT (p < 0.001). Interestingly, there was no significant difference in the magnitude of weight change between the index pregnancy and retesting; women with previous GDM lost a median of 3.8 kg (interquartile range −10.3 to 1.0 kg) while women with NGT lost a median of 2.6 kg (interquartile range −6.3 to 1.0 kg, p = 0.15, 95 % CI for difference −0.26, 2.64). There was no difference in the proportion of women who had gained weight since the index pregnancy between groups (30.4 % GDM vs. 32.9 % NGT, p = 0.30), or in the proportion of women who had gained over 5 kg since the index pregnancy (12.1 % GDM vs. 11.9 % NGT, p = 0.52).
Of note, women who did not attend for this study, but who underwent universal screening in the index pregnancy, and met IADPSG criteria for GDM, were slightly younger at delivery [mean age 33.1 years (SD 5.7) vs. 34.0 years (SD 4.9) p = 0.046], while their BMI did not differ from women who attended [31.1 kg/m2 (SD 6.5), vs. 31.4 kg/m2 (SD 6.6), p = 0.611].
Comparison of women identified by universal or risk-factor-based testing
Given that the risk factors for metabolic syndrome and the risk factors used to select women for GDM testing show considerable overlap, we undertook a stratified analysis of those women identified by risk-factor-based screening and those identified during universal screening. Of the 265 women with IADPSG-defined GDM, 194 (73 %) were identified during the universal screening period. One hundred and seventy-seven (91 %) of these had at least one criterion for risk-factor-based screening, as compared with 80 % of women with NGT (p < 0.01). The prevalence of each risk factor for among women with GDM as compared with those with NGT is shown in Table 3. Women with GDM showed a significantly higher prevalence of a family history of diabetes in a first-degree relative (41.1 vs. 26.5 % in women with NGT, p < 0.01); BMI ≥30 kg/m2 at the time of testing for GDM (83.2 vs. 64.2 %, p < 0.01); and a history of having delivered a previous baby weighing ≥4.5 kg (17.7 vs. 11.9 %, p = 0.04). Women with IADPSG-defined GDM identified during universal screening did not differ from those identified by risk-factor-based screening in either prevalence of ATP-III-defined metabolic syndrome (26.3 vs. 22.4 %, p = 0.63), or in prevalence of HOMA2-IR >1.8 (34.7 vs. 30.2 %, p = 0.54).
In order to adjust for the effect of risk-factor-based screening, we examined the prevalence of ATP-III-defined metabolic syndrome; its individual components; and HOMA-IR >1.8, in women with IADPSG-defined GDM identified during the universal screening phase. The prevalence of ATP-III-defined metabolic syndrome was 26.3 % in women with GDM versus 6.3 % those with NGT (p < 0.01). Women with IADPSG-defined GDM also showed a higher prevalence of each of the individual components of ATP-III-defined metabolic syndrome; waist circumference >88 cm (53.5 vs. 31.4 %, p < 0.01); fasting glucose ≥5.6 mmol/L (16.2 vs. 1.9 %, p < 0.01); serum triglycerides ≥1.7 mmol/L (19.7 vs. 5.5 %, p < 0.01); HDL-cholesterol <1.3 mmol/L (30.3 vs. 14.6 %, p < 0.01); blood pressure ≥130/85 mmHg (39.9 vs. 15.4 %), and a higher prevalence of HOMA2-IR >1.8 (34.7 vs. 9.2 %). When the figures from women identified during the universal screening programme are compared with the those of the entire cohort (as seen in Figs. 1, 2), no difference is seen for a diagnosis of ATP-III-defined metabolic syndrome (p = 0.83); any of the individual components of metabolic syndrome (waist circumference; p = 0.85, fasting glucose; p = 0.80; triglycerides; p = 0.91; blood pressure, p = 0.85; HDL-cholesterol, p = 0.69); or prevalence of HOMA2-IR >1.8 (p = 1.0).
Discussion
Our results show that despite using the less stringent IADPSG criteria for GDM diagnosis, GDM continues to define a high-risk cohort of women at markedly increased future risk of metabolic syndrome, with 25.3 % meeting diagnostic criteria (ATP-III) at a mean of 2.6 years post-partum; a prevalence 3 times greater than that observed in women with NGT during pregnancy. The prevalence of metabolic syndrome and insulin resistance does not differ significantly whether women are identified by risk-factor-based screening, or whether universal screening is employed.
