Abstract
The aims of the study are (1) assessment of cell surface expression of adhesion molecules CD11b and CD62L on peripheral blood neutrophils in patients with type 2 diabetes and microangiopathy; (2) analysis of serum levels of soluble adhesion molecules: E-selectin (sE-selectin), soluble intercellular adhesion molecule-1 (sICAM-1), soluble vascular cell adhesion molecule-1 (sVCAM-1) and von Willebrand factor (vWF) and; (3) evaluation of systemic inflammatory markers like interleukin-6 (IL-6), soluble interleukin-6 receptor (IL-6Rs), high sensitivity C-reactive protein (hsCRP) and fibrinogen. Thirty patients with type 2 diabetes and microangiopathy were enrolled in the study. The study group was compared to 22 patients with type 2 diabetes without microangiopathic compliations. The control group included 20 healthy volunteers. Flow cytometry was used to analyse surface expression of adhesion molecules. Both inflammatory markers and soluble adhesion molecules were determined by immunoenzymatic assay. A significant increase in neutrophil surface CD11b expression (P < 0.01) as well as decrease in surface CD62L expression (P < 0.01) were observed in the group with diabetic microangiopathy in comparison with diabetic group without microangiopathic complications and healthy controls. Moreover, significantly higher concentrations of sICAM-1 (P < 0.05), sVCAM-1 (P < 0.05), sE-selectin (P < 0.05), vWF (P < 0.01), hsCRP (P < 0.01), IL-6 (P < 0.01) and fibrinogen (P < 0.001) were also found in patients with microangiopathy in comparison with the control group. IL-6Rs concentrations did not significantly vary between groups. We concluded (1) diabetic microangiopathy is accompanied by increase in CD11b expression and decrease in CD62L expression on peripheral blood neutrophils; (2) in diabetic microangiopathy rise in CD11b expression indicates neutrophil activation and intensified adhesion; (3) the development of diabetic microangiopathy is accompanied by an increase in soluble adhesion molecules and inflammatory markers concentrations in the blood.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In accordance with the latest views, a chronic, subclinical inflammatory process plays a key role in the development of diabetic vascular complications [1]. An increasing amount of data sugests leukocyte involvement in the pathogenesis of vascular lesions in diabetes [2–11]. Activation of leukocytes leads to their increased adhesion to the vascular wall and is also connected with increase in the production of a wide range of potentially cytotoxic factors (free radicals, TNF-α), factors damaging the vascular basement membrane (free radicals, metalloproteinases), factors activating an inflammatory process in vascular wall (IL-1, TNF-α, IFN-γ, arachidonic derivatives) or stimulating fibroblast proliferation (TGF-β, FGF, PDGF).
Increase in cellular adhesion and production of the above-mentioned factors in diabetes may lead to accelerated atherosclerosis development and small vessel lesion—a process typical for diabetic microangiopathy. Leukocyte adhesion to the endothelium is considered a key component in the process of leukocyte-associated vascular damage induction [2–5, 12, 13]. A central role in leukocyte adhesion and migration is played by adhesion molecules especially selectins (E-selectin, L-selectin), integrins and immunoglobulin superfamily molecules (ICAM-1, VCAM-1). These molecules and their ligands take part in a multistep leukocyte-endothelium interaction process [14]. Leukocyte surface L-selectin (CD62L) and endothelium surface E-selectin play a significant role at the initial “rolling leukocytes” stage of the process. Integrins are heterodimers containing alpha and beta subunits. Those containing identical beta subunits and differing in alpha structure are grouped into specific subfamilies, i.e. beta1, beta2, beta3 [14]. The MAC-1 integrin (CD11b/CD18), belonging to the beta2 subfamily binding ICAM-1 located on the endothelium cells. Leukocytes activation leads to increase in beta2-integrin expression, enabling permanent inter-cell contact. It is considered thad surface expression of beta2-integrin is a marker of leukocyte activation.
