Abstract
Type 2 diabetes is associated with risk of cancer. Hyperinsulinemia and insulin resistance may be the link with cancer, but whether this is independent of the diabetes status, obesity/visceral obesity and metabolic syndrome is uncertain and the present study wanted to address this issue. Fifteen-year all-cause, CVD and cancer mortality data were obtained through the Regional Health Registry in 2,011 out of 2,074 Caucasian middle-aged individuals of the Cremona Study, a population study on the prevalence of diabetes mellitus in Italy in which anthropometric and metabolic characteristics were collected. During the 15-year observation period, 495 deaths were registered: 221 CVD related and 180 cancer related. Age and sex were independently associated with all-cause, cancer and CVD mortality rates. Age- and sex-adjusted analysis showed that HOMA-IR, cigarette smoking and diabetes were independently associated with all-cause mortality; HOMA-IR, systolic blood pressure and fibrinogen were independently associated with CVD mortality; HOMA-IR and smoking habit were independently associated with cancer mortality. Individuals in the highest quintile of serum insulin had a 62% higher risk of cancer mortality (HR = 1.62 95% CI: 1.19–2.20; P < 0.0022) and 161% higher risk of gastrointestinal cancer mortality (HR = 2.61 95% CI: 1.73–3.94; P < 0.0001). Age- and sex-adjusted analysis showed that hyperinsulinemia/insulin resistance is associated with cancer mortality independently of diabetes, obesity/visceral obesity and the metabolic syndrome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epidemiologic studies reported a relationship between type 2 diabetes and the risk of developing different cancers [1]. Potential mediators of this association may be obesity and visceral obesity, insulin resistance, the metabolic syndrome, which are largely prevalent in the diabetic population [2–4] even if a specific role of chronic hyperglycemia cannot be excluded [3]. Since insulin is a growth factor for many cells in culture systems, and since insulin increases the availability of IGF-I, another well-known tumor growth factor [5], hyperinsulinemia probably represents a good potential candidate to explain the association between diabetes and cancer [6]. In the Cremona study, a population survey carried out in 1990–1991 in Lombardy, Italy [7, 8], accurate data about diabetes status, fasting glucose and insulin concentration, body composition (weight, height and waist circumference) and the criteria for the appropriate diagnosis of the metabolic syndrome (serum glucose, lipid profile, blood pressure along with waist circumference) were carefully collected. Fifteen years later, vital status and time of death were ascertained through Regional Health Registry files, and causes of death were classified using the International Classification of Diseases. Aim of this study was, therefore, to assess whether a relationship between fasting insulin and cancer mortality could be detected in this Italian population and whether this association was independent of the diabetes status and fasting glucose, obesity (and visceral obesity) and the metabolic syndrome.
Patients and methods
Study cohort and follow-up
The Cremona study was a large population survey in the health district of Cremona (38,643 inhabitants of three representative municipalities: Cremona, Casalbuttano, Vescovato) performed in order to estimate the prevalence of diagnosed and undiagnosed diabetes and impaired glucose tolerance according to the oral glucose tolerance test and WHO criteria in northern Italy and to set up a population cohort in anticipation of a follow-up study [7, 8]. After an information campaign, 2,074 of the selected subjects visited one of the three clinics set up for this program (one in each town); 2,074 individuals >40 years old were enrolled, and data about 2,011 were available for this analysis. The anthropometric and laboratory features are summarized in Table 1. Past medical history, anthropometric parameters and clinical data of subjects were collected through a standard protocol conducted by trained interviewers. Venous blood sample was collected after 12-h overnight fast and 2 h after the oral administration of 75-g glucose monohydrate. Further details concerning the study protocol have been reported previously [7, 8]. This phase was completed in a 9-month period, following April 2, 1990. Fifteen years later, vital status and time of death were ascertained through Regional Health Registry files, and causes of death were classified using the International Classification of Diseases, Ninth Revision (death codes for CVD from 401 to 448 and cancer from 140.0 to 208.9). Cancer mortality was established in 180 individuals and details are reported in Table 2. Median follow-up was 180 months, and median follow-up of those still alive was 182 months (98% of the still alive had a minimum follow-up period of 174 months). At this stage, data regarding 2,011 individuals were available. The study was approved by the Ethical Committee of the Istituto Scientifico H San Raffaele.
