Abstract
This study was aimed to assess the associations of hemoglobin A1c (HbA1c), fasting plasma glucose (FPG), and 2h postload plasma glucose (2hPG) with β-cell function in the Chinese population. A total of 913 subjects underwent 75-g oral glucose tolerance test (OGTT) and HbA1c testing. According to OGTT, isolated impaired fasting glucose (i-IFG) was defined as 5.6 mmol/l ≤ FPG < 7.0 mmol/l and 2hPG < 7.8 mmol/l; isolated impaired glucose tolerance (i-IGT) was defined as FPG < 5.6 mmol/l and 7.8 mmol/l ≤ 2hPG < 11.1 mmol/l. HbA1c 5.7–6.4 % was used to identify subjects with prediabetes. Insulin release was calculated by basal homeostasis model assessment of insulin secretion (HOMA-β), early-phase InsAUC30/GluAUC30, and total-phase InsAUC120/GluAUC120. β-cell function relative to insulin sensitivity was expressed as disposition index (DI). All indices of insulin sensitivity and β-cell function gradually decreased with increasing HbA1c, FPG, and 2hPG (all p < 0.01). β-cell function decreased precipitously when HbA1c exceeded 5.5 %. Compared with HbA1c, FPG showed stronger correlations with HOMA-β, InsAUC30/GluAUC30, InsAUC120/GluAUC120, DI30, and DI120 (all p < 0.05), and 2hPG was more closely related to DI30 and DI120 (all p < 0.01). Moreover, FPG was more strongly related to HOMA-β and InsAUC30/GluAUC30 than 2hPG (all p < 0.05). The combination of i-IFG and HbA1c 5.7–6.4 % showed the greatest reduction in DI30 and DI120 compared with HbA1c 5.7–6.4 % alone, i-IGT, or i-IFG (p < 0.05). In conclusion, HbA1c could be used as a marker to identify subjects with impaired β-cell function, but OGTT performs better than HbA1c. The combination of HbA1c and FPG is a simple and sensitive method to evaluate β-cell function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
β-cell dysfunction and insulin resistance play an important role in the pathophysiology underlying the development of type 2 diabetes mellitus (T2DM). Evidences demonstrate that insulin resistance occurs 10–20 years before the onset of diabetes [1]. In order to maintain normal glucose tolerance, β-cell secretes sufficient insulin to respond to insulin resistant state. When the progressive deterioration of β-cell function fails to compensate for insulin resistance, hyperglycemia develops.
A number of studies have examined the relationship between fasting plasma glucose (FPG) or 2h postload plasma glucose (2hPG) and insulin sensitivity or β-cell function [2, 3]. Our previous data have shown that the deterioration of β-cell function and insulin sensitivity contribute to the increase in both FPG and 2hPG in the Chinese population and begin within the normal glycemic range [4, 5].
As an indirect measure of mean blood glucose over the previous 2–3 months, glycated hemoglobin 1c (HbA1c) is well correlated with FPG and 2hPG. In addition, it captures chronic hyperglycemia better than FPG or 2hPG with other advantages such as fasting not needed, sample stability, not being altered by acute factors (stress, diet, exercise etc.). The American Diabetes Association (ADA) has recommended HbA1c as a routine measurement in patients with diabetes [6] and admitted it as a diagnostic tool for diabetes [7]. Recently, studies addressing the questions of the pathophysiological defects responsible for increasing HbA1c have attracted considerable interest. Several studies reported that increased HbA1c was associated with decreased β-cell function [8–11], and another study, however, reported a negative relationship between them [12]. Moreover, some investigators found a better correlation of β-cell function with glucose metabolism parameters derived from OGTT than with HbA1c [8, 11], while others suggested similar effects of glucose metabolism parameters and HbA1c on β-cell function [13]. It is known that differences in β-cell function and insulin sensitivity exist among different races, the ethnic differences also influence HbA1c [14], but no relevant data comparing the different effects of the increase in HbA1c, FPG, and 2hPG on changes in β-cell function in the Chinese population have been reported. Therefore, this study was aimed to investigate the relationship between HbA1c and β-cell function and to compare the abilities of HbA1c, FPG, and 2hPG to identify individuals with impaired β-cell function in Chinese subjects.