Until now, most studies analysing leukocytes’ role in the pathogenesis of diabetic vascular complications related to experimental diabetes in animal models [3–7, 15]. Less observations have been made in people. In a few studies higher beta2-integrin (CD11b/CD18) expression were confirmed on neutrophils and monocytes in patients with diabetes [16–18]. Most studies dedicated to leukocyte adhesion molecule expression referred to diabetic patients with atherosclerotic lesions [10, 17, 20, 21]. As opposed to macroangiopathy, scant studies provide data on adhesion molecule expression in the case of diabetic microangiopathy [11]. Furthermore, it remains unclear which factors in diabetes are responsible for increase in leukocyte surface beta2-integrin expression. No connection has been established between markers of metabolic balance in diabetes (glycaemia, HbA1c) and beta2-integrin expression [19, 22]. It must also be mentioned that not all authors have confirmed a rise in surface beta2-integrin expression on leukocytes in patients with diabetes [20, 21]. The obtained results can be affected by diabetes type, duration of the disease, vascular complications and level of metabolic balance.
In light of these facts, attempts were made to assess neutrophil activation in patients with type 2 diabetes and microangiopathic complications. Activation of neutrophils were analysed in context of selected markers of endothelial activation/dysfunction, systemic inflammatory markers as well as metabolic and clinical parameters of the disease.
The aims of the study wereo
-
1.
To assess surface CD11b expression (MAC-1 subunit belonging to the beta2-integrin subfamily) as well as surface CD62L (L-selectin) expression on peripheral blood neutrophils in patients with type 2 diabetes and microangiopathy.
-
2.
To analyse markers of vascular endothelium activation / dysfunction basing on serum levels of soluble adhesion molecules (sE-selectin), intercellular adhesion molecules (sICAM-1), soluble vascular cell adhesion molecule-1 (sVACM-1) and von Willebrand factor (vWF).
-
3.
To evaluate serum levels of inflammatory markers: interleukin-6 (IL-6), soluble interleukin-6 receptor (IL-6Rs), high sensitivity C-reactive protein (hsCRP) and fibrinogen.
Subjects and methods
Subjects
Thirty patients with type 2 diabetes and microangiopathic complications (retinopathy, nephropathy) were enrolled in the study (11 female and 19 male), aged from 40 to 65 years (mean 57.0 ± 5.9). Duration of the disease ranged from 5 to 30 years (mean 11.03 ± 8.50). The study group consisted of subjects with diabetic retinopathy (confirmed by ophtalmoscopy or fluorescein angiography) as well as diabetic nephropathy—at the microalbuminuric or proteinuric stage, with creatinin levels within normal range (<124 μmol/l). Microalbuminuria was diagnosed when two out of three tests performed during 6 months showed increase in albuminuria. The albumin/creatinin index was determined in a morning urine sample. Results above ≥30 μg/mg were considered abnormal. Results were deemed relevant only in patients free from diabetic metabolic imbalance and urinary tract infections. Criteria for proteinuria were set at protein levels of ≥0.5 g in a 24-h urine collection.
Considering that microalbuminuria in type 2 diabetes is not an entirely specific indicator of diabetic nephropathy, all patients enrolled into the study group with microalbuminuria underwent tests in order to confirm presence of diabetic retinopathy. In such context, microalbuminuria was regarded as an indicator of glomerular lesion in the course of diabetic nephropathy.
The study group was compared to patients with type 2 diabetes without microangiopathic compliations. This group was consisted of 22 patients with type 2 diabetes (10 female and 12 male), aged from 40 to 65 years (mean 56.0 ± 6.2), diabetes duration mean 5.32 ± 1.70 years. All patients enrolled into this group have normal albuminuria (<30 μg/mg), lack of retinopathy signs, ankle/brachial index within normal range (>1.0), normal ultrasound assessment of carotid arteries and no history and symptoms of cardiovascular disease.
Enrollment was conducted among patients hospitalised at the Department of Angiology, Hypertension and Diabetology of Wroclaw Medical University. Diabetes was diagnosed in accordance with current standards from the Polish Diabetologic Association [23]. To make certain that the assortment to the studied group concerned only the patients with type 2 diabetes, all of the patients on insulin had taken exclusively oral hypoglicaemic drugs for at least 6 years from the diagnosis of diabetes.
