Abstract
Purpose
The aim of this study was to compare knee awareness, based on the FJS-12 score, among three patient groups: Anterior cruciate ligament reconstruction (ACLR), ACLR + meniscus repair and ACLR + partial meniscectomy. The relationship between FJS-12 scores and scores on other instruments (Lysholm Knee Scoring Scale, Tegner Activity Level Scale, KOOS and WOMAC) was also evaluated.
Methods
Forty-three patients were divided into group A (isolated ACLR) group B (ACLR + meniscectomy) and group C (ACLR + meniscus repair). Graft thickness, femoral tunnel width, tibial tunnel width, tibial screw thickness and follow-up time were evaluated in all three groups. The subjective knee scores (KOOS, WOMAC, Lysholm Knee Scoring Scale, Tegner Activity Level Scale and FJS-12) of the groups were then compared.
Results
FJS-12 scores of 43 patients were evaluated. The mean age was 26.1 ± 6.5 years (range: 18–40 years). Group A: 23; group B: 9 and group C include 11 patients. The mean FJS-12 score of group B (median: 100 [range: 98–100]) was higher than that the others. Spearman’s rho test showed that the FJS-12 is highly compatible with the other scores.
Conclusion
According to this study, FJS-12 and the other scoring systems showed that ACLR with partial meniscectomy is the most effective surgical method to restore normal sensation in the knee.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Different scoring systems are used in the subjective evaluation of pain after knee surgery, including the Lysholm Knee Scoring Scale, the Tegner Activity Level Scale, the Knee Injury and Osteoarthritis Outcome (KOOS), and the Western Ontario and McMaster Universities Arthritis Index (WOMAC) [1,2,3]. The reliability and validity of these scoring systems are well-established. A new patient-reported outcome measure, the Forgotten Joint Score-12 (FJS-12), was created in 2012 [4], and its validity and reliability in Turkish patients have been demonstrated. The FJS-12 consists of 12 questions regarding joint awareness during the night, daily activities and sports participation [5,6,7,8,9]. Function is indexed by a total score of 0–100 [6]. Higher scores are indicative of better adaptation to reconstruction (i.e., better outcomes) [4, 5, 18].
Several studies have used the FJS-12 to evaluate tolerance of artificial joints, especially in patients who underwent hip and knee arthroplasty [4, 10,11,12,13,14,15,16,17]. However, the FJS-12 has rarely been used in patients undergoing anterior cruciate ligament reconstruction (ACLR) [5, 18]. The aim of this study was to compare knee awareness, based on the FJS-12 score, among three patient groups distinguished according to the treatment method: ACLR, ACLR + meniscus repair and ACLR + partial meniscectomy. We also evaluated the relationship between FJS-12 scores and scores on other instruments (Lysholm Knee Scoring Scale, Tegner Activity Level Scale, KOOS and WOMAC).
Materials and methods
Patient selection
In this retrospective study, the hospital records of 65 patients who underwent ACLR between January 2016 and May 2017 were reviewed. Adult patients operated by the same surgeon using the same surgical technique with at least 1 year of follow-up, who participated in subjective knee evaluations during outpatient follow-up and with pathology limited to one knee were included in the study. Patients with accompanying lesions other than meniscus and anterior cruciate ligament injury (osteochondral lesion, multiple ligament lesion), revision surgery, bone patellar tendon bone ACL reconstruction, inside-out and outside-in meniscus repair and were in the pediatric age group were excluded.
The 43 patients who met the inclusion criteria were divided into group A (isolated ACLR), group B (ACLR + meniscectomy) and group C (ACLR + meniscus repair). Graft thickness, femoral tunnel width, tibial tunnel width, tibial screw thickness and follow-up time were evaluated in all three groups. The subjective knee scores of the groups were then compared.
Approval for the study was obtained from the Local Ethics committee of the hospital where the study was conducted (number 2019/16–10).
