Abstract
Ectopic accumulation of lipids in nonadipose tissues plays a primary role in the pathogenesis of type 2 diabetes mellitus (T2DM). This study was to examine the effects of exenatide, insulin, and pioglitazone on liver fat content and body fat distributions in T2DM. Thirty-three drug-naive T2DM patients (age 52.7 ± 1.7 years, HbA1c 8.7 ± 0.2 %, body mass index 24.5 ± 0.5 kg/m2) were randomized into exenatide, insulin, or pioglitazone for 6 months. Intrahepatic fat (IHF), visceral fat (VF), and subcutaneous fat (SF) were measured using proton nuclear magnetic resonance spectroscopy. Plasma tumor necrosis factor α (TNFα) and adiponectin were assayed by ELISA. HbA1c declined significantly in all three groups. Body weight, waist, and serum triglycerides decreased with exenatide. After interventions, IHF significantly reduced with three treatments (exenatide Δ = −68 %, insulin Δ = −58 %, pioglitazone Δ = −49 %). Exenatide reduced VF (Δ = −36 %) and SF (Δ = −13 %), and pioglitazone decreased VF (Δ = −30 %) with no impact on SF, whereas insulin had no impact on VF or SF. Levels of TNFα (exenatide/insulin/pioglitazone) decreased, and levels of adiponectin (exenatide/pioglitazone) increased. Analysis showed that ΔIHF correlated with ΔHbA1c and Δweight. Besides, ΔIHF correlated with Δtriglycerides and ΔTNFα, but the correlations fell short of significance after BMI adjustment. By linear regression analysis, ΔHbA1c alone explained 41.5 % of the variance of ΔIHF, and ΔHbA1c + Δweight explained 57.6 % of the variance. Liver fat content can be significantly reduced irrespective of using exenatide, insulin, and pioglitazone. Early glycaemic control plays an important role in slowing progression of fatty liver in T2DM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lipotoxicity, that is ectopic accumulation of lipids in nonadipose tissues of liver and skeletal muscle, plays a primary role in the pathogenesis of obesity-associated insulin resistance and type 2 diabetes mellitus (T2DM) [1, 2]. Thus, early treatment with agents that blunt both of the deleterious processes of glucotoxicity and lipotoxicity is the preferred anti-diabetic strategies for metabolic control and reducing the risk for micro- and macrovascular complications in T2DM.
Among the common anti-diabetic agents, the glucagon-like peptide-1 (GLP-1) receptor agonists and peroxisome proliferator-activated receptor-γ (PPAR-γ) agonists may affect the distribution of fat mass in a positive manner. Clinical studies have demonstrated that GLP-1 receptor agonists (exenatide and liraglutide) are associated with a reduction in body weight, a decrease in visceral and hepatic fat depots, and an improvement of overall and hepatic insulin sensitivity in obese patients with T2DM [3–6]. As for PPAR-γ agonists (pioglitazone and rosiglitazone), they usually cause weight gain [7]. Nevertheless, pioglitazone treatment can also reduce liver fat content and enhance peripheral tissue glucose uptake [8]. In addition, insulin is commonly used to in clinical practice to improve glycaemic control. We previously have shown that short-term intensive insulin therapy in newly diagnosed T2DM improves β-cell function, restores insulin sensitivity, and ameliorates lipid profiles, leading to long-term glycaemic remission [9, 10]. Some, but not all [11], studies further demonstrated a reduction in liver fat content in association with improved hepatic insulin sensitivity after 7 months of insulin treatment in obese patients with T2DM [12]. However, as the current literature lacks randomized parallel-group intervention study, still unclear is whether these beneficial effects are due to either the agent itself or the effects of simply eliminating glucotoxicity by achieving glycaemic control, and whether these effects differ between agents.
We therefore compared the effects of exenatide, insulin, and pioglitazone therapies on body fat distributions with a prospective, randomized, parallel-group study, and to investigate the contributing factors responsible for the changes in body fat distributions after three treatments. Proton nuclear magnetic resonance spectroscopy (1H-MRS) was used to noninvasively quantify intrahepatic fat (IHF), visceral fat (VF), and subcutaneous fat (SF) contents in all subjects.