Methods
Subjects
This cross-sectional study included 913 individuals who were free of known diabetes and received a 75-g oral glucose tolerance test as an evaluation for glucose tolerance in our department from June 2010 to February 2013. The study protocol was approved by the Ethics Committee of Drum Tower Hospital, and all subjects gave informed consent.
Clinical measurements
A standardized medical history and accurate physical examination were obtained from all subjects before a 75-g OGTT was administered. Measurements of waist (at the midway between the iliac crest and the costal margin) and hip (at the level of the trochanters) circumference were performed twice by the same observer, and the mean value was recorded. Waist-to-hip ratio (WHR) was calculated as waist circumference divided by hip circumference. Weight and height were measured without shoes in light clothing, and body mass index (BMI) was calculated as dividing the body weight in kilograms by the height in meters squared. Blood pressure measurements were taken twice with a standard mercury sphygmomanometer with subjects at rest, and the mean value was calculated. Based on the criterion established by the Working Group On Obesity in China [15], overweight and obesity were defined as 24 kg/m2 ≤ BMI < 28 kg/m2 and BMI ≥ 28 kg/m2, respectively.
Oral glucose tolerance test
All the subjects underwent a 75-g OGTT in the morning after a 10-h overnight fast. Blood samples were collected through an antecubital vein. Blood samples for plasma glucose, insulin, and HbA1c were drawn in the fasting state. The participants then ingested a solution containing 75-g anhydrous glucose in 5 min, and venous blood samples were collected at 30, 60, 120 min for determination of plasma glucose and insulin.
Based on the OGTT, subjects were classified into four categories of glucose tolerance according to the International Diabetes Federation (IDF) guideline [16]: normal glucose tolerance (NGT): FPG < 5.6 mmol/l and 2hPG < 7.8 mmol/l; impaired fasting glucose (i-IFG): 5.6 mmol/l ≤ FPG < 7.0 mmol/l and 2hPG < 7.8 mmol/l; impaired glucose tolerance (i-IGT): FPG < 5.6 mmol/l and 7.8 mmol/l ≤ 2hPG < 11.1 mmol/l; T2DM: FPG ≥ 7.0 mmol/l or 2hPG ≥ 11.1 mmol/l. Glucose tolerance was also determined by HbA1c levels recommended by ADA [7]: normal glucose metabolism, HbA1c < 5.7 %; prediabetes, HbA1c 5.7–6.4 %; T2DM, HbA1c ≥ 6.5 %.
Measurements
Plasma glucose concentration was measured using a hexokinase method (TBA-200FR, Tokyo, Japan). Insulin was determined by electrochemiluminescent immunoassay (Roche, USA). HbA1c analysis was measured by high-performance liquid chromatography (HLC-73G8, Tosoh, Japan).
Calculations
Insulin sensitivity was measured by the homeostasis model assessment as 1/homeostasis model assessment of insulin resistance (1/HOMA-IR) index and Matsuda insulin sensitivity index (ISIM) [17–19], as we described previously [4, 5]. Homeostasis model assessment of insulin secretion (HOMA-β) was calculated as basal insulin release [18]. Early-phase insulin release was calculated as the total insulin area under the curve divided by the total glucose area under the curve during the first 30 min of the OGTT (InsAUC30/GluAUC30), which has previously been shown to have high correlation with the first-phase insulin secretion in intravenous glucose tolerance test [3]. Similarly, total insulin secretion was calculated by insAUC120/GluAUC120. Moreover, insulin secretion relative to insulin sensitivity was expressed as the disposition index (DI) that was calculated as follows: early-phase DI30 = [InsAUC30/GluAUC30] × ISIM and total-phase DI120 = [InsAUC120/GluAUC120] × ISIM [3].
Statistical analysis
All statistical analyses were performed using SPSS version 16.0 and MedCalc Version 11.4.2.0. Data are presented as mean ± SD. Variables with skewed distribution were logarithmically transformed before analysis. Differences in categorical variables were determined by χ2 analysis. The significance of the mean differences was tested by ANOVA followed by Bonferroni post hoc pairwise comparisons or after adjustment of age, sex, and BMI for indexes for insulin sensitivity and β-cell function using the general linear model. Spearman correlation tests were used to determine the relations between glycemic measures and indexes for insulin sensitivity and β-cell function. All p values were two-sided and <0.05 were considered statistically significant.