Exclusion criteria were: signs of infection or inflammation in the course of the last 3 months, ischemic heart disease, cerebrovascular lesions and other macroangiopathic complications, glucocorticosteroid or NSAID intake (except for ASA up to 325 mg/day), confirmed neoplastic disease, liver insufficiency, renal insufficiency (serum creatinin levels >124 μmol/l).
The control group included 20 healthy age- and sex-matched volunteers (9 female, 11 male) aged from 40 to 65 years (mean 55.4 ± 7.5).
Approval of the Ethics Committee of Wroclaw Medical University was obtained for conducting the study. Written informed consent was obtained from each patient.
Methods
Clinical evaluation
Based on body weight and height, the body mass index (BMI) was calculated [body mass (kg)/height2 (m)]. Blood pressure was measured in sitting position, at rest (mean of three measurements performed in 5-min intervals). All tests were performed from a single blood sample collected from the cubital vein after an overnight fast.
Staining cells with anti-CD11b/FITC, anti-62L/TC, anti-CD45/RPE
Three-milliliter blood samples were collected on heparin, then submitted to proper testing 30 min following sample collection. Neutrophils were identified by light and size scattering and using anti-CD45/RPE phycoerythrin-labeled monoclonal antibodies. In order to identify adhesion molecules on neutrophil surface, anti-CD11b/FITC fluorescein-labeled monoclonal antibodies, as well as anti-CD62L/TC “tricolor” monoclonal antibodies were applied. Isotype control antibodies IgG1/FITC/RPE and IgG1/TC were also used.
A measure of 5 μl anti-CD45/RPE, 5 μl anti-CD11b/FITC and 5 μl anti-CD62L/TC antibodies were added to 100 μl blood on heparin. Samples were incubated for 15 min in the dark at room temperature; 100 μl lysate were then added and incubated under similar conditions for another 10 min. Samples were then diluted with 1 ml distilled water and centrifuged (1,000×g, 10 min). After decanting the supernatant, samples were suspended in PBS and analysed by flow cytometry.
Assessing CD11b and CD62L expression
CD11b and CD62L expression was assessed by flow cytometry using DAKO Galaxy Flow Cytometer (Partec GmbH) and FloMax 2.3D software (Partec). Over 20,000 cells were submitted for analysis at each try. Surface expression of adhesion molecules was quantitated as mean channel fluorescence (MCF). Negative control for non-specific flow cytometric background was performed with an isotype-matched, fluorescent, non-binding monoclonal antibody.
Reagents
Antibodies as follows: anti-CD11b/FITC, anti-CD45/RPE, anti-CD62L/TC, IgG1/FITC/RPE, IgG1/TC from CALTAG Laboratories, Philadelphia, USA.
Determining serum levels of adhesion molecules
sE-selectin levels were determined by ELISA using an assay from R&D SYSTEMS, Minneapolis, USA (cat.nr BBE 2B); test sensitivity 0.1 ng/ml; intra- and inter-assay variation at 4.8 and 5.7%, respectively. sICAM-1 levels were evaluated by ELISA using an assay from Bender MedSystems GmbH, Vienna, Austria (cat. nr BMS201); test sensitivity 3.3 ng/ml; intra- and inter-assay variation at 4.1 and 7.66%, respectively. sVCAM-1 levels were assessed by ELISA using an assay from Bender MedSystems GmbH, Vienna, Austria (cat. nr BMS232CE) test sensitivity 0.59 ng/ml; intra- and inter-assay variation at 3.1 and 5.2%, respectively.
Determining serum levels of IL-6 and IL-6Rs
IL-6 levels were determined by ELISA using assay from Bender MedSystems GmbH, Vienna, Austria (cat. nr BMS213/2CE); test sensitivity 0.92 pg/ml; intra- and inter-assay variation at 3.4 and 5.2%, respectively. IL-6Rs levels were determined by ELISA using assay from Bender MedSystems GmbH, Vienna, Austria (cat. nr BMS214) test sensitivity 0.01 ng/ml; intra- and inter-assay variation at 1.7 and 2.2%, respectively.