Methods
Participants
Thirty-three patients with T2DM from Drum Tower Hospital according to World Health Organization diagnostic criteria [13] were a subset of the multicenter study of 342 patients with the primary endpoint to compare the glycaemic efficacy of exenatide, insulin, and pioglitazone (ClinicalTrials.gov, NCT01147627) [14]. They were 52.7 ± 1.7 years of age, with a BMI of 24.5 ± 0.5 kg/m2, HbA1c 8.7 ± 0.2 %, and negative for glutamic acid decarboxylase antibody, and had not received antihyperglycemic therapy. Exclusion criteria included acute or severe chronic diabetic complications, impaired renal function (serum creatinine ≥133 μmol/L), and liver dysfunction (aspartate aminotransferase (AST) or alanine aminotransferase (ALT) levels more than 2.5 times the normal value), taking medications known to affect weight, a history of severe gastrointestinal disease such as pancreatitis. The protocol and informed consent document were approved by the research ethics board of Drum Tower hospital affiliated to Nanjing University Medical School. Informed consent was obtained from all patients for being included in the study.
Intervention study design
After a screening diet/exercise run-in period of 1 week, patients were randomized into one of three treatments for 6 m: exenatide, insulin humalog Mix25, and pioglitazone. For participants assigned to exenatide, the initial dose was 5 μg twice daily and titrated to a maximum 10 μg twice daily at week 4 and maintained throughout the course of the trial. For humalog Mix25, the starting doses were 0.4 IU/kg d twice daily and then gradually uptitrated aiming for glucose values of 4.4–7.0 mmol/L before breakfast and dinner. For pioglitazone, the initial dose was 30 mg daily and titrated to 45 mg daily at week 4 if tolerated and maintained during the intervention period. In the event of significant hypoglycemia (<3.9 mmol/L), frequent nausea, or vomiting, interventions were sequentially backtitrated. Patients who could not stand the side effects of hypoglycemic agents were withdrawn from the trial. All subjects underwent a standard meal tolerance test using the 85-g carbohydrate equivalent ingested within 10 min at baseline and at the end of therapy. Blood was collected at 0, 30, and 120 min from the meal start for the measurement of plasma glucose and insulin. Insulin sensitivity was assessed by homeostasis model assessment of insulin sensitivity (1/HOMA-IR) and the Matsuda insulin sensitivity index (ISIM) [15–17].
1H-MRS
1H-MRS studies were performed on a 3.0 T system (Philips Medical Systems). Subjects were asked to avoid moderate physical activity, vigorous exercise, or high-fat diet 72 h prior to scanning. In liver, MRS studies were performed with an automated single-voxel MRS point-resolved spectroscopy pulse sequence. One 8 cm3 voxel was localized on the survey T1-weighted image at right posterior hepatic lobe and adjusted to avoid visible vascular structures. Signal amplitude of lipid and H2O was used to calculate the relative IHF content by the formula of intrahepatic lipid (%) = [lipid/(H2O + lipid)] × 100 [18, 19].
Dual echo with fast-field echo sequence
For VF and SF, a series of in-phase imaging for determination of VF and SF areas were acquired from a region extending from 4 cm above to 4 cm below the fourth and fifth lumbar interspace. The area of VF and SF was determined from histograms specific to the visceral and subregion. The histograms were summed over the range of pixel values designated as fat [20]. The areas of VF and SF from each slice were summed for comparison. All the assessments were undertaken in a blinded fashion to the assessor in the nature of treatment.
Measurements
HbA1c was measured using high-performance liquid chromatography (Tosoh Bioscience, Japan). Insulin was tested by chemiluminescence immunoassay (Roche, USA). Serum levels of glucose, total cholesterol, triglyceride, low-density lipoprotein (LDL) cholesterol, ALT, and AST were measured by enzymatic methods with the use of an autoanalyzer (TBA-200FR, Tokyo, Japan). Adiponectin (R&D systems, USA) and tumor necrosis factor α (TNFα, ExCell, China) were determined by ELISA kits.