Results
Clinical characteristics according to HbA1c categories
The 913 participants (49.2 % men and 50.8 % women) in this study have an average age of 50.7 ± 13.6 years and a BMI of 25.1 ± 3.6 kg/m2. Table 1 presents the characteristics of the participants with different HbA1c levels. Subjects with HbA1c 5.7–6.4 % and HbA1c ≥ 6.5 % were older than those with HbA1c < 5.7 %. Participants with HbA1c ≥ 6.5 % tended to be more obese with higher percentage of diabetes family history than the other two groups. Systolic blood pressure (SBP) in HbA1c 5.7–6.4 % and HbA1c ≥ 6.5 % was higher than that in HbA1c < 5.7 %. Diastolic blood pressure (DBP) in HbA1c ≥ 6.5 % was higher than that in HbA1c 5.7–6.4 % and HbA1c < 5.7 %. With increasing HbA1c, plasma glucose concentrations significantly increased as well. No difference in fasting insulin levels was found among the three groups. The 30-min insulin secretion decreased as HbA1c increased; 1- and 2-h insulin release were significantly lower in subjects with HbA1c ≥ 6.5 % than in subjects with HbA1c 5.7–6.4 % and HbA1c < 5.7 %.
Relations between HbA1c and β-cell function
As shown in Fig. 1, subjects were divided into subgroups identified by a 0.2 % increase in HbA1c with HbA1c < 5.1 % as the reference category. Generally, all indexes regarding β-cell function and insulin sensitivity showed a downward trend with the increase in HbA1c. Peripheral insulin sensitivity (1/HOMA-IR and ISIM) decreased gradually with increasing HbA1c without a clear threshold effect, while insulin secretion not adjusted (HOMA-β, InsAUC30/GluAUC30 and InsAUC120/GluAUC120) or adjusted for insulin resistance (DI30 and DI120) decreased sharply for an HbA1c > 5.5 %.
Compared with the HbA1c < 5.7 % group, age-, sex-, and BMI-adjusted 1/HOMA-IR and ISIM were significantly decreased in subjects with HbA1c 5.7–6.4 % (−14 % in 1/HOMA-IR and −13 % in ISIM) and HbA1c ≥ 6.5 % (−32 % in 1/HOMA-IR and −21 % in ISIM) (Fig. 1a). Age-, sex-, and BMI-adjusted HOMA-β, InsAUC30/GluAUC30, InsAUC120/GluAUC120, DI30, and DI120 were significantly decreased (by −24, −29, −21, −39, and −33 %, respectively) in subjects with HbA1c 5.7–6.4 % and substantially reduced (by −56, −58, −55, −68, and −66 %, respectively) in subjects with HbA1c ≥ 6.5 % (Fig. 1b, c).
Correlations between glycemic measures and β-cell function
The correlation coefficients between various indices of β-cell function and the three glycemic measures (FPG, 2hPG, and HbA1c) are shown in Table 2. All the indices of β-cell function and insulin sensitivity showed significant correlations with FPG, 2hPG, and HbA1c. FPG was more strongly correlated with HOMA-β (p < 0.001) and InsAUC30/GluAUC30 (p < 0.05) than 2hPG. Furthermore, FPG showed stronger correlations with all the indices (except for ISIM) for β-cell function and insulin sensitivity than HbA1c (all p < 0.05). Additionally, 2hPG rather than HbA1c was more closely associated with DI30, DI120 and ISIM.
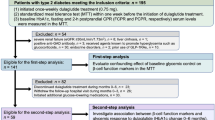
Comparisons of β-cell function in prediabetic subjects defined by HbA1c, OGTT or the combination of the two
Participants were divided into six groups based on the diagnosis of prediabetes according to OGTT and HbA1c: (1) normoglycemia: NGT + HbA1c < 5.7 %; (2) HbA1c 5.7–6.4 % alone: NGT + HbA1c 5.7–6.4 %; (3) IFG alone: i-IFG + HbA1c < 5.7 %; (4) i-IFG + HbA1c 5.7–6.4 %; (5) IGT alone: i-IGT + HbA1c < 5.7 %; and (6) i-IGT + HbA1c 5.7–6.4 %.