Surgical technique
Arthroscopic anatomic ACLR with hamstring autograft is performed in our center. After the hamstring autograft is obtained, the knee is flexed to 110° and the femoral tunnel is opened in accordance with the graft thickness using a low anteromedial portal. The femoral side is then secured using a button system (ToggleLoc With Ziploop; Biomet, Warsaw, IN, USA), and the tibial side using a bioabsorbable screw (Gentle Threads; Biomet,) and ligament staple (Zimmer Biomet).
In the clinic where the study is performed, partial meniscectomy is applied in obesity, chronic degenerative tear, complex tear, and white-white zone tears. Apart from this, repair is applied to the meniscus tears. The rupture patterns in patients with meniscus tear, as determined by diagnostic arthroscopy, are evaluated and partial meniscectomy or all-inside repair (Fast-Fix 360; Smith & Nephew, Fort Worth, TX, USA) is then performed as appropriate. Intraarticular drains are placed in all patients at the end of the surgery. All patients also receive an angle-adjusted hinged knee brace during the postoperative period. On the second postoperative day, 90° flexion is allowed after the drains are removed, followed by 120˚ flexion in week 2, at which time active quadriceps and hamstring strengthening exercises are started. Jogging is allowed in month 2 and a return to recreational sports in month 6.
In patients undergoing meniscus repair, weight-bearing is not allowed for the first 1.5 months. All patients are followed at the outpatient clinic for at least 1 year after surgery. For posterior and midline meniscus tears, all-inside meniscus repair is performed, while for anterior tears outside-in meniscus repair is applied. In our study, all patients underwent all-inside meniscus repair, performed by the same surgeon using the same technique.
Scoring
Patient sex, age and clinical data, as well as follow-up time, were obtained from hospital records. The thickness of the graft used in the reconstruction, the diameters of the femoral and tibial tunnels and the diameter and length of the screw used for tibial side fixation were noted. The KOOS, WOMAC, Lysholm Knee Scoring Scale, Tegner Activity Level Scale and FJS-12 were administered to all patients during the first year of follow-up, and the scores were recorded in the outpatient files. These records were examined retrospectively for this study.
Statistical analysis
Statistical analyses were performed using SPSS 25.0 (IBM Corp., Armonk, NY, USA). The normality of the data was tested using a Shapiro–Wilk test; homogeneity of variance was evaluated using Levene’s test. The Kruskal–Wallis H test was applied according to the results of the Monte Carlo simulation; the post hoc analysis was performed using Dunn’s test. Spearman’s rho tests were used to examine correlations between variables. Categorical variables were compared using the Fisher–Freeman–Halton test and Monte Carlo simulation. Quantitative data are expressed as the mean ± standard deviation (SD) or as the median (range); categorical data are expressed as n (%). The variables were examined at the 95% confidence level, and a p value < 0.05 was considered to indicate statistical significance.
Results
This study examined the FJS-12 scores of 43 patients (25 right knee, 18 left knee). The mean age of the patients was 26.1 ± 6.5 years (range: 18–40 years). All patients were found to have non-contact rotational knee trauma while doing sports. Twenty-three patients underwent isolated ACLR (group A), nine underwent ACLR with partial meniscectomy (group B), and eleven underwent ACLR with meniscus repair (group C). No root rupture or ramp lesion was detected in patients included in the study. It was determined that the ruptures that were repaired are non-complex vertical and radial ruptures. The data of the three patient groups are shown in Table 1.
The mean thickness of the graft was 8.07 ± 0.97 mm (range: 7–10 mm), the mean femoral tunnel width was 8 ± 1.06 mm (range: 6–10 mm), and the mean tibial tunnel width was 8 ± 1.06 mm (range: 6–10). The mean tibial screw thickness was 9.05 ± 0.75 mm (range: 7–10 mm). The mean follow-up period was 30.65 ± 25.23 months (range: 12–126 months). Data related to the surgical technique did not differ significantly among the three groups.
