Abstract
Studies investigating the effect of leptin on bone mass were inconsistent and some related it to the effect of insulin. We intend in this cross-sectional study to investigate the effect of leptin on bone mass in type 1 diabetic patients. We recruited 42 patients with type 1 diabetes for which we determined weight, height, HbA1c, microalbuminuria, serum leptin, bone mineral content (BMC) and density (BMD), and body composition. The patients had an average age of 20.1 ± 0.6 years, an average body mass index (BMI) of 23.6 ± 0.5 kg/cm2 and an average duration of diabetes of 9.1 ± 1.0 years. The Z-score was not correlated with HbA1c or duration of the disease, and the average Z-score was not different in patients with microalbuminuria as compared to patients with no reported microalbuminuria. On the other hand, Z-score and BMC correlated negatively with leptin (r = −0.31; p = 0.04 and −0.60, p < 0.01, respectively). These correlations persisted after adjustment for fat mass. We conclude that not metabolic control of diabetes, but serum leptin has a negative effect on bone density in young patients with type 1 diabetes. This negative effect of leptin on bone density maybe, in part, due to deficiency of endogenous insulin secretion in these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The chronic nature of type 1 diabetes and its relatively early onset have always been a source of concern for the medical and psychological well being of the affected patients. The effect of this disease on bone density was studied [1–8]; however, there is still no conclusive evidence that type 1 diabetes is actually associated with a decreased bone density or an increased risk for fractures. Routine screening or initiation of preventive medications for osteoporosis in patients with type 1 or type 2 diabetes is not recommended at the present time [9]. Leptin a product of the ob gene was considered to be the link between fat and bone mass because it induces differentiation of the stromal cells toward the osteoblastic lineage [10] and because it affects numerous other endocrine functions such as thyroid and sex hormones [11]. Results of prior human studies investigating the effect of leptin on bone mass were inconsistent. Some studies failed to show any association [12–18], some showed positive association [15, 19–22] and conversely, others showed negative association [23–26].
It has been suggested that the effect of leptin on bone is linked to the effect of insulin [27, 28]. Indeed, the protective effect of leptin against bone loss in obese subjects is lost in the setting of insulin resistance [28]. We therefore hypothesized that the lack of endogenous insulin secretion in the setting of type 1 diabetes mellitus modulates the relationship between leptin and bone mass in these patients. The current study aimed at exploring the influence of leptin on bone density in patients with type 1 diabetes.
Subjects and methods
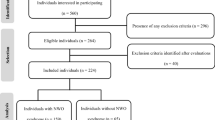
The study participants were recruited among patients who were followed up for type 1 diabetes at a referral center in Lebanon (The Chronic Care Center for Diabetes). From 266 patients with type 1 diabetes between the age of 18 and 22 years followed up at that center, only 42 patients (24 females and 18 males) were willing to participate in the study. All subjects were healthy type 1 diabetics, who were free of diseases and not taking medications known to affect bone health. All patients were pubertal with Tanner stage 5 for sexual development. Female patients were all menstruating with no history of prolonged amenorrhea of more than 3 months. At study entry, all subjects underwent physical examination including height (cm) and weight (kg) and body mass index was calculated (kg/m2). Blood was drawn for glycosylated hemoglobin (HbA1c) and fasting serum leptin levels. Glycosylated hemoglobin was done by the High Performance Liquid Chromatography (HPLC) method using a Variant kit (BIORAD). Plasma samples used for leptin determination were stored at −20°C and were not thawed until the leptin assay was performed. The quantitative detection of leptin levels was performed in duplicate using a commercially available human leptin Radioimmunoassay (RIA) kit (DRG Instruments GmbH, Marburg, Germany). The average was used in the analyses. The presence of microalbuminuria was assessed on a random spot urine sample using Tina-quant® Albumin (Roche Diagnostics GmbH, Indiana, USA). Total bone mineral content (BMC), total bone mineral density (BMD), as well as body composition including lean mass and fat mass were measured in the supine position by a dual-energy X-ray absorptiometry using LUNAR device. Total body age and gender specific Z-scores were automatically derived by the densitometer using the Western database provided by the manufacturer.
All patients signed a written informed consent before participating in the study, which was approved by the Institutional Review Board of the American University of Beirut.
