Abstract
Background
To compare the clinical outcomes between isolated cruciate ligament reconstruction (ACLR) and combined ACL with anterolateral ligament reconstruction in chronic ACL injury especially with rotary instability problem.
Methods
Systematic searches were conducted of literature published up to July 2021 on PubMed, Google Search, and Cochrane databases for studies comparing isolated ACLR and ACL with anterolateral reconstruction. Two reviewers independently determined eligibility, extracted outcome data, and assessed the risk of bias of eligible studies. Pooled clinical outcomes used random effects with mean differences and risk ratio for continuous and dichotomous variables, respectively.
Results
After excluding 49 articles based on full-text screening, six studies were identified which met the inclusion criteria in the meta-analysis. Clinical outcomes such as residual laxity, rotatory instability, and graft failure were compared between isolated ACLR and combined ACL and anterolateral stability reconstruction. Overall, both clinical outcomes of isolated ACL and combined ACL with anterolateral reconstruction show improvement results in pivot shift test, the absence of residual laxity and incidence of graft failure. Compared to isolated ACLR, the prominent postoperative result was by combined ACL with anterolateral reconstruction which had significant differences in laxity outcome based on (I2 = 89%, p < 0.00001) and (MD = 0.71, 95%CI: 0.33–1.08, p = 0.00002).
Conclusions
The combined ACL with anterolateral reconstruction tended to have superior clinical outcomes, especially in the absence of residual laxity, compared to the isolated ACLR, but the other results were not significantly different statistically. Combined ACL and anterolateral reconstruction were not performed routinely for patients undergoing ACL reconstruction, but more suitable for chronic rotatory instability problem.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical techniques of the anterior cruciate ligament reconstruction (ACLR) are aimed not only to restore the anatomy of the native ACL, but also to improve functional stability of the injured knee and prevent secondary damage to cartilage and meniscus [1,2,3]. Although the knowledge progress of ACL injury and techniques for ACLR resulted in long-term outcomes that are generally favorable, persistent rotational instability and graft rupture remain serious concerns of most orthopedic surgeon [1, 2, 4].
The primary function of ACL is to restrain the anterior translation at all flexion angles of the knee and also during internal rotation at flexion angles less than 35°. The Anterolateral ligament (ALL) is a secondary stabilizer for the ACL, preventing anterolateral tibial translation and internal rotation, especially at 30°–90° of knee flexion. The presence of a positive high grade of pivot shift phenomenon after ACLR is caused by inadequate restoration of rotational knee stability [2, 4,5,6,7]. It was reported that 25% of patients may have a residual pivot shift after ACLR that reaffirms the theory that it is common to have tears of secondary restraints such as the ligamentous and capsular structures of the lateral compartment [8].
Recently, the good clinical results of a surgical technique that combined ACL and ALL grafts have been published from several comparative studies which have demonstrated that concomitant ALL reconstruction (ALLR) is associated with a significantly reduced risk of ACL graft rupture and improved knee stability [1, 2, 4,5,6,7]. Several studies that reported combined ACL and ALL reconstructions in a high-risk population found a lower graft rupture rate, improvement in rotational and anteroposterior stability than the isolated ACL reconstructions that used a bone-patellar tendon-bone graft or a quadrupled hamstring tendon graft [8]. Although promising outcomes after combined intra-articular and extra-articular ACLR have been reported, advance research is still needed to prove the ALL may need to be reconstructed in cases of residual rotatory laxity after ACLR to improve rotational stability.
This study aimed to produce a systematic review and meta-analysis about clinical outcomes between combined ACL and ALL reconstruction compared to isolated ACL reconstruction, especially in rational stability, knee function and incidence of re-rupture graft based on the published literature.
Material and methods
Review of protocol
Review question of this study was “How are the clinical outcomes from combined ACL and ALL reconstruction compared to isolated ACL reconstruction and what is the incidence rate of graft failure or re-rupture?”
Outcome measure
This study assessed the clinical outcomes based on: (1) Evaluation of rotational stability of knee joint, (2) Evaluation of objective knee function, and (3) Evaluation of incidence rate of graft failure or re-rupture.
Literature search and study selection
In June 2021, we conducted a literature search from online databases using Cochrane library, PubMed (Medline), Web of Science, and Google Search to select and identify all studies published in English which describe the comparation of clinical outcomes between isolated ACL reconstruction and combined ACL with ALL reconstruction. All studies were reported based on the Preferred reporting items for systemic reviews and meta-analyses (PRISMA) statement [9].