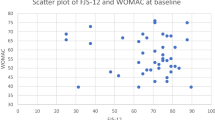
The mean (range) scores on the various scoring systems used in this study are shown in Table 2. The mean FJS-12 score of group B (median: 100 [range: 98–100]) was higher than that of group A or C. The latter group had the lowest FJS-12 score (median: 94 [range: 87–100]) (p = 0.008) (Fig. 1). The correlation between the FJS-12 score and the other scores was evaluated using Spearman’s rho test (Table 3), which showed that the FJS-12 is highly compatible with the other scores.
Discussion
Behrend et al. (2012) devised the FJS-12 to evaluate the extent to which a repaired joint could be “forgotten” and became “normal” after knee surgery. A recent study determined the correlation of the FJS-12 with other scores and concluded that the FJS-12 is a “promising” scoring system [4].
The FJS-12 was initially developed for evaluating the recovery of the treated knee of arthroplasty patients. In addition to the study of Behrend et al. (2012), Thienpont et al. (2014) compared different knee replacement options and found that patients with patellofemoral resurfacing had lower FJS-12 scores than those who underwent medial unicompartmental knee arthroplasty or total knee arthroplasty (TKA) [4, 11]. Hamilton et al. (2016) showed that the FJS-12 was more sensitive and less vulnerable to ceiling effects than the Oxford Hip Score [10]. Other studies have used the FJS-12 to compare the results of different surgical techniques [13,14,15,16,17]. Most recently, Fichler et al. evaluated 100 total TKAs and concluded that the FJS-12 has several advantages over other subjective scoring systems [19].
For arthroplasty, the surface material used in the repair differs from the native tissue, similar to the graft used in ACLR. Consequently, the sense of “normality” of the knee may change after surgery. Two previous studies used the FJS-12 to evaluate ACLR outcomes. In 2016, Behrend et al. [5] showed that the FJS-12 scores of patients undergoing ACLR were lower than those of the unoperated population with healthy knees. In 2017, Behrend et al. compared medium- and long-term FJS-12 scores to those of other scoring systems. They found a lower ceiling effect for the FJS-12 compared to the WOMAC and KOOS and concluded that the FJS-12 is a valuable scoring system not only for TKA patients, but also for young, active patients undergoing other knee surgeries [18]. In this study, we obtained the FJS-12 scores of patients who underwent ACLR and examined the compatibility of this scoring system with the Lysholm Knee Scoring Scale, Tegner Activity Level Scale, KOOS and WOMAC. We found strong correlations between the FJS-12 scores and those of the other scoring systems, thus supporting the results of Behrend et al. [18] by showing that: (i) the FJS-12 can be used in young, active patients undergoing ACL surgery, and (ii) the FJS-12 is compatible with other scoring systems but can also be used alone.
Hevesi et al. (2019) pointed out the necessity of meniscus repair, due to its ability to enhance joint contact and protect against osteoarthritis. In a study by Cinque et al. (2019), the Tegner, Lysholm and WOMAC scores after meniscus repair in a white-white region were lower than those after repairs in red-red and red-white regions [20, 21]. Svantesson et al. (2018) evaluated the data of 6,398 patients and concluded that those who underwent combined ACLR and medial meniscus repair showed the least improvement in symptoms, while those who underwent medial and lateral meniscus resection showed the greatest improvement [22]. In a recent study, significant differences in outcomes between ACLR + meniscus repair and ACLR + partial meniscectomy groups were determined based on scoring systems other than the FJS-12. However, our study showed that a difference is also apparent when using the FJS-12. There are many studies support that arthrosis develops when patients who undergo meniscectomy. This difference in favor of the meniscectomy group in our study is only related to the early postoperative joint sensation. The scoring should not be expected to evaluate arthrosis at the end of the first year.
It is not one of the aims of this study to reveal the relationship between smoking and meniscus repair and FJS-12 score. However, it is thought that knowing the status of smoking may be valuable in terms of providing preliminary information for randomized studies in which standard patient groups are evaluated in large series of this group of patients in the future.
A limitation of our retrospective study was that all of the patients were male, as no data were available for female patients. This likely reflects the socioeconomic structure of Turkey, and specifically the geographic region in which our center is located, where women's participation in sports is limited by cultural constraints, as described previously [23]. A further limitation was the small sample size. Nonetheless, even though the patients were divided into three groups according to the surgical method, statistically significant differences were demonstrated.