Other studies have examined the prevalence of metabolic syndrome, at varying intervals post-partum, and with older GDM diagnostic criteria. Retnakaran et al. [28] examined women with previous GDM at 3 months post-partum and found an almost twofold increased prevalence (17 %) when compared to a control population with NGT in pregnancy (9 %). Lauenborg et al. [3] also showed a threefold increased prevalence of metabolic syndrome at almost 10 years post-partum in women with diet-treated GDM (44 %) versus women with NGT (15 %). Despite the significantly shorter time elapsed since the index pregnancy (2.6 years) in our IADPSG-defined GDM cohort, and the use of the generally more conservative ATP-III criteria, we find both a greater than threefold elevation of metabolic syndrome in women with prior GDM compared to NGT matched controls and a high absolute prevalence of metabolic syndrome, with over 25 % of women with previous GDM affected. This is particularly concerning in a population of young women belonging to what has previously been considered a lower-risk ethnic group for the development of metabolic syndrome [29].
The figures for insulin resistance are also a source of concern. HOMA-IR has been correlated with earlier beta-cell deterioration in the early post-partum period [30]. Xiang et al. [27] also demonstrated, using detailed physiological techniques (frequently sampled intravenous glucose tolerance test and the hyperinsulinaemic–euglycaemic clamp) in a longitudinal study with up to 12-year follow-up, that lower insulin sensitivity and lower beta-cell compensation for insulin resistance at the baseline assessment were associated with progression to diabetes over the study period. With over one-third of our cohort of women with previous GDM by IADPSG criteria displaying values indicative of insulin resistance, this has potentially serious long-term consequences, both for the individual women and the health services that must plan for their future care.
This effect cannot be entirely explained by obesity alone, although the prevalence of obesity is significantly higher in women with previous GDM (see Fig. 2). Obesity confers a significant excess risk of metabolic syndrome in this cohort, but the prevalence of metabolic syndrome still remains double that observed in obese women with previous NGT in pregnancy. This finding is in keeping with recent data from Buchanan et al. [31], showing that insulin sensitivity declined faster in women with previous GDM compared to NGT women, despite no difference in weight change.
Our study has some important limitations. We are unable to compare the full demographic or metabolic characteristics of this cohort with those of women who did not attend for testing, either in the index pregnancy, or for participation in this study. We are also unable to characterise fully the metabolic characteristics of this cohort before the index pregnancy, although data on weight measurements in the index pregnancy were available for the majority of our cohort, and show no significant difference between the groups.
Notwithstanding these limitations, our results demonstrate a significant and clinically relevant difference in metabolic risk factors between the two groups. Over one in four women with previous IADPSG-defined GDM meet the diagnostic criteria for metabolic syndrome, while one in three women with previous IADPSG-defined GDM demonstrate biochemical evidence of insulin resistance. This is despite the IADPSG criteria defining what one would assume to be a lower-risk population, due to the lower thresholds and single abnormal value required for diagnosis, and despite these women still being of reproductive age (mean 36.7 years, SD 5.0 years). The high prevalence of risk factors associated with both GDM and metabolic syndrome in the index pregnancy, particularly the high prevalence of obesity, indicates that interventions aimed at reducing the future consequences of GDM should begin before the diagnosis of GDM is made. Efforts focused on lifestyle modification in these high-risk women, in both the preconception and post-partum periods, are necessary to try to ameliorate the excess future risk of diabetes, cardiovascular disease, and excess mortality associated with such an adverse metabolic profile.