Definition of diabetes, impaired glucose tolerance (IGT) and metabolic syndrome
Diabetes was defined at that time according to a previously known diabetes status (patients on oral hypoglycemic agents) or according to the results of the OGTT and on WHO criteria (fasting plasma glucose ≥7.0 mmol/L or 2-h plasma glucose ≥11.1 mmol/L). Patients with known diabetes did not undergo the OGTT. IGT was defined as fasting plasma glucose <7.0 mmol/L and 2-h plasma glucose ≥7.8 and <11.1 mmol/L. Metabolic syndrome was defined accordingly to the definition of the NCEP Adult Treatment Program III [9]. Data about waist, fasting plasma glucose, systolic and diastolic blood pressure, HDL cholesterol and triglycerides were available for at least 2,011 individuals. Insulin and HOMA-IR were available in 1,994 out of 2,011.
Analytical determinations
Blood, serum and plasma substrates were assessed as previously described [7, 8].
Calculation
BMI was calculated as weight in kilograms divided by the square of height in meters. Alcohol consumption was calculated as units of alcohol (glass of wine = 20 g, glass of aperitif = 30 g and glass of liquor = 80 g). HOMA-IR was calculated as previously described [10].
Statistical analysis
Analyses were performed using the Statistical Analysis System (SAS) Software (v.9.1). Concentrations are presented as average ±SD unless differently stated. Because of the skewed distribution of serum insulin, triglycerides, fibrinogen, glucose, log-transformed values were used in the analysis. The association of each investigated risk factors with total cancer mortality after the 15-year observational period was estimated by the Cox proportional hazard model adjusting for age and sex. Hazard ratio (HR) and 95% C.I. are presented. The multivariate Cox proportional model (stepwise), including parameters with P values <0.1 at univariate analysis, was used to investigate the independent association of the risk factors with all-cause, CVD and cancer mortality. Subtypes of cancer were subdivided as summarized in Table 2 as those of the gastrointestinal tract, respiratory system, urogenital system, lympho-hemopoietic system and the others (brain tumors, tumors of the abdominal cavity and nonspecified malignant tumors). Survival curves for total cancer mortality in quintile of fasting insulin (1st to 4th quintiles vs. 5th quintile) were estimated by the Kaplan and Meier method, and comparisons among survival curves were made by means of the log-rank test.
Results
Anthropometric and laboratory characteristics of study subjects (Table 1)
The population was constituted by overweight individuals; 22% of the study subjects were active smokers and they have higher than normal systolic blood pressure and total cholesterol. Metabolic syndrome was detected in 34% and diabetes in 9.5% of the population.
All-cause mortality during the 15-year observation period
During the 15-year observation period, 495 deaths were registered: 221 CVD related and 180 cancer related. Age (HR: 1.11, 95% CI: 1.10–1.12; P < 0.0001) and sex (HR: 0.47, 95% CI: 0.39–0.56; P < 0.0001) were associated with higher all-cause mortality.
When multivariate analysis was performed adjusting for age and sex, HOMA-IR (HR: 1.05, 95% CI: 1.03–1.07; P < 0.0001), cigarette smoking (HR: 1.72, 95 CI: 1.38–2.16; P < 0.0001) and diabetes (HR: 1.45, 95% CI: 1.12–1.88; P < 0.0047) were all independently associated with all-cause mortality, while BMI and waist did not.