Conclusion
In this study, the results of the FJS-12 were highly consistent with those of the Lysholm Knee Scoring Scale, Tegner Activity Level Scale, COOS and WOMAC scores, in the context of postoperative evaluation of ACLR outcomes. Based on the scores on the FJS-12 and the other scoring systems, ACLR with partial meniscectomy is the most effective surgical method to restore normal sensation in the knee. Prospective studies with larger series and longer follow-up periods would provide more comprehensive results and should be performed to confirm the validity of the FJS-12 for evaluating ACLR procedures.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article or its supplementary materials.
Code availability
The authors confirm that the code of this study are available within the article or its supplementary materials.
References
Rothrauff BB, Jorge A, de Sa D, Kay J, Fu FH, Musahl V (2019) Anatomic ACL reconstruction reduces risk of post-traumatic osteoarthritis: a systematic review with minimum 10-year follow-up. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05665-2
Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD (1988) Knee injury and osteoarthritis outcome score (KOOS)–development of a self-administered outcome measure. J Orthop Sports Phys Ther 28(2):88–96. https://doi.org/10.2519/jospt.1998.28.2.88
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Behrend H, Giesinger K, Giesinger JM, Kuster MS (2012) The “forgotten joint” as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. J Arthroplasty 27:430–436. https://doi.org/10.1016/j.arth.2011.06.035
Behrend H, Zdravkovic V, Giesinger JM, Giesinger K (2017) Joint awareness after ACL reconstruction: patient-reported outcomes measured with the forgotten joint score-12. Knee Surg Sports Traumatol Arthrosc 25(5):1454–1460. https://doi.org/10.1007/s00167-016-4357-x
Kınıklı GI, Deniz HG, Karahan S, Yuksel E, Kalkan S, Donder Kara D, Onal S, Sevinc C, Caglar O, Atilla B, Yuksel İ (2017) Validity and reliability of Turkish version of the forgotten joint score-12. J Exerc Ther Rehabilit 4(1):18–25
Tuzun EH, Eker L, Aytar A, Daskapan A, Bayramoglu M (2005) Acceptability, reliability, validity and responsiveness of the Turkish version of WOMAC osteoarthritis index. Osteoarthritis Cartilage 13(1):28–33. https://doi.org/10.1016/j.joca.2004.10.010
Paker N, Buğdaycı D, Sabırlı F, Özel S, Ersoy S (2007) Knee injury and osteoarthritis outcome score: reliability and validation of the Turkish version. Turkiye Klinikleri J Med Sci 27:350–435
Celik D, Coskunsu D, Kilicoglu O (2013) Translation and cultural adaptation of the Turkish Lysholm knee scale: ease of use, validity, and reliability. Clin Orthop Relat Res 471(8):2602–2610. https://doi.org/10.1007/s11999-013-3046-z (Epub 2013 May 11)
Hamilton DF, Giesinger JM, MacDonald DJ, Simpson AH, Howie CR, Giesinger K (2016) Responsiveness and ceiling effects of the forgotten joint score-12 following total hip arthroplasty. Bone Joint Res 5(3):87–91. https://doi.org/10.1302/2046-758.53.2000480
Thienpont E, Opsomer G, Koninckx A, Houssiau F (2014) Joint awareness in different types of knee arthroplasty evaluated with the forgotten joint score. J Arthroplasty 29(1):48–51. https://doi.org/10.1016/j.arth.2013.04.024
Thomsen MG, Latifi R, Kallemose T, Barfod KW, Husted H, Troelsen A (2016) Good validity and reliability of the forgotten joint score in evaluating the outcome of total knee arthroplasty. Acta Orthop 87(3):280–285. https://doi.org/10.3109/17453674.2016.1156934
Bell SW, Stoddard J, Bennett C, London NJ (2014) Accuracy and early outcomes in medial unicompartmental knee arthroplasty performed using patient specific instrumentation. Knee 21(Suppl 1):S33–S36. https://doi.org/10.1016/S0968-0160(14)50007-5
Matsumoto M, Baba T, Homma Y, Kobayashi H, Ochi H, Yuasa T, Behrend H, Kaneko K (2015) Validation study of the forgotten joint score-12 as a universal patient-reported outcome measure. Eur J Orthop Surg Traumatol 25:1141–1145. https://doi.org/10.1007/s00590-015-1660-