References
Bellamy L, Casas JP, Hingorani AD, Williams D (2009) Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. The Lancet 373(9677):1773–1779
Shah BR, Retnakaran R, Booth GL (2008) Increased risk of cardiovascular disease in young women following gestational diabetes mellitus. Diabetes Care 31(8):1668–1669. doi:10.2337/dc08-0706
Lauenborg J, Mathiesen E, Hansen T, Glumer C, Jorgensen T, Borch-Johnsen K, Hornnes P, Pedersen O, Damm P (2005) The prevalence of the metabolic syndrome in a Danish population of women with previous gestational diabetes mellitus is three-fold higher than in the general population. J Clin Endocrinol Metab 90(7):4004–4010. doi:10.1210/jc.2004-1713
O’Sullivan JB, Mahan CM (1964) Criteria for the oral glucose tolerance test in pregnancy. Diabetes 13:278–285
National Diabetes Data Group (1979) Classification and diagnosis of diabetes mellitus and other categories of glucose intolerance. Diabetes 28(12):1039–1057
Carpenter MW, Coustan DR (1982) Criteria for screening tests for gestational diabetes. Am J Obstet Gynecol 144(7):768–773
O’Sullivan JB (1991) Diabetes mellitus after GDM. Diabetes 40(Suppl 2):131–135
WHO Expert Committee on Diabetes Mellitus (1980) Second report. World Health Organ Tech Rep Ser, vol 646, 1980/01/01 edn
World Health Organisation (1999) Definition, diagnosis, and classification of diabetes and its complications. Part 1: diagnosis and classification of diabetes mellitus. World Health Organisation, Geneva
Metzger BE, Gabbe SG, Persson B, Buchanan TA, Catalano PA, Damm P, Dyer AR, Leiva A, Hod M, Kitzmiler JL, Lowe LP, McIntyre HD, Oats JJ, Omori Y, Schmidt MI (2010) International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 33(3):676–682. doi:10.2337/dc09-1848
Sacks DA, Hadden DR, Maresh M, Deerochanawong C, Dyer AR, Metzger BE, Lowe LP, Coustan DR, Hod M, Oats JJ, Persson B, Trimble ER (2012) Frequency of gestational diabetes mellitus at collaborating centers based on IADPSG consensus panel-recommended criteria: the hyperglycemia and adverse pregnancy outcome (HAPO) study. Diabetes Care 35(3):526–528. doi:10.2337/dc11-1641
American Diabetes Association (2011) Standards of medical care in diabetes. Diabetes Care 34(Suppl 1):S11–S61. doi:10.2337/dc11-S011
WHO (2013) Diagnostic criteria and classification of hyperglycaemia first detected in pregnancy. World Health Organisation, Geneva
Kahn R, Buse J, Ferrannini E, Stern M (2005) The metabolic syndrome: time for a critical appraisal: joint statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 28(9):2289–2304
Ford ES, Li C, Sattar N (2008) Metabolic syndrome and incident diabetes: current state of the evidence. Diabetes Care 31(9):1898–1904. doi:10.2337/dc08-0423
Ford ES (2005) Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: a summary of the evidence. Diabetes Care 28(7):1769–1778
O’Reilly MW, Avalos G, Dennedy MC, O’Sullivan EP, Dunne F (2011) Atlantic DIP: high prevalence of abnormal glucose tolerance post partum is reduced by breast-feeding in women with prior gestational diabetes mellitus. Eur J Endocrinol 165(6):953–959. doi:10.1530/EJE-11-0663
Noctor E, Crowe C, Carmody LA, Avalos GM, Kirwan B, Infanti JJ, O’Dea A, Gillespie P, Newell J, McGuire B, O’Neill C, O’Shea PM, Dunne FP (2013) ATLANTIC DIP: simplifying the follow-up of women with previous gestational diabetes. Eur J Endocrinol 169(5):681–687. doi:10.1530/EJE-13-0491
O’Sullivan EP, Avalos G, O’Reilly M, Dennedy MC, Gaffney G, Dunne F (2011) Atlantic diabetes in pregnancy (DIP): the prevalence and outcomes of gestational diabetes mellitus using new diagnostic criteria. Diabetologia 54(7):1670–1675. doi:10.1007/s00125-011-2150-4
Wallace TM, Levy JC, Matthews DR (2004) Use and abuse of HOMA modeling. Diabetes Care 27(6):1487–1495
Geloneze B, Vasques AC, Stabe CF, Pareja JC, Rosado LE, Queiroz EC, Tambascia MA, Investigators B (2009) HOMA1-IR and HOMA2-IR indexes in identifying insulin resistance and metabolic syndrome: Brazilian Metabolic Syndrome Study (BRAMS). Arq Bras Endocrinol Metabol 53(2):281–287