We used the following keywords for the literature search: “ACL”, “Anterior cruciate ligament”, “ALL ligament”, “Anterolateral ligament” “isolated ACL reconstruction”, “Combined ACL and ALL reconstruction”, “outcome”, “re-rupture”, “graft failure” and various combinations using the “AND”, “OR”, or “VERSUS”.
Eligibility criteria
Inclusion criteria of the study were: (1) Articles publish in English, (2) Articles on isolated ACL reconstruction, (3) Articles on combined ACL and ALL reconstruction, (4) Articles which describe comparison outcome isolated ACL reconstruction and combined ACL and ALL reconstruction (5) Articles that describe laxity after surgery using KT1000 tests, (6) Articles that describe the pivot shift test after surgery, and (7) Articles that describe the graft failure or re-rupture after surgery. Articles that met these inclusion criteria were included in this systematic review. Non-English articles, articles on multiple ligament reconstruction, duplicate articles, literature reviews, articles on studies in vitro and cadaveric, biomechanical study, letters to editors, instructional courses were excluded. All articles with incomplete information on diagnosis, imaging, arthroscopic or surgical assessment of the associated lesions, clinical examination, follow-up duration, clinical postoperative outcomes, and no statistical analysis were also excluded.
Data extraction
To avoid bias, the following data were identified and recorded independently by all of the investigators: study design, types of graft, types of surgical technique, outcome after surgery, degree of rotational stability, degree of laxity, interventions, comparisons, duration of follow-up, and complications.
Methodological quality assessment and risk of bias
The methodological quality of the included studies was assessed using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [9]. Two authors (M.W.A and S.R.) independently performed all of the assessments. Coleman methodology score (CMS) was used to quantify the quality of the article. The article’s methodology was assessed by CMS with a total score ranging from 0 to 100. The higher the CMS score of the article indicated the more valid the article because it lacked biases and confounding factors. To avoid selection bias, the included and excluded articles were reviewed and re-assessed by all authors. If there was any disagreement between the authors, the problem was resolved by S.R as the senior investigator.
Data synthesis
We used RevMan 5 software (Version 5.3, the Cochrane Collaboration) and Stata 12.0 software for meta-analysis in the statistical analyses. The 95% Confidence interval (CI) and Mean difference (MD) were counted for continuous data. The Odds Ratio (OR) and 95% CI were calculated for dichotomous data. An alpha level of < 0.05 was considered statistically significant. The heterogeneity among the included studies was tested using the I-square tests and chi-square tests. The chi-square test was performed to quantify heterogeneity significance. The I-square test was performed to quantify the estimation of variability in the effect that occurred because of its heterogeneity. The result interpretation of the chi-square test was quantified based on the Cochrane Handbook of Systemic Reviews. The result has its interpretation (0–40%, might not be important; 40–60%, may represent moderate heterogeneity; 60–90%, may represent substantial heterogeneity; and 90–100%, considerable heterogeneity). When no significant heterogeneity was present (I2 < 50%, P > 0.1), the fixed-effect model was used. If the result was significant heterogeneity, we used a random effect model.
Results
Study selection
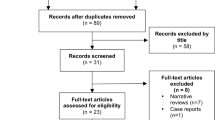
A total of 85,000 articles were obtained from the database literature search and 74,300 were excluded based on the title or due to duplication. A total of 10,700 articles were eligible for further screening. There were 10,643 articles excluded because they did not match the inclusion criteria resulting in a total of 57 articles. Next, there were 49 articles excluded after the full-text screening was performed and last study selection we found six articles meet the criteria for meta-analysis study. We excluded these articles due to nonoriginal articles, nonoperative study and were not in accordance with the criteria inclusion and exclusion of this study. The flowchart of the article is shown in Fig. 1.
Demographics and characteristics of selected studies
The six studies consist of two retrospective studies, three randomized control trials studies, and one case control study. All of this studies met the requirements and then included in the systematic review and meta-analysis. The total of 683 patients were divided into 375 patients in group I (isolated ACLR) and group II (combined ACL and ALLR). The mean of age in group I was 27.5 years old (25–33) and the group II was 26.8 years old (24–33). The mean onset of injury before the patient got surgical reconstruction was 6 months (3–14) in group I and 7 months in group II (3–15), while the mean follow-up time after surgical reconstruction both group I and group II were 29 months (24–60). The characteristics of the included studies are shown in Table 1.