After adjusting for age, sex and BMI, compared with the NGT + HbA1c < 5.7 % group, the i-IFG + HbA1c < 5.7 % and i-IFG + HbA1c 5.7–6.4 % groups had a significant decrease in 1/HOMA-IR (P < 0.05) (Fig. 2a), and the i-IFG + HbA1c 5.7–6.4 % and i-IGT + HbA1c 5.7–6.4 % groups had a significant decrease in ISIM (p < 0.05) (Fig. 2b).
Analysis of indexes of insulin sensitivity (a, b), β-cell function (c, d, e), and disposition index (f, g) in subjects with prediabetes defined by HbA1c or OGTT or the combination of the two. Data are shown as mean ± SE. *p < 0.05 versus HbA1c < 5.7 % + NGT group, # p < 0.05 versus HbA1c 5.7–6.4 % alone group, Δ p < 0.05 versus IFG alone group, $ p < 0.05 versus IGT alone group, & p < 0.05 versus IGT + HbA1c 5.7–6.4 % group. Calculations were based on geometric means, adjusted for age, sex, and BMI with the general linear model
HOMA-β in the i-IFG + HbA1c < 5.7 % and i-IFG + HbA1c 5.7–6.4 % groups were significantly lower than that in the other four groups (p < 0.05) (Fig. 2c). InsAUC30/GluAUC30 and InsAUC120/GluAUC120 in all prediabetic groups except for the NGT + HbA1c 5.7–6.4 % group were significantly lower compared with the NGT + HbA1c < 5.7 % group (p < 0.05) (Fig. 2d, e).
DI30 and DI120 were significantly decreased in all prediabetes groups in comparison with the NGT + HbA1c < 5.7 % group and had the greatest reduction in the i-IFG + HbA1c 5.7–6.4 % group (p < 0.05) (Fig. 2f, g).
Effects of age, sex, and BMI on the relation of HbA1c to β-cell function
Subjects were divided into groups with diabetes [men (n = 201) and women (n = 179)] and without diabetes [men (n = 248) and women (n = 285)]. The interaction between HbA1c and BMI in determining β-cell function was significant in individuals with diabetes (p < 0.05) but not in individuals without diabetes. In subjects with diabetes, every 1 % increase in HbA1c concentration was associated with −26.4 % decline in HOMA-β, −23.0 % in InsAUC30/GluAUC30, −27.5 % in InsAUC120/GluAUC120, −19.0 % in DI30, and −23.7 % in DI120 in the non-obese, while the decay rate was −15.1, −7.3, −10.2, −8.0, −10.9 %, respectively, in the obese. No significant interaction between age and sex on the relation of HbA1c levels to β-cell function was found (p > 0.05).
Discussion
Our study demonstrated that, in the Chinese population, the increasing HbA1c levels are associated with decreasing β-cell function. Generally, FPG and 2hPG perform better than HbA1c in detecting β-cell dysfunction. Furthermore, we provided the important finding that subjects with both i-IFG and HbA1c 5.7–6.4 % show worse β-cell function compared to subjects with i-IFG, i-IGT, or HbA1c 5.7–6.4 % alone.
In the present study, we divided all the cases into three groups according to the ADA recommended HbA1c categories and found a significant decrease in β-cell functions from normal glycemia (HbA1c < 5.7 %) to prediabetes (HbA1c 5.7–6.4 %) and diabetes (HbA1c ≥ 6.5 %). Consistent with previous findings in western populations [8, 9], our data indicated that the ADA HbA1c criteria could identify subjects with impaired β-cell function in the Chinese population as well. Further, we found a progressive decrease in HOMA-β, InsAUC30/GluAUC30, InsAUC120/GluAUC120, DI30, and DI120 at the point of HbA1c 5.5 %. Our results demonstrated that, in the Chinese population, β-cell dysfunction occurred in subjects within normal HbA1c levels. Consistent with ours, a study from Japanese individuals also reported that subjects with HbA1c of 5.4–5.5 % have a significant decrease in HOMA-β, insulinogenic index, and DI, compared subjects with HbA1c ≤ 5.1 % [10].