Statistical analyses
Statistical analyses were performed using SPSS version 15.0 program (Chicago, IL). For the assessment of differences between the treatment groups with regard to quantitative variables, one-way analysis of variance (ANOVA) was used. The comparisons for potential confounders were made using an ANCOVA model with treatment as fixed effects and baseline measure, age, gender, and body weight as the covariates where appropriate. Pearson's correlation analysis was used when applicable to examine bivariate relationships. Stepwise multiple linear regression analysis was used to examine the contributions of potential risk variants to the reduction in IHF after treatments. Data are presented as mean ± SE. A p value of <0.05 was considered statistically significant.
Results
Clinical parameters
After 24 weeks of treatment, HbA1c was significantly reduced to a similar extent among three groups (exenatide Δ = −2.9 ± 0.4 % vs. insulin Δ = −2.8 ± 0.3 % vs. pioglitazone Δ = −2.0 ± 0.4 %, P = 0.158). Body weight (Δ = −5.0 kg, P = 0.002), waist (Δ = −5.1 cm, P = 0.037), triglycerides (Δ = −19.1 ± 11.0 %, P = 0.03), and ALT (Δ = −34.0 ± 13.5 %, P = 0.043) significantly decreased with exenatide but did not change with insulin and pioglitazone. Total cholesterol (Δ = −12.8 ± 4.7 %, P = 0.023) decreased in exenatide and insulin (Δ = −9.1 ± 5.4 %, P = 0.027) but not in pioglitazone. LDL cholesterol and AST did not change in any group. Exenatide and pioglitazone markedly increased insulin sensitivity as indicated in ISIM (exenatide: Δ = 99.2 ± 34.6 %, P = 0.004; pioglitazone: Δ = 32.9 ± 20.0 %, P = 0.003) and 1/HOMA-IR (exenatide: Δ = 148.2 ± 53.3 %, P = 0.007; pioglitazone: Δ = 41.6 ± 19.5 %, P = 0.001), whereas insulin did not (Table 1).
Treatment effects on IHF, VF, and SF contents
Thirty-three patients had baseline IHF, VF, and SF of 23.5 ± 2.8 %, 130.8 ± 11.0 cm2, and 107.1 ± 10.5 cm2, respectively, and there were no significant differences in baseline IHF, VF, and SF among three groups (P = 0.506, 0.207, 0.715, respectively).
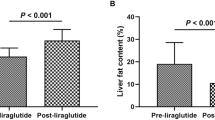
After interventions, three treatments resulted in a statistically significant reduction in IHF: exenatide from 27.4 ± 5.5 % to 6.3 ± 1.4 %, Δ = −68 ± 6 %, P = 0.004; insulin from 23.7 ± 5.0 % to 9.1 ± 2.9 %, Δ = −58 ± 9 %, P = 0.012; pioglitazone from 20.2 ± 4.2 % to 8.0 ± 2.6 %, Δ = −49 ± 9 %, P = 0.039. The reduction in IHF did not differ between three groups (P = 0.454) (Fig. 1).
Effects of exenatide, insulin, or pioglitazone treatments on IHF, VF, and SF. a IHF, VF, and SF at baseline and after treatment in three groups. b The relative changes in IHF, VF, and SF after treatments. White bars pretreatment, black bars posttreatment. *P < 0.05 compared with pretreatment. Values are mean ± SE
Exenatide and pioglitazone markedly declined VF (exenatide from 159.3 ± 14.4 cm2 to 104.1 ± 16.0 cm2, Δ = −36 ± 6 %, P < 0.001; pioglitazone from 112.7 ± 18.8 cm2 to 80.0 ± 17.3 cm2, Δ = −30 ± 7 %, P = 0.003), but insulin did not. Exenatide also decreased SF (from 108.5 ± 19.6 cm2 to 85.8 ± 18.1 cm2, Δ = −13 ± 9 %, P = 0.006), while insulin and pioglitazone did not (Fig. 1).