Determining serum C-reactive protein (CRP) levels
CRP levels were determined by ELISA using a high-sensitivity assay from DRG International, Inc., USA (cat. nr EIA-3954); test sensitivity 0.1 mg/l; intra- and inter-assay variation at 2.3–7.5% and 2.5–4.1%, respectively.
Determining plasma von Willebrand factor levels
vWF levels were determined by ELISA using assay from Asserachrom vWF, Diagnostica Stago; Asnieres, France, test sensitivity 2%; intra- and inter-assay variation at 5.8–6.3% and 3.0–7.2%, respectively. The remaining biochemical tests were routinely conducted in a clinical laboratory. Blood counts were performed using a16-parameter automatic hematology analyzer ABX MICROS 60 OT, from ABX Diagnostics, France. Concentrations of the following parameters were assessed: glucose (using an enzymatic assay from Analco Medical Trade), insulin (using the Microparticle Enzyme Immunoassay from ABBOTT), HbA1c (by immunoturbidimetry, using UNIMATE HBA1C from Roche), lipid levels (using Liquick enzymatic assay from Cormay), fibrinogen (using Behring Coagulation Timer). Basing on obtained insulin and fasting glucose levels, the insulin resistance index (HOMA IR) was calculated (HOMA Calculator v2.2 -http://www.dtu.ox.ac.uk).
Statistics
Results were expressed as means ± standard deviation. Comparisons between diabetic patients and healthy controls were performed using the Wilcoxon signed rank test. Correlation was tested using Spearman’s Rank Correlation. All statistical analyses were performed using Statistica 7.1 (StatSoft, Inc.). For all analyses, significance was defined as a P value <0.05.
Results
Clinical profile
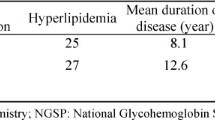
Selected clinical and laboratory parameters as well as treatment programs are located in Tables 1, 2. Higher BMI, systolic blood pressure, glucose, triglyceride, HbA1c levels and lower serum HDL levels were found in diabetic patients in comparison with healthy controls. Significantly higher leukocytosis were also observed in both diabetic groups.
CD11b and CD62L expression on neutrophil surface
Significantly higher surface expression of CD11b was found in patients with microangiopathy in comparison with healthy volunteers and patients with diabetes without microangiopathic complications. There were no differences in CD11b expression between diabetes without microangiopathy and controls. While surface expression of CD62L on neutrophils in patients with diabetic microangiopathy was significantly lower than in controls and patients with diabetes without microangiopathic complications (Table 3).
Soluble adhesion molecule and vWF levels
In patients with microangiopathy, sICAM-1, sVCAM-1, sE-selectin and vWF concentrations were significantly higher than those of the control group. Moreover, an increase in sICAM-1 and sVCAM-1 concentrations were observed in patients with microangiopathy in comparison with diabetes without microangiopathic complications (Table 2).
Concentrations of inflammatory markers
HsCRP and IL-6 levels were significantly higher in both diabetic groups than in controls. In patients with microangiopathy fibrinogen level was elevated in comparison with controls. IL-6Rs concentrations did not significantly vary between groups (Table 2).
Parameter correlations
In the group of patients with microangiopathy, a positive correlation was established between neutrophil surface CD11b expression and serum sICAM-1 concentration (ρ = 0.46; P < 0.05) as well as a negative correlation between CD11b expression and duration of diabetes (ρ = −0.41; P < 0.05). The degree of proteinuria significantly correlated with sICAM-1 (ρ = 0.53; P < 0.01) and sE-selectin (ρ = 0.42; P < 0.05) levels. A strong positive correlation was found between sE-selectin and sICAM-1 levels (ρ = 0.6; P < 0.001). The concentration of sVCAM-1 correlated with HbA1c values (ρ = 0.52; P < 0.01). Analysing all study subjects together, a positive correlation between leukocytosis and BMI was established (ρ = 0.31; P < 0.01).