Outcome measurements, detailed graft type, and fixation techniques from the studies are listed in Table 2. Based on Table 2, we compared and evaluated the outcome measurements of each study which met the criteria outcome of this study especially pivot shift test, KT-1000, and incidence of graft failure or rupture between group I and group II. In group I graft was harvested from hamstring tendon in five studies and only one study was using BTB, while techniques in group II always used hamstring tendon. The graft thickness all of studies was designed in double until quadruple and fixation graft methods were using interference screw or button.
Residual pivot shift test
The outcome of the pivot shift test was grouped into four categories: normal, grade 1 (glide), grade 2 (clunk), and grade 3 (gross). Overall, six studies showed no different outcome in pivot shift test. A fixed-effects model was applied because a low statistical heterogeneity was observed (I2 = 0%, p = 0.52), (I2 = 0%, p = 0.71), (I2 = 0%, p = 0.52), and (I2 = 0%, p = 0.79), respectively. There was no significant difference in re-rupture graft in both group 1 and group 2 based on (MD = 0.37, 95% CI [0.19, 0.73], p = 0.004), (MD = 1.89, 95% CI [0.94, 3.83], p = 0.008), and (MD = 4.10, 95% CI [0.84, 20.00], p = 0.008) as show in Figs. 2, 3, 4, 5.
Instrumented knee laxity testing using KT-1000 arthrometer
The outcomes of the KT-1000 tests were grouped into three categories: < 3 mm, between 3 and 5 mm, and > 5 mm. All of studies evaluated residual laxity using the KT-1000 arthrometer measurement. We used a random effect model because a statistical heterogeneity was observed (I2 = 89%, p < 0.00001). There was a significant difference in laxity outcome between the group 1 and group 2 based on KT-1000 (MD = 0.71, 95% CI [0.33, 1.08], p = 0.00002). This finding shows that the laxity outcome was significantly higher in the group 1 than in the group 2 after surgery (Fig. 6).
Graft rupture rate
Re-rupture was described in this study and there was no significant difference between groups within the study findings. A fixed-effects model was applied because a low statistical heterogeneity was observed (I2 = 0%, p = 0.99). There was no significant difference in re-rupture graft in both group 1 and group 2 based on (MD = 7.06, 95% CI [2.29, 21.76], p = 0.00002) as shown in Fig. 7.
Risk of bias assessment
The risk of bias summary and graph are described in Figs. 8, 9.
Discussion
Various studies have been used to evaluate clinical outcome of combined ACL and ALL reconstruction using hamstring and BTP tendons as grafts. The final results did not completely support this study’s hypothesis in that the only significant difference noted was in the instrumented knee laxity testing results. This finding might indicate that ALL reconstruction should not be performed routinely for patients undergoing ACL reconstruction. The fact that better anterior stability on instrumented knee laxity testing was found in group 2 supports the findings of previously published biomechanical studies about the ALL. During the past few decades, ACL reconstruction has significantly advanced. Surgeons and scientists are working hard on improving the functional outcomes and quality of life of patients with ACL injuries. Excellent results were obtained with such development; however, rotational instability remains an issue in a large minority of patients. Because single-bundle ACL reconstruction does not completely restore the normal kinematics of the knee, double-bundle reconstruction was introduced. Double-bundle ACL reconstruction has achieved superior biomechanical stability of the knee. Nevertheless, rotational instability has still not been fully resolved with this technique. Surgeons have therefore combined ACL reconstruction with lateral extra-articular augmentation to overcome this problem. This adaptation was found to be more effective in recovering lateral rotational stability of the knee when combined with ACL reconstruction. By adding lateral extra-articular augmentation to reconstructive surgery of the ACL, internal rotation of the tibia at 300 of knee flexion was reduced more significantly compared with either single-bundle or anatomic double-bundle reconstruction. Recently, techniques for reconstruction of the ALL of the knee have been developed after gaining better understanding of its anatomy. This effort was made to ensure rotational stability in patients after ACL reconstruction. In a case series of patients with combined ACL and ALL reconstruction, significant improvements were observed in objective and subjective outcomes at a mean follow-up of 32.4 months. From analysis statistic did not reveal statistically significant difference in physical examination finding especially pivot shift test; however, a higher percentage of normal results was observed among the patients who underwent combined ACL and ALL reconstruction. A recently published biomechanical study had demonstrated that the load-bearing ability of the ALL in an ACL-intact knee was minimal in response to the simulated anterior drawer, Lachman, and pivot shift tests. Nevertheless, in the ACL-deficient knee, the load-bearing ability of the ALL increased to nearly sixfold in response to the anterior drawer and Lachman tests and to threefold in response to the pivot shift test. In the ACL-deficient knee, anterior translation increased by 2 to 3 mm on all the three simulated tests after sectioning the ALL. These biomechanical findings proved the importance of the ALL in anterior and rotational stability of the knee joint [2, 10,11,12, 17,18,19,20,21].