Inflammatory biomarkers
Three treatments significantly decreased plasma TNFα levels (exenatide Δ = −62 ± 19 %, P = 0.012; insulin Δ = −60 ± 17 %, P = 0.002; pioglitazone Δ = −42 ± 25 %, P = 0.001). Plasma adiponectin levels (exenatide Δ = 118 ± 24 %, P = 0.008; pioglitazone Δ = 207 ± 38 %, P < 0.001) were significantly increased with exenatide and pioglitazone, but not with insulin (Table 1). No significant effect of any treatment on circulating levels of IL-1β or IL-6 was observed.
Correlative analysis
HbA1c reduction
There was a significant correlation between ΔHbA1c and ΔIHF in the entire subjects both before and after BMI adjustment (Table 2; Fig. 2a).
Correlations between changes in IHF and HbA1c reduction and weight loss after treatments with exenatide, insulin, or pioglitazone. a Correlations between changes in IHF and HbA1c reduction. b Correlations between changes in IHF and weight loss. c Changes in relative reduction in IHF according to weight loss <5 and ≥5 %. Black circles exenatide, white circles insulin, black triangles pioglitazone
Weight loss
There was a significant correlation between weight reduction and ΔIHF after intervention (Table 2; Fig. 2b). To reinforce the contributions of weight loss on changes in IHF, we divided patients into two subgroups according to amount of weight loss of <5 % (n = 20, mean weight change of 0.3 ± 0.6 kg) and ≥5 % (n = 13, mean weight change of −6.3 ± 0.6 kg). The reduction of IHF in those patients who achieved marked weight loss were significantly greater than those with less weight loss (−41.4 ± 10.6 % vs. −83.3 ± 2.5 %, P = 0.001) (Fig. 2c).
Serum triglycerides reduction
There was a significant relationship between the relative reduction in serum triglycerides and ΔIHF before BMI adjustment (r = 0.407, P = 0.019), but it fell short of statistical significance after BMI adjustment (r = 0.309, P = 0.085) (Table 2).
Inflammatory biomarkers
The relative ΔTNFα was associated with the relative ΔIHF before BMI adjustment, but the correlation fell short of significance after BMI adjustment. No significant correlation between Δadiponectin and ΔIHF was shown before and after BMI adjustment (Table 2).
ΔVF
There was a significant correlation between ΔIHF and ΔVF before BMI adjustment, but it fell short of significance after BMI adjustment (Table 2).
Baseline IHF
Additionally, there was a significant and negative correlation between baseline IHF and relative ΔIHF with all three treatments (Table 2).
Multiple regression analysis
Using ΔIHF as the independent variable, and ΔHbA1c, Δweight, Δtriglycerides, baseline IHF, ΔVF, and ΔTNFα as the dependent variables, we found that ΔHbA1c and Δweight entered into the equation: ΔHbA1c alone explained 41.5 % of the variance of ΔIHF, and ΔHbA1c + Δweight explained 57.6 % of the variance (Table 3).
Discussion
This analysis represents the first systematic and comparative evaluation of changes in IHF, and body fat distributions in patients with T2DM randomized into exenatide, insulin, or pioglitazone monotherapy, especially in the absence of the confounding effects of any other anti-diabetic medications. Of note, the important finding of this study is that IHF content could be similarly reduced after 6 month of treatment with exenatide, insulin, or pioglitazone intervention. Also, treatment with exenatide significantly reduced VF and SF contents, and pioglitazone decreased VF but had minimal impact on SF, whereas insulin had no impact on VF and SF distributions.
Although studies support the idea that diabetes is a high risk for the development of nonalcoholic fatty liver that progresses in parallel to glucose dysregulation [21], the question remains of whether anti-diabetic therapies might gain additional benefits on reducing fat deposition in the liver beyond the effects on glucose control. Previous studies have shown that anti-diabetic agents of exenatide, insulin, or pioglitazone could improve glucose control and concomitantly decline hepatic fat by 20–60 % [3–8, 11, 22]. However, those reports were placebo-controlled studies, whether the beneficial effects on IHF are indirect as a result of their ability to improve glycemia or the result from the agent itself cannot be analyzed before this study. Consistent with the results of those studies, we demonstrated a reduction in IHF of 68, 58, and 49 %, respectively, following exenatide, insulin, and pioglitazone treatment. Furthermore, we observed a close relationship between ΔHbA1c and ΔIHF, and ΔHbA1c explained 41.5 % of the ΔIHF, suggesting that alleviation of glucose toxicity is crucial to the reduction in IHF with three medications.