Discussion
In our study subjects, a significant increase in surface CD11b expression on peripheral blood neutrophils (PMNs) was demonstrated. This findings indicate increased activity of PMNs in patients with type 2 diabetes complicated by microangiopathy. Basing mostly on observations from experimental diabetes in animal models, it is possible that the elevated CD11b expression on PMNs surface, as shown in our study, may have impact on the development of microangiopathic complications in diabetes. Joussen et al. [4] proved that, in diabetic animal models, retinal leukocyte (granulocyte and monocyte) adhesion is responsible for endothelial cell damage and necrosis. It has also been proved that leukocyte-surface beta2-integrin and endothelium-surface ICAM-1 molecules are involved in leukocyte adhesion. Similarly, it has also been demonstrated that the administration of anti-beta2-integrin and anti-ICAM-1 antibodies reduces leukocyte adhesion to vessel walls, also limiting retinal leukostasis (entrapment of leukocytes in the retinal microcirculation) and preventing endothelial damage. Barouch et al. [3], likewise, demonstrated increase in surface beta-integrin (CD11b, CD18) expression on PMNs in experimental diabetic animal models, together with increased retinal adhesion. In vitro administration of specific anti-CD18 and anti-CD11b antibodies inhibited the increase in PMNs adhesion. A similar inhibitory effect was obtained in vivo following anti-CD18 administration. Increased adhesion of PMNs in the choroid was also reported in diabetic humans, these changes being very similar to those found within the retina [24]. It may be possible that PMNs activation, as observed in our study, may correspond to an increase in PMNs adhesion, thus contributing to the progression of diabetic retinopathy.
After thorough analysis of the available data, no studies were found concerning neutrophil surface CD11b expression in patients with type 2 diabetes complicated by microangiopathy. This probably is the first report unequivocally documenting the increase in surface expression of the adhesion molecule CD11b, leukocyte activation marker in patients with type 2 diabetes and microangiopathy complications (retino- and nephropathy).
Meanwhile, neutrophil surface CD62L (L-selectin) expression in the study group was significantly lower in comparison with the control group. This should be linked with neutrophil activation, as leukocyte stimulation occurs with concomittant reduction in surface L-selectin expression [2, 14, 25]. Following activation, L-selectin molecules are removed from the leukocyte surface through proteolysis and appear in peripheral blood as “soluble” forms [25]. MacKinnon et al. [2] noted a reduction in CD62L (L-selectin) expression on lymphocytes in a study concerning patients with type 1 as well as type 2 diabetes and retinopathy. They also demonstrated that lymphocytes from patients with retinopathy show increased adhesion to the endothelium in vitro. The authors link decrease in L-selectin expression with lymphocyte activation and augmented retinal adhesion. Our observations converge with these data. Although our study did not concern lymphocytes, similar lower CD62L expression was observed on PMNs. It may be presumed that reduced L-selectin expression in patients with microangiopathy derives from PMNs activation, a fact corroborated in this study by an demonstrated increase in CD11b expression (a leukocyte activation marker) (Fig 1).
The obtained results concur with current outlooks stating that microangiopathy development is linked with an underlying, low-intensity chronic inflammatory process involving leukocyte activation, augmented endothelial adhesion and entrapment of leukocytes in the microcirculation [4, 5]. Furthermore, higher serum IL-6, hsCRP and fibrinogen levels (but within normal range) in microangiopathic patients, as compared to healthy controls, confirm a systemic subclinical activation of inflammatory processes. Similarly increased surface CD11b expression reflects PMNs activation. Remarkably, there is absence of correlations between CD11b / CD62L expression and selected inflammatory markers (hsCRP, fibrinogen, IL-6, IL6Rs). This indicates that analysis of systemic inflammatory markers does not correspond to PMNs activation.