Mojiminiyi OA, Abdella NA (2010) Effect of homeostasis model assessment computational method on the definition and associations of insulin resistance. Clin Chem Lab Med 48(11):1629–1634. doi:10.1515/CCLM.2010.303
Radikova Z, Koska J, Huckova M, Ksinantova L, Imrich R, Vigas M, Trnovec T, Langer P, Sebokova E, Klimes I (2006) Insulin sensitivity indices: a proposal of cut-off points for simple identification of insulin-resistant subjects. Exp Clin Endocrinol Diabetes 114(5):249–256. doi:10.1055/s-2006-924233
Ascaso JF, Pardo S, Real JT, Lorente RI, Priego A, Carmena R (2003) Diagnosing insulin resistance by simple quantitative methods in subjects with normal glucose metabolism. Diabetes Care 26(12):3320–3325
Safar FH, Mojiminiyi OA, Al-Rumaih HM, Diejomaoh MF (2011) Computational methods are significant determinants of the associations and definitions of insulin resistance using the homeostasis model assessment in women of reproductive age. Clin Chem 57(2):279–285. doi:10.1373/clinchem.2010.152025
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC Jr (2009) Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120(16):1640–1645. doi:10.1161/CIRCULATIONAHA.109.192644
Xiang AH, Kjos SL, Takayanagi M, Trigo E, Buchanan TA (2010) Detailed physiological characterization of the development of type 2 diabetes in Hispanic women with prior gestational diabetes mellitus. Diabetes 59(10):2625–2630. doi:10.2337/db10-0521
Retnakaran R, Qi Y, Connelly PW, Sermer M, Zinman B, Hanley AJ (2010) Glucose intolerance in pregnancy and postpartum risk of metabolic syndrome in young women. J Clin Endocrinol Metab 95(2):670–677. doi:10.1210/jc.2009-1990
Kousta E, Efstathiadou Z, Lawrence NJ, Jeffs JA, Godsland IF, Barrett SC, Dore CJ, Penny A, Anyaoku V, Millauer BA, Cela E, Robinson S, McCarthy MI, Johnston DG (2006) The impact of ethnicity on glucose regulation and the metabolic syndrome following gestational diabetes. Diabetologia 49(1):36–40. doi:10.1007/s00125-005-0058-6
Retnakaran R, Qi Y, Ye C, Hanley AJ, Connelly PW, Sermer M, Zinman B (2011) Hepatic insulin resistance is an early determinant of declining beta-cell function in the first year postpartum after glucose intolerance in pregnancy. Diabetes Care 34(11):2431–2434. doi:10.2337/dc11-0817
Xiang AH, Takayanagi M, Black MH, Trigo E, Lawrence JM, Watanabe RM, Buchanan TA (2013) Longitudinal changes in insulin sensitivity and beta cell function between women with and without a history of gestational diabetes mellitus. Diabetologia 56(12):2753–2760. doi:10.1007/s00125-013-3048-0
Acknowledgments
Funding for the study was provided by the Health Research Board (HRB) of Ireland. E.N. reports receiving an unrestricted educational grant from Novo Nordisk Ireland Ltd.
Conflict of interest
C.C., L.C., B.K., A.O.D., L.G., B.M.G., P.O.S., and F.D. have nothing to declare. E.N. reports receiving an unrestricted educational grant from Novo Nordisk Ireland Ltd. for this study.
Ethical standard
This study involved human participants and was approved by the ethics committees of the relevant institutions and conducted in accordance with the principles laid out in the 1964 Helsinki declaration.
Human and animal rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Informed consent
All participants gave informed consent for participation in this study.
ATLANTIC-DIP collaborators
Dr. Geraldine Gaffney, University Hospital Galway, Dr. Maeve Durkan, Portiuncula Hospital, Co. Galway, Dr. Murtada Mohammed, Mayo General Hospital, Dr. Nandini Ravikumar, and Ms. Therese Gallacher, Letterkenny General Hospital.
Author information
Authors and Affiliations
Corresponding author
Additional information
Managed by Massimo Porta.
For the ATLANTIC-DIP investigators.
Rights and permissions
About this article
Cite this article
Noctor, E., Crowe, C., Carmody, L.A. et al. ATLANTIC-DIP: prevalence of metabolic syndrome and insulin resistance in women with previous gestational diabetes mellitus by International Association of Diabetes in Pregnancy Study Groups criteria. Acta Diabetol 52, 153–160 (2015). https://doi.org/10.1007/s00592-014-0621-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-014-0621-z