Abstract
Background/Purpose
Forgotten Joint Score (FJS) is designed to asses patient recovery post Total Knee Arthroplasty (TKA) in a new dimension. It assess the ability to forget the operated joint as artificial during activities of daily living. New Knee Society Score (NKSS) is developed to encompass objective and subjective outcome as well as an assessment of patient expectation and satisfaction. Our purpose was (1) to determine FJS at 1 year post TKA in Indian Patients, and (2) to assess convergent validity between FJS and the NKSS. We hypothesised that FJS should strongly correlate with the Satisfaction (SS) and Knee perception(KPS) sub-component of NKSS
Methods
We enrolled 181 patients who underwent primary TKA during an 8-month duration. They were prospectively followed up at 1-year review clinic when FJS and NKSS were administered. 169 patients completed the assessment forms and 13 patients were lost to follow-up. Statistical evaluation was done with Spearman correlation test.
Results
Mean FJS at 1 year was 66.6 ± 25.9 with 14% ceiling and 1% floor effects. There was a mild to moderate correlation of FJS with NKSS (p < 0.001, r = 0.47) and its sub-scores (p < 0.001; r = 0.43 and r = 0.44). There was a weak correlation of FJS with NKSS sub-components of SS and KPS (p < 0.001; r = 0.37 and 0.25, respectively).
Conclusion
Mean FJS at 1 year post TKA showed convergent validity with NKSS; however, the correlation was not strong enough to use them interchangeably. Hypothesis that FJS should strongly correlate with the NKSS sub-components of satisfaction and joint perception was refuted. We conclude, FJS provides unique evaluation in recovery post TKA, different from NKSS.
Level of Evidence
Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the years, several outcome measures have been developed to evaluate results of Total Knee Arthroplasty (TKA). The challenges are to include both the patient’s subjective assessment of the implanted joint’s function and the objective assessment done by the clinician, while limiting the respondent burden. There remains a small percentage of patients who record good scores on some well-established scores and yet remain dissatisfied after surgery. The search for an ideal outcome measure has thus continued. There has been an increasing amount of interest in Forgotten Joint Score (FJS), a patient reported outcome measure (PROM) which uses a novel dimension of “forgetting the joint” in activities of daily living as a benchmark to evaluate the outcome of the implanted joint. A status of “forgotten joint” would integrate a variety of variables like pain, stiffness, function in activities of daily living, patient expectations, and psycho-social factors [1]. FJS is reported to provide useful information supplementing other scores [2,3,4]. In our practice, we use the New Knee Society Score (NKSS) developed from its predecessor the Knee Society Score as our routine outcome measure for arthroplasty patients. NKSS is designed to combine the surgeon assessed objective outcome (OKS), patients’ evaluation of subjective recovery as well as assessment of their expectation and satisfaction (SKS) [5, 6]. We decided to study the FJS in our patients and compare it to the NKSS.
Our Primary aim was to determine FJS values for Indian patients at 1 year post TKA along with its floor and ceiling effects. Our secondary aim was to determine the convergent validity of FJS with NKSS and its subcomponents. We aimed to see if FJS and NKSS could be used interchangeably. Further, we hypothesised that ‘forgetting the joint’ concept correlates to a more ‘normal’ perception of the implanted joint, and should translate into better satisfaction post TKA. As per our hypothesis, we expected a strong correlation between FJS and sub-components of NKSS namely—Satisfaction (SS) and Knee Perception(KPS) which we have elaborated in ‘Methods’ section. To our knowledge, there is no study in literature that has correlated the two PROMS of FJS and NKSS in this manner.