CVD mortality during the 15-year observation period
Age (HR:1.13, 95% CI: 1.11–1.15; P < 0.0001) and sex (HR: 0.38, 95% CI: 0.29–0.50; P < 0.0001) were associated with higher CVD mortality. When analysis was performed adjusting for age and sex, HOMA-IR (HR: 1.05, 95% CI: 1.03–1.08; P < 0.0001), systolic blood pressure (HR: 1.01; 95% CI: 1.00–1.02; P < 0.0027) and fibrinogen (HR: 1.00, 95% CI: 1.00–1.01; P < 0.0196) were independently associated with CVD mortality, while BMI and waist did not.
Cancer mortality during the 15-year period of follow-up. Anthropometric and laboratory features of the cases: univariate analysis after the 15-year observational period (Table 3)
In univariate analysis, the anthropometric features (BMI and waist) and metabolic syndrome were not associated with higher risk for cancer mortality. Parameters of glucose homeostasis (fasting glucose and insulin concentrations, HOMA-IR, the surrogate index of insulin resistance) and prevalence of diabetes were associated with higher risk for cancer mortality. The smoking habit and the daily alcohol consumption were associated with higher risk of cancer mortality as well.
Multivariate analysis after the 15-year observational period (Table 4)
Multivariate analysis was performed using only variables significant at P < 0.1 in univariate analysis. Along with age and sex (male), the risk of total cancer mortality was associated with the smoking habit and with HOMA-IR. To understand the relative contribution of fasting insulin and fasting glucose (the factors used to calculate HOMA-IR), we repeated the multivariate analysis excluding HOMA-IR and found that only fasting insulin, but not glucose, retained an independent association.
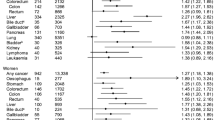
Multivariate analysis after the 15-year observational period: cancer subtypes
Analysis related to the single cancers was not possible because of the low number of events. Therefore, we performed the analysis grouping the cancer mortality in categories: gastrointestinal tract, respiratory system, urogenital system, lympho-hemopoietic system. Variables associated with the mortality for cancer of the gastrointestinal tract paralleled those selected for total cancer mortality: age (HR 1.096; 95% CI: 1.072–1.120; P < 0.0001), sex (HR 0.336; 95% CI: 0.211–0.533; P < 0.0001), smoking habit (HR 2.088; 95% CI: 1.278–3.413; P < 0.0033) and fasting insulin (HR 1.020; 95% CI: 1.008–1.033; P < 0.0015). For the mortality of cancer of the respiratory system, we found an association with age (HR 1.073; 95% CI: 1.040–1.107; P < 0.0001), sex (HR 0.403; 95% CI: 0.203–0.798; P < 0.0091) and smoking habit (HR 4.848; 95% CI: 2.504–9.388; P < 0.0001). Age (HR 1.080; 95% CI: 1.059–1.102; P < 0.0001), sex (HR 0.294; 95% CI: 0.192–0.448; P < 0.0001) and diabetes (HR 1.927; 95% CI: 1.155–3.213; P < 0.012) were associated with cancer mortality of the urogenital system. Only age (HR 1.070; 95% CI: 1.024–1.119; P < 0.0027) was selected with respect to cancer mortality of the lympho-hemopoietic system.
Total cancer mortality in the 5th quintile of fasting serum insulin concentration
We analyzed the features of subjects with the highest fasting serum insulin concentrations. Cutoff values for insulin quintiles were: 48, 66, 90, 126 pmol/L. In the subjects within the 5th quintile of fasting serum insulin (>126 pmol/L), the total cancer mortality was higher than in those in the 1st to 4th quintiles (combined) of fasting insulin: 14.3% with respect to 8.7% (HR = 1.617 95% CI: 1.189–2.198; P < 0.0022). The test for linear trend resulted significant (P = 0.007). In Fig. 1, the survival by Kaplan–Meier estimates of total cancer mortality is shown. The individuals within this quintile of fasting insulin had also a higher risk of mortality for cancers of the gastrointestinal tract (HR = 2.611 95% CI: 1.729–3.942; P < 0.0001) than in those in the 1st to 4th quintiles (combined) of fasting insulin.