Statistical methods
Independent-samples t test was used to compare means of continuous variables between two different groups. Correlations between the continuous variables such as BMC, Z-score, duration of the disease, HbA1c, weight, height, lean mass, and fasting serum leptin were assessed using the Pearson correlation coefficient. The correlation between bone parameters and serum leptin were assessed before and after controlling for fat mass. The mean Z-score was compared to zero using the one-sample t test, in order to determine whether bone mineral density in the study population was different from that of their healthy age matched western counterparts. P values <0.05 were considered significant. All values are reported as mean ± standard error of the mean (SEM). Statistical analysis was done using the SPSS version 13.0.
Results
The clinical, biochemical and densitometric characteristics of the study population are shown in Table 1. The mean age was 20.1 ± 0.6 years, the mean BMI was 23.6 ± 0.5 kg/cm2 and the mean duration of diabetes was 9.1 ± 1.0 years and the mean HbA1c was 7.7 ± 0.4. There was no significant difference between males and females in mean age, BMI, duration of DM or HbA1c. As expected, serum leptin levels and fat mass were higher in females (p < 0.01 and 0.05, respectively), whereas lean mass was higher in males (p < 0.01). Males had a higher areal total body BMC and BMD as compared to females (p < 0.01). The mean Z-score of the patients was 0.23 ± 1.1, which by one-sample t test, was not significantly different from zero, suggesting that total BMD of the study population was not significantly different from that of their age and gender matched healthy counterparts.
Relationship between bone parameters and diabetes
There was no significant correlation between Z-score and HbA1c or duration of the disease. When the study subjects were divided into two groups according to the presence or absence of albuminuria, the mean Z-score did not differ between the two subgroups. On the other hand, BMC correlated negatively with the duration of diabetes (R = −0.426; p < 0.05) but not with HbA1c or microalbuminuria (Fig. 1).
Relationship between bone parameters and leptin
There was a significant negative correlation between Z-score and leptin (r = −0.31; p = 0.04). This correlation persisted after controlling for fat mass (r = −0.35; p = 0.04).
Similarly, BMC correlated negatively with fasting serum leptin (R = −0.603; p < 0.01). The negative correlation between BMC and serum leptin persisted after controlling for fat mass (p < 0.01). When females and males were analyzed separately, and after controlling for fat mass, leptin correlated with BMC more strongly in females (R = −0.686; p < 0.01) than in males (R = −0.575; p = 0.051). The relationship between serum leptin level and total body BMC in the study population is shown in Fig. 2.
Discussion
This study showed that in patients with type 1 diabetes mellitus, average Z-score was neither significantly affected by the disease nor by the presence of microalbuminuria. Leptin correlated negatively with Z-score in the whole group and with total body BMC in both the genders, the correlation persisted after adjustment for fat mass.
Some studies have suggested that type 1 diabetes is associated with a modest reduction in BMD [1–5, 7], whereas others have found no effect on bone characteristics [4, 6, 7]. In a recent study assessing the prevalence and severity of bone disease in a cohort of young adult male with type 1 diabetic, Alexopoulou et al. [29] found that osteopenia and osteoporosis were present in 40 and 7% of the study population. In our study, BMC was negatively correlated with the duration of diabetes; the average Z-score of our young type 1 diabetic patients was not statistically different from zero. Therefore, a negative effect of type 1 diabetes on bone mass cannot be concluded. This finding is consistent with a study by Rozadilla et al. [6], which showed that bone loss might not represent a major problem in young type 1 diabetic patients with relatively shorter duration of disease. However, the negative correlation with the duration of the disease suggests that there is a risk of bone loss with age and therefore a risk of osteopenia or osteoporosis in adulthood, as it was reported by Alexopoulou et al. This requires further investigation through longitudinal studies. Previous studies also failed to show any association between microalbuminuria [5, 7] or metabolic control [3, 5, 7, 8, 30] and bone mineral density which is also consistent with our findings that neither the presence of microalbuminuria nor HbA1c were correlated with BMC or Z-score.
The effect of leptin on bone mass is still controversial. Few studies have supported the negative effect of leptin on bone density [23–26], whereas other studies showed that it has a positive effect on bone density [15, 19–22]. This effect seems to be different according to the pathway: central versus peripheral [31] and to the insulin level [27, 28]. Indeed, a study analyzing ob/ob mice demonstrated that leptin inhibits bone formation through a hypothalamic relay [31]. A study by Watanabe et al. [32] found that the troglitazone induced decrease in serum leptin is associated with the less bone loss in type 2 diabetes. Moreover, a recent study showed that in the setting of insulin resistance, high leptin level did not result in increased bone density in obese women [28]. Since our patients do not have adequate endogenous insulin secretion, we can hypothesize that the positive effect of leptin on bone might not be mediated by insulin per se but could be mediated by pro-insulin or C-peptide the lack of which resulted in the resistance of bone to leptin; and this is what caused this negative correlation between BMC and leptin. However, this hypothesis needs to be further investigated. On the other hand, the body composition and body fat content in patients with type 1 diabetes receiving insulin therapy may differ from that of healthy adolescents. Leptin is a polypeptide that is synthesized in adipose tissue. Therefore, insulin therapy may be of importance as a regulator of serum leptin levels and effect. Indeed, it has been previously shown that insulin is a potent stimulator of leptin expression in rodents [33].