Many studies have reported that both decreased insulin sensitivity and insulin secretion were associated with increased FPG, 2hPG, or HbA1c [3–5, 9–11]. However, few of them investigated the different effects of these three glycemic measures on β-cell function. In the current study, we comparatively studied the correlations between HbA1c, FPG, 2hPG, and β-cell function. Our results demonstrated that increased HbA1c and glycemia (FPG and 2hPG) were associated with decreased β-cell function. However, HbA1c is a less accurate correlate of β-cell function than FPG and 2hPG. Similar results were obtained in a study including 855 participants from three ethnic groups in which researchers showed that, compared with HbA1c, FPG correlated better with the first-phase insulin secretion [8]. In addition to previous studies, we provided a detailed measurement for β-cell function and found that, relative to HbA1c, FPG was more closely correlated with the β-cell function indexes HOMA-β, InsAUC30/GluAUC30, InsAUC120/GluAUC120 and with DI30 and DI120. Moreover, 2hPG presented a stronger association with the β-cell function indexes DI30 and DI120. Additionally, FPG showed a better correlation with basal and early-phase insulin release (HOMA-β and InsAUC30/GluAUC30) than 2hPG. These results were consistent with our previous work which indicated that the decline in insulin secretion was more pronounced with increasing FPG than 2hPG [4].
Further analysis compared the abilities of HbA1c 5.7–6.4 %, i-IFG, i-IGT or the combination of them in identifying individuals with impaired β-cell function. Since they correlate better with β-cell function, both i-IFG and i-IGT could identify subjects with impaired β-cell function better than HbA1c 5.7–6.4 %. Consistent with us, Mustafa et al. also reported that in subjects with NGT no difference in β-cell function was found between the HbA1c < 5.7 % and HbA1c 5.7–6.4 % subgroups, but subjects with i-IFG or i-IGT had a marked decrease in β-cell function despite similar HbA1c levels [11].
Although HbA1c played a less important role than FPG and 2hPG in detecting β-cell dysfunction, we for the first time found that the combination of HbA1c 5.7–6.4 % and i-IFG presented the relatively greatest reduction in DI30 and DI120 when the normal glycemia group was used as the reference category. Because insulin secretion is modulated by insulin sensitivity, as an index calculated from insulin secretion adjusted for insulin sensitivity, DI is the optimal measurement of β-cell function. Furthermore, a longitudinal study reported that DI was predictive of development of diabetes over 10 years [20]. Thus, since it works better in detecting decreased DI30 and DI120 as well as in predicting diabetes [21–23], measurement of HbA1c in association with FPG could provide a better tool in identifying subjects with impaired β-cell function.
Finally, our results indicated that obesity does not affect insulin secretion with increasing HbA1c in subjects without diabetes. However, significant interaction between BMI and HbA1c in determining insulin secretion was found in subjects with diabetes: with increasing HbA1c, insulin secretion in the non-obese individuals with diabetes decreased faster than in the obese. Lorenzo et al. also reported a negative interaction effect of obesity on the relationship between HbA1c and insulin secretion in individuals without diabetes [8], but no further data in individuals with diabetes were reported. Previous evidences suggested that obese subjects have higher insulin secretion than lean subjects in people with NGT or diabetes [24, 25]. The β-cell in obese subjects with diabetes could, perhaps, secret more insulin than in lean subjects with diabetes to compensate for the increased insulin resistance. This may be one of the causes leading to the differences between the obese and lean individuals, but it still remains to be determined.
There are some limitations to this study. Although we studied the decay rates of the β-cell function with increasing HbA1c and glucose and the differences between them, this question is better addressed by longitudinal rather than cross-sectional studies. In addition, the indexes of insulin secretion and action were not derived directly from glucose clamp techniques, which are the gold standard for assessment of β-cell function and insulin sensitivity. Nevertheless, previous studies have reported high correlations of these indexes derived from OGTT with euglycemic insulin clamp or IVGTT [3, 17, 26–28] and validated their usefulness in several large-scale studies [3, 29, 30].
In summary, the ADA recommended HbA1c criteria for prediabetes and T2DM could identify subjects with impaired β-cell function in the Chinese population. FPG and 2hPG predict β-cell function better than HbA1c. The combination of HbA1c and FPG may be a good choice to detect loss of β-cell function and allow for early intervention to slow the progressive β-cell dysfunction.