Another question arises from our results: to what extent is reduction in liver fat explained by weight loss with all three treatments? Our data showed that the changes in IHF correlated with weight loss following therapies. A greater reduction in IHF was achieved in patients with ≥5 % weight loss (mean weight change of −6.3 kg) than that in patients with <5 % weight loss, and Δweight loss explained 16.1 % of the ΔIHF after the contribution of ΔHbA1c to ΔIHF, indicating that weight loss has an additional effect on the decrease in hepatic fat. This is in line with previous observations demonstrating that hepatic steatosis was significantly reduced with exenatide, lifestyle, or dietary intervention when a similar reduction in body weight was achieved as we observed [5, 23–25]. Importantly, the reductions in IHF in those patients who achieved marked weight loss in insulin and pioglitazone were very similar to those in exenatide, indicating that the beneficial effect of weight loss on IHF apply to all the treatments, but it needs to be examined in future studies.
Chronic inflammatory states are associated with the development of nonalcoholic fatty liver and type 2 diabetes, in which circulating inflammatory cytokines are considered to be the major biochemical mediators [26, 27], and also hyperglycemia is a critical component in the sub-inflammatory status, beyond insulin resistance and obesity [28]. Previous studies indicated that plasma levels of TNFα positively correlated with the degree of liver fibrosis when assessed by the ultrasound-guided liver biopsy [29]. Consistent with these observations, we found that decreased TNFα was associated with the reduced IHF with all three treatments. Nonetheless, after BMI adjustment, the correlation between the change in TNFα and IHF fell short of statistical significance, supporting TNFα as a mechanistic link to obesity-associated hepatic steatosis.
Nonalcoholic fatty liver is associated with increased levels of serum triglycerides, independent of visceral adipose tissue and other obesity measures [30]. Aggressive treatment of hypertriglyceridemia with different agents led to inconsistent effects on fatty liver, in which fenofibrate had minimal effects on liver histology [31] while omega-3 fatty acids supplementation was associated with improvement of hepatic steatosis in patients with nonalcoholic fatty liver disease [32]. In this study, we found that improvement in serum triglycerides was associated with reduction in IHF but it fell short of significance after BMI adjustment, indicating that serum triglycerides may be a link to the development of fatty liver associated with obesity in T2DM.
In this study, we enrolled nonobese Chinese subjects while most of previous studies examining the effects of anti-diabetic agents on lipid partitioning were investigated in obese patients with T2DM. Nonetheless, we found that our patients had a relatively higher amount of baseline IHF with relatively lower BMI (IHF of 23.5 % with BMI of 24.5 kg/m2) in comparison to a study from obese Europeans that had an IHF of 28 % with BMI of 38.4 kg/m2 [5]. Albeit the quantification of IHF may differ in varying degree across studies, this predisposition is consistent with previous data. As highlighted earlier, multiethnic studies showed that Asians including Chinese have greater adiposity than Caucasian subjects [33], and were more insulin resistant than other ethnic groups [34, 35]. Thus, effects of current anti-diabetic treatments on fatty liver and visceral lipid overload might be of considerable therapeutic interest even in less obese Chinese patients with T2DM. Given the baseline BMI in this study is similar to the mean BMI that was reported in China nationwide survey [36], our patients could be representative in clinical settings.
During the interventions, one patient who received exenatide complained of nausea with self-limiting and did not require discontinuation from the study. Mild hypoglycemia was observed in one of the eleven insulin-treated patients. Mild lower extremity edema was seen in one of the eleven pioglitazone-treated patients.
A major limitation of the present study is the smaller number of subjects that might weaken the statistical power. The findings of this study remain worthy to be powered in clinical trial with larger group of patients. In addition, it has been reported that ultrasonography provides a reliable estimate of visceral adipose tissue in nonobese population compared with dual-energy X-ray absorptiometry [37]. Future study might be required to further test its utility in clinical practice for the assessment of body composition by incorporating MRI and ultrasonography.