Our study has some limitations. The cross-sectional design, the small sample size and the lack of information regarding lifestyle factors, which are important determinants of bone mass in adolescents, such as nutritional factors, calcium intake from dairy products and physical activity.
Nevertheless, we may conclude, based on our results and on all the above-mentioned studies, that metabolic control of diabetes (reflected in this case by HbA1c and microalbuminuria) does not significantly affect bone density in young type 1 diabetic patients and that serum leptin has a negative effect on bone in these patients which is probably in part due to the deficiency of endogenous insulin in these patients.
References
Levin ME, Boisseau VC, Avioli LV (1976) Effects of diabetes mellitus on bone mass in juvenile and adult-onset diabetes. N Engl J Med 294(5):241–245
McNair P, Christiansen C, Christensen MS, Madsbad S, Faber OK, Binder C, Transbol I (1981) Development of bone mineral loss in insulin-treated diabetes: a 1 1/2 years follow-up study in sixty patients. Eur J Clin Invest 11(1):55–59
Hui SL, Epstein S, Johnston CC Jr (1985) A prospective study of bone mass in patients with type I diabetes. J Clin Endocrinol Metab 60(1):74–80
Olmos JM, Perez-Castrillon JL, Garcia MT, Garrido JC, Amado JA, Gonzalez-Macias J (1994) Bone densitometry and biochemical bone remodeling markers in type 1 Diabetes Mellitus. Bone Miner 26(1):1–8
Miazgowski T, Czekalski S (1998) A 2-year follow-up study on bone mineral density and markers of bone turnover in patients with long-standing insulin-dependent diabetes mellitus. Osteoporos Int 8(5):399–403
Rozadilla A, Nolla JM, Montana E, Fiter J, Gomez-Vaquero C, Soler J, Roig-Escofet D (2000) Bone mineral density in patients with type 1 diabetes mellitus. Jt Bone Spine 67(3):215–218
Bartos V, Jirkovska A, Kasalicky P, Smahelova A, Vondra K, Skibova J (2001) Osteopenia and osteoporosis in diabetic women over 40 years of age. Cas Lek Cesk 140(10):299–301
Lopez-Ibarra PJ, Pastor MM, Escobar-Jimenez F, Pardo MD, Gonzalez AG, Luna JD, Requena ME, Diosdado MA (2001) Bone mineral density at time of clinical diagnosis of adultonset type 1 diabetes mellitus. Endocr Pract 7(5):346–351
Chau DL, Edelman SV, Chandran M (2003) Osteoporosis and diabetes. Curr Diabetes Rep 3(1):37–42
Thomas T, Gori F, Khosla S, Jensen MD, Buerguera B, Riggs BL (1999) Leptin acts on human marrow stromal cells to enhance differentiation to osteoblasts and to inhibit differentiation to adipocytes. Endocrinology 140:1630–1638
Thomas T, Burguera B (2002) Mini review: is leptin the link between fat and bone mass? J Bone Miner Res 17:1563–1569
Goulding A, Taylor RW (1998) Plasma leptin values in relation to bone mass and density and to dynamic biochemical markers of bone resorption and formation in postmenopausal women. Calcif Tissue Int 63:456–458
Rauch F, Blum WF, Klein K, Allolio B, Schonau E (1998) Does leptin have an effect on bone in adult women? Calcif Tissue Int 63:453–455
Kiel D, Harris T, Visser M, Hannan M, Wilson P (1999) Leptin and bone mineral density (BMD) in older men and women. J Bone Miner Res 14:475–765
Odabasi E, Ozata M, Turan M, Bingol N, Yonem A, Cakir B, Kutlu M, Ozdemir IC (2000) Plasma leptin concentrations in postmenopausal women with osteoporosis. Eur J Endocrinol 142:170–173
Martini G, Valenti R, Giovani S, Franci B, Campagna S, Nuti R (2001) Influence of insulin-like growth factor-1 and leptin on bone mass in healthy postmenopausal women. Bone 28:113–117
Ruhl CE, Everhart JE (2002) Relationship of serum leptin concentration with bone mineral density in the United States population. J Bone Miner Res 17:1896–1903