Thienpont E, Vanden Berghe A, Schwab PE, Forthomme JP, Cornu O (2016) Joint awareness in osteoarthritis of the hip and knee evaluated with the ‘Forgotten Joint’ Score before and after joint replacement. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-00015-03970-00164
Thienpont E, Zorman D (2015) Higher forgotten joint score for fixed-bearing than for mobile-bearing total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-00015-03663-z
Zuiderbaan HA, van der List JP, Khamaisy S, Nawabi DH, Thein R, Ishmael C, Paul S, Pearle AD (2015) Unicompartmental knee arthroplasty versus total knee arthroplasty: Which type of artificial joint do patients forget? Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-00015-03868-00161
Behrend H, Giesinger K, Zdravkovic V, Giesinger JM (2017) Validating the forgotten joint score-12 in patients after ACL reconstruction. Knee 24(4):768–774. https://doi.org/10.1016/j.knee.2017.05.007
Eichler D, Beaulieu Y, Barry J, Massé V, Vendittoli PA (2020) Perception of a natural joint after total knee arthroplasty. J Arthroplasty 35(2):358–363
Hevesi M, Krych AJ, Kurzweil PR (2019) Meniscus tear management: indications, technique, and outcomes arthroscopy. J Arthrosc Relat Surg 35(9):2542–2544
Cinque ME, DePhillipo NN, Moatshe G, Chahla J, Kennedy MI, Dornan GJ, LaPrade RF (2019) Clinical outcomes of inside-out meniscal repair according to anatomic zone of the meniscal tear. Orthop J Sports Med 25(7):2325967119860806
Svantesson E, Cristiani R, Hamrin Senorski E, Forssblad M, Samuelsson K, Stålman A (2018) Meniscal repair results in inferior short-term outcomes compared with meniscal resection: a cohort study of 6398 patients with primary anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 26(8):2251–2258. https://doi.org/10.1007/s00167-017-4793-2 (Epub 2017 Nov 13)
Inal HS (2011) Women’s and Girls’ Sports in Turkey. WSPAJ. https://doi.org/10.1123/wspaj.20.2.76
Acknowledgments
The authors would like to thank biostatistician Huseyin Candan for cleaning the data and performing the statistical analysis. The English in this document has been checked by at least two professional editors, both native speakers of English. For a certificate, please see: http://www.textcheck.com/certificate/5Lkmhc.
Funding
This study has no funding.
Author information
Authors and Affiliations
Contributions
IEK contributed to protocol development, data analysis, manuscript writing/editing, data collection or management. MCG contributed to data collection or management, data analysis, manuscript editing. CDB contributed to data analysis, manuscript editing. VZ contributed to data analysis, manuscript editing. OE contributed to protocol development, data analysis, manuscript writing/editing. All authors confirm that the manuscript has been read and approved by all named authors and there are no other people who meet the criteria for authorship that are no listed. We further confirm that the order of authors listed in the manuscript has been approved by all of us.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethics approval
Approval for the study was obtained from the Local Ethics committee of the hospital where the study was conducted (number 2019/16–10).
Consent to participate
Consent to participate approval was obtained from all participants who participated in the study.
Consent for publication
Consent for publication approval was obtained from all participants who participated in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kacmaz, I.E., Gezer, M.C., Basa, C.D. et al. Use of the forgotten joint score (FJS)-12 to evaluate knee awareness after isolated anterior cruciate ligament reconstruction with and without meniscus repair or partial meniscectomy. Eur J Orthop Surg Traumatol 32, 413–418 (2022). https://doi.org/10.1007/s00590-021-02991-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-021-02991-5