In summary, this study suggests that, in patients with drug-naive T2DM, liver fat content can be significantly decreased irrespective of using exenatide, insulin, or pioglitazone therapy. Early metabolic control, including glycemic control and weight reduction, plays an important role in slowing progression of fatty liver in T2DM.
References
McGarry JD (2001) Banting lecture 2001: dysregulation of fatty acid metabolism in the etiology of type 2 diabetes. Diabetes 51:7–18
Unger RH (2008) Reinventing type 2 diabetes: pathogenesis, treatment, and prevention. JAMA 299:1185–1187
Vilsbøll T, Christensen M, Junker AE, Knop FK, Gluud LL (2012) Effects of glucagon-like peptide-1 receptor agonists on weight loss: systematic review and meta-analyses of randomised controlled trials. BMJ 344:d7771
Jendle J, Nauck MA, Matthews DR, Frid A, Hermansen K, Düring M, Zdravkovic M, Strauss BJ, Garber AJ (2009) LEAD-2 and LEAD-3 study groups weight loss with liraglutide, a once-daily human glucagon-like peptide-1 analogue for type 2 diabetes treatment as monotherapy or added to metformin, is primarily as a result of a reduction in fat tissue. Diabetes Obes Metab 11:1163–1172
Cuthbertson DJ, Irwin A, Gardner CJ, Daousi C, Purewal T, Furlong N, Goenka N, Thomas EL, Adams VL, Pushpakom SP, Pirmohamed M, Kemp GJ (2012) Improved glycaemia correlates with liver fat reduction in obese, type 2 diabetes, patients given glucagon-like peptide-1 (GLP-1) receptor agonists. PLoS One 7:e50117
Sathyanarayana P, Jogi M, Muthupillai R, Krishnamurthy R, Samson SL, Bajaj M (2011) Effects of combined exenatide and pioglitazone therapy on hepatic fat content in type 2 diabetes. Obesity (Silver Spring) 19:2310–2315
Lindberg M, Astrup A (2007) The role of glitazones in management of type 2 diabetes. A dream or a nightmare? Obes Rev 8:381–384
Bajaj M, Suraamornkul S, Pratipanawatr T, Hardies LJ, Pratipanawatr W, Glass L, Cersosimo E, Miyazaki Y, DeFronzo RA (2003) Pioglitazone reduces hepatic fat content and augments splanchnic glucose uptake in patients with type 2 diabetes. Diabetes 52:1364–1370
Weng J, Li Y, Xu W, Shi L, Zhang Q, Zhu D, Hu Y, Zhou Z, Yan X, Tian H, Ran X, Luo Z, Xian J, Yan L, Li F, Zeng L, Chen Y, Yang L, Yan S, Liu J, Li M, Fu Z, Cheng H (2008) Effect of intensive insulin therapy on beta-cell function and glycaemic control in patients with newly diagnosed type 2 diabetes: a multicentre randomised parallel-group trial. Lancet 371:1753–1760
Hu Y, Li L, Xu Y, Yu T, Tong G, Huang H, Bi Y, Weng J, Zhu D (2011) Short-term intensive therapy in newly diagnosed type 2 diabetes partially restores both insulin sensitivity and β-cell function in subjects with long-term remission. Diabetes Care 34:1848–1853
Juurinen L, Tiikkainen M, Häkkinen AM, Hakkarainen A, Yki-Järvinen H (2007) Effects of insulin therapy on liver fat content and hepatic insulin sensitivity in patients with type 2 diabetes. Am J Physiol Endocrinol Metab 292:E829–E835
Shah PK, Mudaliar S, Chang AR, Aroda V, Andre M, Burke P, Henry RR (2011) Effects of intensive insulin therapy alone and in combination with pioglitazone on body weight, composition, distribution and liver fat content in patients with type 2 diabetes. Diabetes Obes Metab 13:505–510
Alberti KG, Zimmet PZ (1998) Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 15:539–553