Survival by Kaplan–Meier estimates of total cancer mortality. The association of insulinemia with total cancer mortality was estimated after a 15-year observational period. Subjects were divided according to fasting serum insulin level in two groups (subjects within the 1st to 4 th quintiles combined of fasting serum insulin versus subjects within the 5th quintile). Statistical analysis was performed by log-rank test
Discussion
In our cohort of middle-aged individuals, the fasting insulin concentration was related to total cancer mortality in an age- and sex-adjusted analysis. This association was detected independently of other metabolic conditions potentiality involved into the development of cancer: (1) parameters of general body adiposity (BMI) but also of visceral adiposity (waist), (2) overt diabetes but also glucose intolerance, based on the OGTT and (3) the metabolic syndrome, based on the ATP III definition. In addition, individuals within the quintile of highest concentration of fasting serum insulin were characterized by a higher risk of total mortality for cancer (Fig. 1) and for cancers of the gastrointestinal tract.
Pathophysiologic implications
Type 2 diabetes is associated with higher cancer mortality, higher risk of developing specific cancers and a higher risk of a more aggressive progression of the neoplastic disease. Several metabolic factors related with diabetes were taken into consideration as mediators of this detrimental prognosis. Obesity is associated with colon cancer because the RR of these subjects is one to twofold higher than in those with BMI in the normal range [11]; nevertheless, this relationship was reported to be stronger in men than in women [12] arguing for a potential effect of body fat distribution. Studies showing a relationship between waist and colon cancer, independent of BMI, led to the conclusion that it is possible that some metabolic features typical of the central adiposity increase the risk of colon cancer [12]. Obesity is also associated with the prostate cancer, but in this case, it appears to be involved with the progression of prostate cancer rather than its onset or induced mortality [3]. Also, chronic hyperglycemia, inducing oxidative stress, may be an important mediator of carcinogenesis in certain tumors such as the pancreatic cancer [13]. Finally, some studies found that individuals with the metabolic syndrome had elevated risk to develop the colon cancer [14–16]. Our results would support the hypothesis that hyperinsulinemia/insulin resistance may be potential detrimental factors acting at different steps of carcinogenesis in diabetic individuals. In previous epidemiological studies, hyperinsulinemia was found to be related to colon, prostate and pancreatic cancers. In those studies, reviewed by Giovannucci and Michaud [3], there was a lack of knowledge of the diabetic status and insulin resistance that we collected in our Cremona study allowing us to control and adjust the effect of hyperinsulinemia also for adiposity and hyperglycemia, all simultaneously assessed in the cohort.
The lack of association between BMI/waist and cancer mortality despite the presence of association between cancer mortality and insulin resistance/hyperinsulinemia was somehow a surprising result of our work. Insulin resistance, body mass and central adiposity are tightly linked each other, sometimes in a collinear fashion, and it is difficult to dissect out the relative contribution of each of these variables. Nevertheless, one of the strengths of our work is the simultaneous assessment of these variables, and it was concluded that insulin HOMA-IR was a more sensitive predictor, and we have to emphasize that this was found despite the fact that in our cohort, the variability of HOMA-IR was much greater than the variability of BMI and waist. In agreement with our finding, Ausk et al. [17] recently reported HOMA-IR to be independently associated with increased all-cause mortality in nondiabetic adults after adjusting for measures of obesity, including BMI and waist-to-hip ratio, but only among persons with BMI <25.2. These findings suggest that “high” BMI−related insulin resistance does not confer an independent, excess risk of mortality while “low” BMI–related insulin resistance is independently associated with mortality [17]. In our view, this finding would confirm that when the confounding effect of body adiposity is cleared, the effect of hyperinsulinemia becomes more evident. A second explanation could be related to the fact that BMI/waist increases risk of some but not all cancers, and the number of events due to specific cancer group with relevant interest (colon, pancreas, breast and prostate) could be too low to reach a reliable power.