Furthermore, significantly higher serum levels of sE-selectin, sICAM-1, sVCAM-1 and vWF were found in the study group, which undoubtedly reflects endothelial activation/damage in diabetic microangiopathy. A simultaneously observed PMNs activation process suggests their increased endothelial adhesion. Moreover, a significant positive correlation between CD11b expression (beta2-integrin subunit) on PMNs and serum sICAM-1 level was established in patients with diabetic microangiopathy. The ICAM-1 molecule is an endothelial receptor for beta2-integrins and participates in leukocyte adhesion to the vascular wall. The above correlation indirectly shows a link between PMNs activation and endothelial activation/dysfunction in studied patients.
At this point, the question arises “Which factor is responsible for PMNs activation in diabetic angiopathy?” The level of PMNs activation, reflected by CD11b expression, did not correlate with metabolic balance in diabetes (glycaemia, HbA1c, insulinaemia), BMI or with blood pressure values. This lack of correlation between leukocyte activation and metabolic parameters in patients with microangiopathy has also been confirmed in other studies [19, 22]. Thus, the nature of the factors responsible for PMNs activation in diabetic microangiopathy remains unclear. PMNs activation may primarily occur in areas of damaged microcirculation under the influence of local factors. Under these conditions, a certain quantity of PMNs remains trapped in capillaries, while the rest remain accessible for evaluation in peripheral blood. The link between increased CD11 expression and the presence of microangiopathy may be confirmed by lack of differences in CD11 expression between patients with diabetes without microangiopathy and control group. The increased CD11b expression on PMNs was observed only in patients with microangiopathy and was significantly elevated in comparison with both diabetes without microangiopathic complications and control group. The increase in CD11b expression isn’t related to presence of diabtes per se. Altough diabetes duration in patients with microangiopathy was significantly longer than in patients without microangiopathic complications but it doesn’t explain an increase in CD11b expression on PMNs due to negative correlation observed between CD11b expression and duration od diabetes in our study.
Reassuming, in patients with microangiopathy, the activation of inflammatory mechanisms was confirmed, reflected by an increase in systemic levels of IL-6, hsCRP and fibrinogen. Simultaneously, activation of PMNs in peripheral blood was demonstrated, as shown through higher surface expression of CD11b, thus indicating increased PMNs adhesion to vessel walls. Lower CD62L (L-selectin) expression was also determined in PMNs from patients with microangiopathy. This probably is the consequence of a natural process, removing L-selectin from PMNs’ cell surface following their activation. Raised levels of markers of endothelial activation/dysfunction (sE-selectin, sICAM-1, sVCAM-1 and vWF) were also found in the study group, a fact which additionally correlated with PMNs activation level and degree of microangiopathy. This is confirmed by a positive correlation between PMNs surface CD11b expression and sICAM-1, as well as the interdependence between sE-selectin and sICAM-1 concentrations and degree of proteinuria.
References
Bullo M, Garcia-Lorda P, Megias I, Salas-Salvado J (2003) Systemic inflammation, adipose tissue tumor necrosis factor, and leptin expression. Obes Res 11:525–531
MacKinnon JR, Knott RM, Forrester JV (2004) Altered L-selectin expression in lymphocytes and increased adhesion to endothelium in patients with diabetic retinopathy. Br J Ophthalmol 88:1137–1141
Barouch FC, Miyamoto K, Allport JR (2000) Integrin-mediated neutrophil adhesion and retinal leukostasis in diabetes. Invest Ophthalmol Vis Sci 41:1153–1158