References
Shulman GI (2000) Cellular mechanisms of insulin resistance. J Clin Invest 106:171–176
Festa A, D’Agostino R Jr, Hanley AJ, Karter AJ, Saad MF, Haffner SM (2004) Differences in insulin resistance in nondiabetic subjects with isolated impaired glucose tolerance or isolated impaired fasting glucose. Diabetes 53:1549–1555
Stancakova A, Javorsky M, Kuulasmaa T, Haffner SM, Kuusisto J, Laakso M (2009) Changes in insulin sensitivity and insulin release in relation to glycemia and glucose tolerance in 6, 414 Finnish men. Diabetes 58:1212–1221
Bi Y, Zeng L, Zhu D, Yan J, Zhang Y, Tong G, Mu P, Shen S, Hu Y, Yu Q (2012) Association of beta-cell function and insulin sensitivity with fasting and 2-h plasma glucose in a large Chinese population. Diabetes Obes Metab 14:174–180
Bi Y, Zhu D, Jing Y, Hu Y, Feng W, Shen S, Tong G, Shen X, Yu T, Song D (2010) Decreased beta cell function and insulin sensitivity contributed to increasing fasting glucose in Chinese. Acta Diabetol 49(Suppl 1):S51–S58
American Diabetes Association (1989) Standards of medical care for patients with diabetes mellitus. Diabetes Care 12:365–368
American Diabetes Association (2010) Standards of medical care in diabetes—2010. Diabetes Care 33(Suppl 1):S11–S61
Lorenzo C, Wagenknecht LE, Hanley AJ, Rewers MJ, Karter AJ, Haffner SM (2010) A1C between 5.7 and 6.4% as a marker for identifying pre-diabetes, insulin sensitivity and secretion, and cardiovascular risk factors: the Insulin Resistance Atherosclerosis Study (IRAS). Diabetes Care 33:2104–2109
Sjaarda LA, Michaliszyn SF, Lee S, Tfayli H, Bacha F, Farchoukh L, Arslanian SA (2012) HbA1c diagnostic categories and beta-cell function relative to insulin sensitivity in overweight/obese adolescents. Diabetes Care 35:2559–2563
Heianza Y, Arase Y, Fujihara K, Tsuji H, Saito K, Hsieh SD, Kodama S, Shimano H, Yamada N, Hara S, Sone H (2012) High normal HbA(1c) levels were associated with impaired insulin secretion without escalating insulin resistance in Japanese individuals: the Toranomon Hospital Health Management Center Study 8 (TOPICS 8). Diabet Med 29:1285–1290
Kanat M, Winnier D, Norton L, Arar N, Jenkinson C, DeFronzo RA, Abdul-Ghani MA (2011) The relationship between β-cell function and glycated hemoglobin results from the Veterans Administration Genetic Epidemiology Study. Diabetes Care 34:1006–1010
Wang JS, Lee IT, Lee WJ, Lin SY, Fu CP, Ting CT, Lee WL, Liang KW, Sheu WH (2013) Performance of HbA1c and fasting plasma glucose in screening for diabetes in patients undergoing coronary angiography. Diabetes Care 36:1138–1140
Bianchi C, Miccoli R, Bonadonna RC, Giorgino F, Frontoni S, Faloia E, Marchesini G, Dolci MA, Cavalot F, Cavallo GM, Leonetti F, Del Prato S (2012) Pathogenetic mechanisms and cardiovascular risk: differences between HbA1c and oral glucose tolerance test for the diagnosis of glucose tolerance. Diabetes Care 35:2607–2612
Herman WH (2009) Do race and ethnicity impact hemoglobin A1c independent of glycemia? J Diabetes Sci Technol 3:656–660
Bei‐Fan Z (2002) Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults: study on optimal cut‐off points of body mass index and waist circumference in Chinese adults. Asia Pac J Clin Nutr 11:S685–S693
IDF Clinical Guidelines Task Force (2012) International diabetes federation global guideline for type 2 diabetes. http://www.idf.org/global-guideline-type-2-diabetes-2012. Accessed 27 March 2013
Matsuda M, DeFronzo RA (1999) Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care 22:1462–1470