An important consideration is that hyperinsulinemia and insulin resistance are tightly linked each other. HOMA-IR, the mathematical product of fasting glucose and insulin, was independently associated with cancer mortality (Table 4), but even if HOMA-IR is known to be a reliable surrogate marker of insulin resistance with respect to glucose metabolism [18, 19], we feel difficult to speculate about how HOMA-IR may reflect insulin action on cell growth and differentiation. At this stage, we simply believe that hyperinsulinemia and hyperglycemia bringing additive information when used mathematically as a product had a higher predictive power than when they are taken into consideration separately; more importantly, when the specific impact on the two was dissected out, we found that insulin was more relevant than glucose.
Potential relevance with respect to the therapeutic strategy
In our cohort, cancer mortality was frequent as of that for CVD mortality. In the subgroup of individuals with diabetes, the comparative CVD mortality ratio (compared to that of the entire cohort) was 80 and 90% higher in diabetic men and women, respectively. The comparative mortality ratio for cancer was 30 and 26% higher in diabetic men and women, respectively. This finding is in agreement with previous reports related to US populations [6]. Therefore, also in our Italian cohort, even if the relevance of CVD disease mortality in patients with diabetes remained of pivotal importance, also the cancer mortality resulted remarkably higher than in the nondiabetic population. If hyperinsulinemia/insulin resistance will be further confirmed to be a variable able to explain the excess risk of cancer in diabetic and insulin resistant patients, strategies to alleviate hyperinsulinemia in these individuals should be taken into account either in hyperinsulinemic subject without cancer for primary prevention (emphasizing the importance of lifestyle intervention for the prevention of neoplastic diseases) but also in diabetic individuals with overt neoplastic diseases to potentially improve their life expectancy and prognosis [20]. Following this logic, interventions able to determine insulin sensitization and to reduce the circulating insulin levels should be tested. Metformin administration, which is able to reduce circulating insulin levels, was associated with lower risk of cancer than the administration of insulin or sulfonylureas in patients with type 2 diabetes [21–24], and some authors are now testing metformin in breast cancer [25].
Limitations of the study
In complex, we had a reasonably high number of total events. A limitation of our work was that we had little chance to establish whether hyperinsulinemia had a specific relevance for the mortality related to specific tumors. We could only report that when cancer-related mortality was segregated in four subgroups associated with the gastrointestinal, respiratory, urogenital and lympho-hemopoietic systems, fasting insulin was significantly associated with cancer mortality of the gastrointestinal tract. Most of these events were related to cancers of the liver and biliary ducts, pancreas and stomach: those with the worst prognosis and more likely to be responsible for mortality. Our study was not designed to establish during the observational period the onset of cancer regardless of the fact that it was or was not identified as the cause of mortality. Another limitation of the study was that we did not collect data serially; the association we report in the present work is between one single assessment of these parameters and cancer mortality assessed 15 years later. A final comment is related to the fact that dietary habits, habitual physical activity and antidiabetic therapies are additional metabolic variables with a well-recognized impact on insulin sensitivity and with potential impact on carcinogenesis, and in the present study, we did not collect this kind of information. In particular, antidiabetic therapies were recently described as potentially relevant both in terms of cancer risk and cancer progression. Some large cohort studies have reported lower cancer incidence and mortality in diabetic patients treated with metformin [21, 25]. A recent meta-analysis concluded that metformin in diabetic patients is associated with a decreased risk of cancer incidence compared with other treatments, even if most studies were retrospective [26]. On the other hand, insulin, sulfonylureas and thiazolidinediones have been variably reported to have no effect or a slightly increasing or a significantly reducing effect on cancer risk [27, 28].
Conclusion
We report that fasting hyperinsulinemia was independently associated with cancer mortality regardless of the diabetic status, fasting glucose, obesity and the metabolic syndrome, providing epidemiological support to the hypothesis that hyperinsulinemia/insulin resistance—rather than hyperglycemia, body fatness and the metabolic syndrome—is the most important metabolic variable related to cancer mortality risk in patients with type 2 diabetes.