Patients with chronic ACL injury who underwent combined intra- and extra-articular reconstruction showed better pivot shift and improvements in the functional outcome scores when compared to those submitted to isolated intra-articular reconstruction. In this way, they may benefit from this type of reconstruction. Chronic ACL injuries present a difference in relation to the acute injuries, because they show a higher anterolateral laxity. The instability is due to an anterior asymmetrical translation of the lateral tibial plateau. When there is injury or insufficiency of anterolateral structures, either by acute injury that does not heal properly or by the loosening resulting from an untreated ACL injury, isolated ACL reconstruction does not re-establish normal knee kinematics; thus, something more is required to treat these patients. Ferretti et al. described 90% of ALL injury while exploring acute ACL injury and the healing potentials of ALL are yet unknown, but will give residual pivot shift and does not heal adequately without surgery [6, 7, 10, 15, 19,20,21].
Regarding graft failure, this study concludes there was a nonsignificant differentiation between both groups based on the statistical analysis. Cotter et al. concluded that combined ACL and ALL reconstruction had 2.5-fold lower odds of failure than reconstruction of the patellar tendon and 3.1-fold lower odds than with hamstrings tendons. Trojani et al. showed that adding the extra-articular reconstruction decreases the failure rate by more than 50%. As mentioned before, augmentation using ALL cannot be performed routinely for every case, but this procedure was suitable for ACL reconstruction in patients with ligamentous laxity. Larson et al. showed that patients with hypermobility had a 24.4% failure rate, with rates of 25% for hamstrings tendons, and 21.1% for the patellar tendon. Rosenstiel et al. described the combined ACL and ALL reconstruction is associated with excellent outcomes in professional athletes with respect to graft rupture rates, return to sport, knee stability, and reoperation rates after injury [67, 13, 14, 16, 20, 21].
Limitations
There are several limitations of the present meta-analysis. First, the quality of the available studies is low. The three RCTs, two retrospective and one case control study described only 683 patients, which is low, considering the high incidence of ACL injury. Variations in study design, patient characteristics, sample size, reporting of outcome, and postoperative protocol resulted in high heterogeneity between the studies.
Second, we did not serially investigate outcome measurement, especially for long-term follow-up which may have indicated some complications such as graft loosening, implant breakage, or revision surgery might occur after 5 years. More studies investigating the long-term follow-up are needed to prove the reliability of this new technique and implants.
Conclusions
In this systematic review and meta-analysis, with a limited sample and follow-up period, we concluded that combined ACL and ALLR tended to have superior clinical outcomes, especially the absence of residual laxity, compared to the isolated ACLR based on measurement residual laxity using the KT-1000 arthrometer, but the other results showed no significant differences statistically. Combined ACL and anterolateral reconstruction were not performed routinely for patients undergoing ACL reconstruction, but is indicated more suitable for chronic rotatory instability problem. However, combined ACL and ALL reconstruction gave effective results in improving objective outcomes and no serious complications. We recommend future long-term follow-up studies comparing combined ALL and ACL reconstruction with other techniques of ACL reconstruction among patients with different demographic features.