Joussen AM, Poulaki V, Le ML et al (2004) A central role for inflammation in the pathogenesis of diabetic retinopathy. FASEB J 18:1450–1452
Adamis AP (2002) Is diabetic retinopathy an inflammatory disease? Br J Ophthalmol 86:363–365
Sassy-Prigent C, Heudes D, Mandet C et al (2000) Early glomerular macrophage recruitment in streptozotocin-induced diabetic rats. Diabetes 49: 466–475
Chow FY, Nikolic-Paterson DJ, Atkins RC, Tesch GH (2004) Macrophages in streptozotocin-induced diabetic nephropathy: potential role in renal fibrosis. Nephrol Dial Transplant 19:2987–2996
Heinzelmann M, Mercer-Jones MA, Passmore JC (1999) Neutrophils and renal failure. Am J Kidney Dis 34:384–399
Galkina E, Ley K (2006) Leukocyte recruitment and vascular injury in diabetic nephropathy. J Am Soc Nephrol 17:368–377
Fusman R, Rotstein R, Zeltser D et al (2001) The state of leukocyte adhesiveness/aggregation in the peripheral blood of patients with type 2 diabetes and ischemic vascular disease. Acta Diabetol 38:43–49
Rao KM, Hatchell DL, Cohen HJ (1997) Alterations in stimulus-induced integrin expression in peripheral blood neutrophils of patients with diabetic retinopathy. Am J Med Sci 313:131–137
Ruberg FL, Loscalzo J (2004) Inflammation and atherothrombosis. In: Loscalzo J (ed) Molecular mechanisms of atherosclerosis. Taylor & Francis, London, pp 45–60
Wierusz-Wysocka B, Zozulińska D, Wysocki H (2002) Odczyn zapalny w patogenezie mikro- i makroangiopatii cukrzycowej. Diabetologia 1:56–62
Gołąb J (2005) Krążenie limfocytów. In: Jakóbisiak M (ed) Immunologia. PWN, Warszawa, pp 103–117
Schröder S, Palinski W, Schmid-Schönbein GW (1991) Activated monocytes and granulocytes, capillary nonperfusion, and neovascularization in diabetic retinopathy. Am J Pathol 139:81–100
Oostrom AJ, Wijk JP, Sijmonsma TP et al (2004) Increased expression of activation markers on monocytes and neutrophils in type 2 diabetes. Neth J Med 62:320–324
Berliner S, Rogowski O, Rotstein R, Fusman R et al (2000) Activated polymorphonuclear leukocytes and monocytes in the peripheral blood of patients with ischemic heart and brain conditions correspond to the presence of multiple risk factors for atherothrombosis. Cardiology 94:19–25
Delamaire M, Maugendre D, Moreno M et al (1997) Impaired leukocyte functions in diabetic patients. Diabet Med 14:29–34
Grykiel K, Zozulińska D, Kostrzewa A et al (2001) Ocena ekspresji receptorów powierzchniowych na granulocytach obojętnochłonnych u chorych na cukrzycę typu 1. Pol Arch Med Wewn 5:377–381
Caimi G, Montana M, Ferrara F et al (2003) Polymorphonuclear leukocyte integrin pattern, at baseline and after activation, in type 2 diabetic subjects with macrovascular complications. Acta Diabetol 40:14–19
Danielsson P, Truedsson L, Eriksson K-F, Norgren L (2005) Inflammatory markers and IL-6 polymorphism in peripheral arterial disease with and without diabetes mellitus. Vasc Med 10:191–198
Fogelstrand L, Hulthe J, Hulten LM et al (2004) Monocytic expression of CD14 and CD18, circulating adhesion molecules and inflammatory markers in women with diabetes mellitus and impaired glucose tolerance. Diabetologia 47:1948–1952
Zalecenia kliniczne dotyczące postępowania u chorych na cukrzycę (2005) Stanowisko Polskiego Towarzystwa Diabetologicznego. Diabetologia Doświadczalna i Kliniczna 2004; 4, sup.E
Lutty GA, Cao J, McLeod DS (1997) Relationship of polymorphonuclear leukocytes to capillary dropout in the human diabetic choroid. Am J Pathol 151:707–714
Smalley DM, Ley K (2005) L-selectin: mechanisms and physiological significance of ectodomain cleavage. J Cell Mol Med 9:255–266
Declaration of competing interests
None to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mastej, K., Adamiec, R. Neutrophil surface expression of CD11b and CD62L in diabetic microangiopathy. Acta Diabetol 45, 183–190 (2008). https://doi.org/10.1007/s00592-008-0040-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-008-0040-0