References
Coughlin SS, Calle EE, Teras LR, Petrelli J, Thun MJ (2004) Diabetes mellitus as a predictor of cancer mortality in a large cohort of US adults. Am J Epidemiol 159:1160–1167
Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ (2003) Overweight, obesity, and mortality from cancer in a prospectively studied cohort of US adults. N Engl J Med 348:1625–1638
Giovannucci E, Michaud D (2007) The role of obesity and related metabolic disturbances in cancers of the colon, prostate, and pancreas. Gastroenterology 132:2208–2225
Nicolucci A (2010) Epidemiological aspects of neoplasms in diabetes. Acta Diabetol 47:87–95
Annunziata M, Granata R, Ghigo E (2011) The IGF system. Acta Diabetol 48:1–9
Vigneri R, Frasca F, Sciacca L, Vigneri P, Frittitta L (2009) Re: insulin, insulin-like growth factor-I, and risk of breast cancer in postmenopausal women. J Natl Cancer Inst 101:1030–1031; author reply 1031–1032
Garancini MP, Calori G, Manara E, Izzo A, Ebbli E, Galli L, Boari L, Gallus G (1993) An Italian population-based study of the prevalence of diabetes: some methodological aspects. Diabete Metab 19:116–120
Garancini MP, Calori G, Ruotolo G, Manara E, Izzo A, Ebbli E, Bozzetti AM, Boari L, Lazzari P, Gallus G (1995) Prevalence of NIDDM and impaired glucose tolerance in Italy: an OGTT-based population study. Diabetologia 38:306–313
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) (2002) Third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation 106:3143–3421
Perseghin G, Caumo A, Caloni M, Testolin G, Luzi L (2001) Incorporation of the fasting plasma FFA concentration into QUICKI improves its association with insulin sensitivity in nonobese individuals. J Clin Endocrinol Metab 86:4776–4781
Giovannucci E (2001) Insulin, insulin-like growth factors and colon cancer: a review of the evidence. J Nutr 131:3109S–3120S
Pischon T, Lahmann PH, Boeing H, Friedenreich C, Norat T, Tjonneland A, Halkjaer J, Overvad K, Clavel-Chapelon F, Boutron-Ruault MC, Guernec G, Bergmann MM, Linseisen J, Becker N, Trichopoulou A, Trichopoulos D, Sieri S, Palli D, Tumino R, Vineis P, Panico S, Peeters PH, Bueno-de-Mesquita HB, Boshuizen HC, Van Guelpen B, Palmqvist R, Berglund G, Gonzalez CA, Dorronsoro M, Barricarte A, Navarro C, Martinez C, Quiros JR, Roddam A, Allen N, Bingham S, Khaw KT, Ferrari P, Kaaks R, Slimani N, Riboli E (2006) Body size and risk of colon and rectal cancer in the European Prospective Investigation Into Cancer and Nutrition (EPIC). J Natl Cancer Inst 98:920–931
Busik JV, Hootman SR, Greenidge CA, Henry DN (1997) Glucose-specific regulation of aldose reductase in capan-1 human pancreatic duct cells In vitro. J Clin Invest 100:1685–1692
Ahmed RL, Schmitz KH, Anderson KE, Rosamond WD, Folsom AR (2006) The metabolic syndrome and risk of incident colorectal cancer. Cancer 107:28–36
Aleksandrova K, Boeing H, Jenab M, Bueno-de-Mesquita HB, Jansen E, van Duijnhoven F, Fedirko V, Rinaldi S, Romieu I, Riboli E, Romaguera D, Overvad KK, Ostergaard JN, Olsen A, Tjonneland AA, Boutron-Ruault MC, Clavel-Chapelon F, Morois S, Masala G, Agnoli C, Panico S, Tumino R, Vineis P, Kaaks R, Lukanova A, Trichopoulou A, Naska A, Bamia C, Peeters PH, Rodriguez L, Buckland G, Sanchez MJ, Dorronsoro M, Huerta JM, Barricarte Gurrea A, Hallmans G, Palmqvist R, Khaw KT, Wareham NJ, Allen NE, Tsilidis KK, Pischon T (2011) Metabolic syndrome and risks of colon and rectal cancer: the European prospective investigation into cancer and nutrition study. Cancer Prev Res (Phila) 66:1873–1883