References
Erden T, Toker B, Toprak A, Taşer O (2021) Comparison of the outcomes of isolated anterior cruciate ligament reconstruction and combined anterolateral ligament suture tape augmentation and anterior cruciate ligament reconstruction. Jt Dis Relat Surg 32(1):129–136. https://doi.org/10.5606/ehc.2020.78201
Ibrahim SA et al (2017) Anatomic reconstruction of the anterior cruciate ligament of the knee with or without reconstruction of the anterolateral ligament. Am J Sports Med 45(7):1558–1566. https://doi.org/10.1177/0363546517691517
Brown C. Anatomic ACL reconstruction. Sport Medical Journal ASPETAR. https://www.aspetar.com/journal/upload/PDF/201418125811.pdf
Hamido F et al (2020) Anterolateral ligament reconstruction improves the clinical and functional outcomes of anterior cruciate ligament reconstruction in athletes. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06119-w
Sonnery-Cottet et al (2020) Combined ACL and anterolateral reconstruction is not associated with a higher risk of adverse outcomes. Orthopaedic J Sports Med 8(5):2325967120918490. https://doi.org/10.1177/2325967120918490
Helito CP et al (2019) Combined reconstruction of the anterolateral ligament in patients with ACL injury and ligamentous hyperlaxity leads to better clinical stability and a lower failure rate than isolated ACL reconstruction. J Arthroscopic Related Surg. https://doi.org/10.1016/j.arthro.2019.03.059
Helito CP et al (2018) Combined reconstruction of the anterolateral ligament in chronic ACL injuries leads to better clinical outcomes than isolated ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-4934-2
Nitri M (2016) An in vitro robotic assessment of the anterolateral ligament: part 2, anterolateral ligament reconstruction combined with anterior cruciate ligament reconstruction. Am J Sports Med 44(3):593–601. https://doi.org/10.1177/0363546515620183
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097pmid:19621072
Tulloch S, Getgood A (2019) Consideration of lateral augmentation in anatomic anterior cruciate ligament reconstruction. Ann Joint. https://doi.org/10.21037/aoj.2019.02.01
Fu et al (2020) Is all inside with suspensory cortical button fixation a superior technique for anterior cruciate ligament reconstruction surgery? BMC Musculoskeletal Disorders, A systematic review and meta-analysis Fu et al. https://doi.org/10.1186/s12891-020-03471-3
Kelly et al (2021) Biomechanical effects of combined anterior cruciate ligament reconstruction and anterolateral ligament reconstruction: a systematic review and meta-analysis. Orthopaedic J Sports Med 9(6):23259671211009880. https://doi.org/10.1177/23259671211009879
Ferretti A et al (2016) Combined intra-articular and extra-articular reconstruction in anterior cruciate ligament deficient knee: 25 years later. Arthroscopy J Arthroscopic Related Surg. https://doi.org/10.1016/j.arthro.2016.02.006
Rosenstiel N et al (2018) Combined Anterior Cruciate and Anterolateral Ligament Reconstruction in the Professional Athlete: Clinical Outcomes From the Scientific Anterior Cruciate Ligament Network International Study Group in a Series of 70 Patients With a Minimum Follow-Up of 2 Years. Arthroscopy J Arthroscopic Related Surg. https://doi.org/10.1016/j.arthro.2018.09.020
Gurpinar T (2019). Decision-Making for ALL Reconstruction and Surgical Techniques. https://doi.org/10.5772/intechopen.86398
Delaloye JR et al (2017) Clinical outcomes after combined anterior cruciate ligament and anterolateral ligament reconstruction. Techniques Orthopaedics 33(4):225–231. https://doi.org/10.1097/bto.00326
Delaloye JR et al (2018) Combined anterior cruciate ligament and anterolateral ligament lesions: from anatomy to clinical results. Ann Joint 3:82. https://doi.org/10.21037/aoj.2018.09.08
Daggett M et al (2021) Clinical results of combined ACL and anterolateral ligament reconstruction: a narrative review from the SANTI Study Group. J Knee Surg 34(09):962–970. https://doi.org/10.1055/s-0040-1701220
Cheng et al (2020) Surgical intra- and extra-articular anterior cruciate ligament reconstruction: a meta-analysis. BMC Musculoskelet Disord 21:414. https://doi.org/10.1186/s12891-020-03438-4
Jankovic et al (2021) Modified technique for combined reconstruction of anterior cruciate ligament and anterolateral ligament. Arthrosc Tech. https://doi.org/10.1016/j.eats.2020.10.046
Gomes JLE et al (2017) Intra-articular Anterior Cruciate Ligament Reconstruction with Extra-articular Lateral Tenodesis of the Iliotibial Band. Arthrosc Tech. https://doi.org/10.1016/j.eats.2017.05.032
Acknowledgements
We thank the staff of Klinik Bahasa for their help during manuscript preparation.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they do not have any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rhatomy, S., Ariyanto, M.W., Fiolin, J. et al. Comparison of clinical outcomes between isolated ACL reconstruction and combined ACL with anterolateral ligament reconstruction: a systematic review and meta-analysis. Eur J Orthop Surg Traumatol 33, 685–694 (2023). https://doi.org/10.1007/s00590-021-03194-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-021-03194-8