Johnstone AM, Murison SD, Duncan JS, Rance KA, Speakman JR (2005) Factors influencing variation in basal metabolic rate include fat-free mass, fat mass, age, and circulating thyroxine but not sex, circulating leptin, or triiodothyronine. Am J Clin Nutr 82(5):941–948
Matkovic V, Ilich JZ, Skugor M, Badenhop NE, Goel P, Clairmont A, Klisovic D, Nahhas RHW, Landoll JO (1997) Leptin is inversely related to age at menarche in human females. J Clin Endocrinol Metab 82:3239–3245
Iwamoto I, Oouchi T, Kosha A, Murakami M, Fujino T, Nagata Y (2000) Relationships between serum leptin level and regional bone mineral density, bone metabolic markers in healthy women. Acta Obstet Gynecol Scandinavica 79:1060–1064
Pasco JA, Henry MJ, Kotowicz MA, Collier GR, Ball MJ, Ugoni AM, Nicholson GC (2001) Serum leptin levels are associated with bone mass in nonobese women. J Clin Endocrinol Metab 86:1884–1887
Yamauchi M, Sugimoto T, Yamaguchi T, Nakaoka D, Kanzawa M, Yano S, Ozuru R, Sugishita T, Chihara K (2001) Plasma leptin concentrations are associated with bone mineral density and the presence of vertebral fractures in postmenopausal women. Clin Endocrinol 55:341–347
Ormarsdottir S, Ljunggren O, Mallmin H, Olofsson H, Blum WF, Loof L (2001) Inverse relationship between circulating levels of leptin and bone mineral density in chronic liver disease. J Gastroenterol Hepatol 16:1409–1414
Sato M, Takeda N, Sarui H, Takami R, Takami K, Hayashi M, Sasaki A, Kawachi S, Yoshino K, Yasuda K (2001) Association between serum leptin concentrations and bone mineral density, and biochemical markers of bone turnover in adult men. J Clin Endocrinol Metab 86:5273–5276
Blum M, Harris SS, Must A, Naumova EN, Phillips SM, Rand WM, Dawson- Hughes B (2003) Leptin, body composition and bone mineral density in premenopausal women. Calcif Tissue Int 73(1):27–32
Morberg C, Tetens I, Black E, Toubro S, Soerensen T, Pedersen O, Astrup A (2003) Leptin and bone mineral density: a cross-sectional study in obese and nonobese men. J Clin Endocrinol Metab 88(12):5795–5800
Kontogianni M, Dafni U, Routsias J, Skopouli F (2004) Blood leptin and adiponectin as possible mediators of the relation between fat mass and BMD in perimenopausal women. J Bone Miner Res 19:546–551
Abou Samra R, Baba N, Torbay N, Dib L, Fuleihan GE (2005) High plasma leptin is not associated with higher bone mineral density in insulin-resistant premenopausal obese women. J Clin Endocrinol Metab 90:2588–2594
Alexopoulou O, Jamart J, Devogelaer JP, Brichard S, de Nayer P, Buysschaert M (2006) Bone density and markers of bone remodeling in type 1 male diabetic patients. Diabetes Metab 32:453–458
Vina Simon E, Bueno Lozano G, Armada Maresca MI, Ruibal Francisco JL, Fernandez Perez C, Lozano Tonkin C, Casado de Frias E (2000) Bone mineral density in juvenile-onset diabetes mellitus. An Esp Pediatr 52(6):507–515
Ducy P, Amling M, Takeda S, Priemel M, Schilling AF, Beil FT, Shen J, Vinson C, Rueger JM, Karsenty G (2000) Leptin inhibits bone formation through a hypothalamic relay: a central control of bone mass. Cell 100:197–207
Watanabe S, Takeuchi Y, Fukumoto S, Fujita H, Nakano T, Fujita T (2003) Decrease in serum leptin by troglitazone is associated with preventing bone loss in type 2 diabetic patients. J Bone Miner Metab 21(3):166–171
Lönnqvist F, Arner P, Nordfors L, Schalling M (1995) Overexpression of the obese (ob) gene in adipose tissue of human obese subjects. Nat Med 1:950–953
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kassem, H.S., Arabi, A., Zantout, M.S. et al. Negative effect of leptin on bone mass in type 1 diabetes. Acta Diabetol 45, 237–241 (2008). https://doi.org/10.1007/s00592-008-0050-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-008-0050-y