Bowers K, Albanes D, Limburg P, Pietinen P, Taylor PR, Virtamo J, Stolzenberg-Solomon R (2006) A prospective study of anthropometric and clinical measurements associated with insulin resistance syndrome and colorectal cancer in male smokers. Am J Epidemiol 164:652–664
Ausk KJ, Boyko EJ, Ioannou GN (2010) Insulin resistance predicts mortality in nondiabetic individuals in the US. Diabetes Care 33:1179–1185
Bonora E, Targher G, Alberiche M, Bonadonna RC, Saggiani F, Zenere MB, Monauni T, Muggeo M (2000) Homeostasis model assessment closely mirrors the glucose clamp technique in the assessment of insulin sensitivity: studies in subjects with various degrees of glucose tolerance and insulin sensitivity. Diabetes Care 23:57–63
Katz A, Nambi SS, Mather K, Baron AD, Follmann DA, Sullivan G, Quon MJ (2000) Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J Clin Endocrinol Metab 85:2402–2410
Barone BB, Yeh HC, Snyder CF, Peairs KS, Stein KB, Derr RL, Wolff AC, Brancati FL (2008) Long-term all-cause mortality in cancer patients with preexisting diabetes mellitus: a systematic review and meta-analysis. JAMA 300:2754–2764
Evans JM, Donnelly LA, Emslie-Smith AM, Alessi DR, Morris AD (2005) Metformin and reduced risk of cancer in diabetic patients. BMJ 330:1304–1305
Bowker SL, Majumdar SR, Veugelers P, Johnson JA (2006) Increased cancer-related mortality for patients with type 2 diabetes who use sulfonylureas or insulin. Diabetes Care 29:254–258
Currie CJ, Poole CD, Gale EA (2009) The influence of glucose-lowering therapies on cancer risk in type 2 diabetes. Diabetologia 52:1766–1777
Li D, Yeung SC, Hassan MM, Konopleva M, Abbruzzese JL (2009) Antidiabetic therapies affect risk of pancreatic cancer. Gastroenterology 137:482–488
Cazzaniga M, Bonanni B, Guerrieri-Gonzaga A, Decensi A (2009) Is it time to test metformin in breast cancer clinical trials? Cancer Epidemiol Biomarkers Prev 18:701–705
Decensi A, Puntoni M, Goodwin P, Cazzaniga M, Gennari A, Bonanni B, Gandini S (2010) Metformin and cancer risk in diabetic patients: a systematic review and meta-analysis. Cancer Prev Res Phila 3:1451–1461
Vigneri P, Frasca F, Sciacca L, Pandini G, Vigneri R (2009) Diabetes and cancer. Endocr Relat Cancer 16:1103–1123
Monami M, Lamanna C, Balzi D, Marchionni N, Mannucci E (2009) Sulphonylureas and cancer: a case-control study. Acta Diabetol 46:279–284
Acknowledgments
This work was supported by Associazione Italiana per la Ricerca sul Cancro (AIRC, bando 5 × 1,000 N°12182 and Progetto IG N° 11783), by European Community’s Seventh Framework Programme (EPC-TM net, project number 256974), by INAIL Research Grant and by a liberal donation by Angela Musazzi and Mario Stellato family.
Conflict of interest
Authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Perseghin, G., Calori, G., Lattuada, G. et al. Insulin resistance/hyperinsulinemia and cancer mortality: the Cremona study at the 15th year of follow-up. Acta Diabetol 49, 421–428 (2012). https://doi.org/10.1007/s00592-011-0361-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-011-0361-2