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Abdul-Ghani MA, Matsuda M, Balas B, DeFronzo RA (2007) Muscle and liver insulin resistance indexes derived from the oral glucose tolerance test. Diabetes Care 30:89–94
Utzschneider KM, Prigeon RL, Faulenbach MV, Tong J, Carr DB, Boyko EJ, Leonetti DL, McNeely MJ, Fujimoto WY, Kahn SE (2009) Oral disposition index predicts the development of future diabetes above and beyond fasting and 2-h glucose levels. Diabetes Care 32:335–341
Ko GT, Chan JC, Tsang LW, Cockram CS (2000) Combined use of fasting plasma glucose and HbA1c predicts the progression to diabetes in Chinese subjects. Diabetes Care 23:1770–1773
Nomura K, Inoue K, Akimoto K (2012) A two-step screening, measurement of HbA1c in association with FPG, may be useful in predicting diabetes. PLoS ONE 7:e36309
Heianza Y, Hara S, Arase Y, Saito K, Fujiwara K, Tsuji H, Kodama S, Hsieh SD, Mori Y, Shimano H, Yamada N, Kosaka K, Sone H (2011) HbA1c 5.7–6.4% and impaired fasting plasma glucose for diagnosis of prediabetes and risk of progression to diabetes in Japan (TOPICS 3): a longitudinal cohort study. Lancet 378:147–155
Elbein SC, Wegner K, Kahn SE (2000) Reduced beta-cell compensation to the insulin resistance associated with obesity in members of caucasian familial type 2 diabetic kindreds. Diabetes Care 23:221–227
Jie H, Weiqiong G, Yifei Z, Yuhong C, Shouyue S, Yongjie Z, Guang N (2003) Study on insulin sensitivity and islet β cell’s function in obesity and non-obesity type 2 diabetes. Chin J Diabetes 11:96–99
Retnakaran R, Shen S, Hanley AJ, Vuksan V, Hamilton JK, Zinman B (2008) Hyperbolic relationship between insulin secretion and sensitivity on oral glucose tolerance test. Obesity (Silver Spring) 16:1901–1907
Retnakaran R, Qi Y, Goran MI, Hamilton JK (2009) Evaluation of proposed oral disposition index measures in relation to the actual disposition index. Diabet Med 26:1198–1203
Stumvoll M, Mitrakou A, Pimenta W, Jenssen T, Yki-Järvinen H, Van Haeften T, Renn W, Gerich J (2000) Use of the oral glucose tolerance test to assess insulin release and insulin sensitivity. Diabetes Care 23:295–301
Hanefeld M, Koehler C, Fuecker K, Henkel E, Schaper F, Temelkova-Kurktschiev T (2003) Insulin secretion and insulin sensitivity pattern is different in isolated impaired glucose tolerance and impaired fasting glucose: the risk factor in impaired glucose tolerance for Atherosclerosis and Diabetes Study. Diabetes Care 26:868–874
Tripathy D, Carlsson M, Almgren P, Isomaa B, Taskinen MR, Tuomi T, Groop LC (2000) Insulin secretion and insulin sensitivity in relation to glucose tolerance: lessons from the Botnia Study. Diabetes 49:975–980
Acknowledgments
This study was sponsored by grants from the National Natural Science Foundation of China Grant Award (81270906, 30800539, 81070636), the Project of National Key Clinical Division, the China postdoctoral Science Foundation (2012M521050), Jiangsu postdoctoral Science Foundation, Jiangsu Province’s Key Provincial Talents Program (RC2011011), Jiangsu Province’s Key Discipline of Medicine (XK201105), and the Key Project of Nanjing Medical Science and Technology Development Foundation (ZKX11017).
Conflict of interest
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Communicated by Massimo Porta.
Cuiliu Li and Huijie Yang have contributed equally to the paper.
Rights and permissions
About this article
Cite this article
Li, C., Yang, H., Tong, G. et al. Correlations between A1c, fasting glucose, 2h postload glucose, and β-cell function in the Chinese population. Acta Diabetol 51, 601–608 (2014). https://doi.org/10.1007/s00592-014-0563-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-014-0563-5