Xu W, Bi Y, Sun Z, Li J, Guo L, Yang T, Wu G, Shi L, Feng Z, Qiu L, Li Q, Guo X, Luo Z, Lu J, Shan Z, Yang W, Ji Q, Yan L, Li H, Yu X, Li S, Zhou Z, Lv X, Liang Z, Lin S, Zeng L, Yan J, Ji L, Weng J (2014) Comparison of the effects on glycaemic control and β-cell function in newly diagnosed type 2 diabetes patients of treatment with exenatide, insulin or pioglitazone: a multicentre randomized parallel-group trial (the CONFIDENCE study). J Intern Med Jul 16, Epub ahead of print
Bi Y, Zeng LY, Zhu DL, Yan J, Zhang Y, Tong G, Mu P, Shen S, Hu Y, Yu Q, Liang H, Weng J (2012) Association of β-cell function and insulin sensitivity with fasting and 2 h plasma glucose in a large Chinese population. Diabetes Obes Metab 14:174–180
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Matsuda M, DeFronzo RA (1999) Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care 22:1462–1470
Thomas EL, Hamilton G, Patel N, O’Dwyer R, Doré CJ, Goldin RD, Bell JD, Taylor-Robinson SD (2005) Hepatic triglyceride content and its relation to body adiposity: a magnetic resonance imaging and proton magnetic resonance spectroscopy study. Gut 54:122–127
Liska D, Dufour S, Zern TL, Taksali S, Calí AM, Dziura J, Shulman GI, Pierpont BM, Caprio S (2007) Interethnic differences in muscle, liver, and abdominal fat partitioning in obese adolescents. PLoS One 2:e569
Hwang JH, Stein DT, Barzilai N, Cui MH, Tonelli J, Kishore P, Hawkins M (2007) Increased intrahepatic triglyceride is associated with peripheral insulin resistance: in vivo MR imaging and spectroscopy studies. Am J Physiol Endocrinol Metab 293:E1663–E1669
Porepa L, Ray JG, Sanchez-Romeu P, Booth GL (2010) Newly diagnosed diabetes mellitus as a risk factor for serious liver disease. CMAJ 182:E526–E531
Musso G, Cassader M, Rosina F, Gambino R (2012) Impact of current treatments on liver disease, glucose metabolism and cardiovascular risk in non-alcoholic fatty liver disease (NAFLD): a systematic review and meta-analysis of randomised trials. Diabetologia 55:885–904
Petersen KF, Dufour S, Befroy D, Lehrke M, Hendler RE, Shulman GI (2005) Reversal of nonalcoholic hepatic steatosis, hepatic insulin resistance, and hyperglycemia by moderate weight reduction in patients with type 2 diabetes. Diabetes 54:603–608
Kenny PR, Brady DE, Torres DM, Ragozzino L, Chalasani N, Harrison SA (2010) Exenatide in the treatment of diabetic patients with non-alcoholic steatohepatitis: a case series. Am J Gastroenterol 105:2707–2709
Lim EL, Hollingsworth KG, Aribisala BS, Chen MJ, Mathers JC, Taylor R (2011) Reversal of type 2 diabetes: normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia 54:2506–2514
Asrih M, Jornayvaz F (2013) Inflammation as a link between nonalcoholic fatty liver disease and insulin resistance. J Endocrinol 218:R25–R36
Daniele G, Guardado Mendoza R, Winnier D, Fiorentino TV, Pengou Z, Cornell J, Andreozzi F, Jenkinson C, Cersosimo E, Federici M, Tripathy D, Folli F (2014) The inflammatory status score including IL-6, TNF-α, osteopontin, fractalkine, MCP-1 and adiponectin underlies whole-body insulin resistance and hyperglycemia in type 2 diabetes mellitus. Acta Diabetol 51:123–131
Tripathy D, Daniele G, Fiorentino TV, Perez-Cadena Z, Chavez-Velasquez A, Kamath S, Fanti P, Jenkinson C, Andreozzi F, Federici M, Gastaldelli A, Defronzo RA, Folli F (2013) Pioglitazone improves glucose metabolism and modulates skeletal muscle TIMP-3-TACE dyad in type 2 diabetes mellitus: a randomised, double-blind, placebo-controlled, mechanistic study. Diabetologia 56:2153–2163
Lesmana CR, Hasan I, Budihusodo U, Gani RA, Krisnuhoni E, Akbar N, Lesmana LA (2009) Diagnostic value of a group of biochemical markers of liver fibrosis in patients with non-alcoholic steatohepatitis. J Did Dis 10:201–206
Speliotes EK, Massaro JM, Hoffmann U, Vasan RS, Meigs JB, Sahani DV, Hirschhorn JN, O’Donnell CJ, Fox CS (2010) Fatty liver is associated with dyslipidemia and dysglycemia independent of visceral fat: the Framingham heart study. Hepatology 51:1979–1987
Fernández-Miranda C, Pérez-Carreras M, Colina F, López-Alonso G, Vargas C, Solís-Herruzo JA (2008) A pilot trial of fenofibrate for the treatment of non-alcoholic fatty liver disease. Dig Liver Dis 40:200–205
Spadaro L, Magliocco O, Spampinato D, Piro S, Oliveri C, Alagona C, Papa G, Rabuazzo AM, Purrello F (2008) Effects of n-3 polyunsaturated fatty acids in subjects with nonalcoholic fatty liver disease. Dig Liver Dis 40:194–199
Deurenberg P, Yap M, van Staveren WA (1998) Body mass index and percent body fat: a meta analysis among different ethnic groups. Int J Obes Relat Metab Disord 22:1164–1171
Chiu KC, Cohan P, Lee NP, Chuang LM (2000) Insulin sensitivity differs among ethnic groups with a compensatory response in beta-cell function. Diabetes Care 23:1353–1358
Ma RC, Chan JC (2013) Type 2 diabetes in East Asians: similarities and differences with populations in Europe and the United States. Ann NY Acad Sci 1281:64–91
Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, Shan Z, Liu J, Tian H, Ji Q, Zhu D, Ge J, Lin L, Chen L, Guo X, Zhao Z, Li Q, Zhou Z, Shan G, He J (2010) China National Diabetes and Metabolic Disorders study group prevalence of diabetes among men and women in China. N Engl J Med 362:1090–1101
Bazzocchi A, Diano D, Ponti F, Salizzoni E, Albisinni U, Marchesini G, Battista G (2014) A 360-degree overview of body composition in healthy people: relationships among anthropometry, ultrasonography, and dual-energy X-ray absorptiometry. Nutrition 30:696–701
Acknowledgments
The authors would like to thank all the participating patients. This study was sponsored by Grants from National Natural Science Foundation of China Grant Award (81270906, 81070636), 973 project (2012CB517506), the China postdoctoral Science Foundation (2012M521050), Jiangsu postdoctoral Science Foundation, Jiangsu Province’s Key Provincial Talents Program (RC2011011), the Key Project of Nanjing Medical Science and Technology Development Foundation (ZKX11017, YKK11092), the Project of National Key Clinical Division, Jiangsu Province’s Key Discipline of Medicine (XK201105), National Science Fund for Distinguished Young Scholars (81025005), and New Drug Development, Construction and management of Clinical Biobank for Major Disease (2011ZX0907-001-08).
Conflict of interest
Yan Bi, Bing Zhang, Wen Xu, Huijie Yang, Wenhuan Feng, Cuiliu Li, Guoyu Tong, Ming Li, Xin Wang, Shanmei Shen, Bin Zhu, Jianping Weng, and Dalong Zhu declare that they have no conflict of interest.
Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Managed by Massimo Federici.
Yan Bi and Bing Zhang contributed equally to the paper.
Rights and permissions
About this article
Cite this article
Bi, Y., Zhang, B., Xu, W. et al. Effects of exenatide, insulin, and pioglitazone on liver fat content and body fat distributions in drug-naive subjects with type 2 diabetes. Acta Diabetol 51, 865–873 (2014). https://doi.org/10.1007/s00592-014-0638-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-014-0638-3