Materials and Methods
This study was undertaken at Lilavati Hospital & Research Centre, Mumbai from 1st June, 2016. We enrolled all patients who had undergone primary TKA by the same operating surgeon (RNM), between 1st June 2016 and 28 February 2017. These patients had a uniform procedure using Computer Assisted System (Kolibri navigation system, Brainlab, Munich, Germany) and one of the two knee implants (PFC Sigma or Attune implant, DePuy Orthopaedics Inc, Warsaw, IN, USA). Their post-operative protocol and rehabilitation were also uniform. The enrolled patients were called to attend 1 year review clinic where FJS and NKSS were administered apart from clinical and radiographic examination by the Joint Replacement Fellow (AD). Study was approved by our IRB. During the specified period, 181 patients (222 knees) including 41 patients who had single stage sequential bilateral arthroplasties presented with primary TKA. Of these 181 patients, 151 patients (186 knees) attended the review clinic within the specified time of 12–14 months post primary procedure, while 17 patients (21 knees) completed the forms with the help of their physiotherapist and sent them via email. There were 13 patients (15 knees) who could do neither and were considered lost to follow-up. Thus, we had 168 patients (207 knees) for whom complete data were available for analysis (Fig. 1 Flowchart). Of 168 patients, 37 were males and 131 were females, with mean age of 66.9 years (37–85), and mean BMI of 30.2 (19–49).
At the review clinic, patients underwent clinical and radiographical examination, and were administered FJS and NKSS.
FJS consists of a self-administered questionnaire on 12 activities asking patients to report on how aware they are of their artificial joint in everyday life [1]. For each of the 12 activities, they are made to select from 5 answers, which represent the level of awareness—from never aware (0 points) to mostly aware (4 points). Thus, each response is given a score (from 0 to 4). The sum of all responses divided by the number of completed items gives a mean value which is multiplied by 25 to obtain a score range of 0–100. Finally, the obtained score is subtracted from 100, to change the direction of the final score so that a higher score represents a higher level of forgetting or a low degree of awareness of the artificial joint. Also, if more than 4 out of 12 responses are missing, then that score is not used, as per the developer’s recommendation.
NKSS is the summation of the Objective knee Score (OKS) of 100 points and Subjective knee score (SKS) of 155 points, giving a maximum total score of 255 points. The SKS (155 points) is calculated from a self-administered questionnaire and consists of two sub-scores, Function Score (FS, 100 points) and Expectation and Satisfaction Score (ESS, 55 points). OKS (100 points) is obtained from a combination of clinical examination and a self-administered questionnaire which includes a question regarding the patients’ perception of his implanted knee i.e. “Does this knee feel ‘normal’ to you?” The patient has to select one of three responses i.e. ‘Always’, ‘Sometimes’ or “Never” with respective scores of 5, 3, and 0. We have labelled this as the Knee Perception sub-component (KPS) for the purpose of this study. Its lowest value is 0 and maximum value is 5, higher score representing more natural joint perception.
Bilateral patients were scored twice, thus each knee had its own FJS and NKSS.
We used the SPSS software V15.0 (Statistical Package for Social Sciences Version 15.0) for the statistical analysis. Evaluation was done to determine, for both FJS and NKSS, mean with standard deviation (SD), median with IQR, range. Also for each score, ceiling and floor effects (number of patients achieving maximum or minimum possible scores, respectively) were calculated. Shapiro–Wilk tests were applied to test whether distribution of FJS & NKSS were normal or not normal. Shapiro–Wilk test values for FJS were test statistic = 0.94, S, P < 0.001 and for NKSS test statistic = 0.98, S, P = 0.003, concluding that the distribution were not normal. Therefore, Spearman Correlation test was run to assess the convergent validity of FJS with NKSS and sub-scores as well as for correlating the post-operative range of flexion achieved at 1 year. If the correlation was found to be significant (p < 0.05), the strength of correlation was determined by the Spearman’s correlation co-efficient “r”. r < 0.2 indicated clinically irrelevant correlation, r = 0.2–0.4 indicated weak correlation, r = 0.4–0.6 indicated moderately strong correlation and r > 0.6 indicated strong correlation [7].
Results
FJS at 1 year: the median value for FJS was 68.8 (IQR 40.9, mean 66.6, SD 25.9, range 0–100). The raw statistics of 207 patients are tabulated in (Table 1). FJS exhibited a 14% ceiling effect and 1% floor effect.
NKSS at 1 year: the median value for NKSS was 194 (IQR 171, mean 191.7, SD 27.1, range 125–242). The raw statistics of 207 patients are tabulated in (Table 1). No ceiling effect or floor effect was seen with NKSS (Table 1).
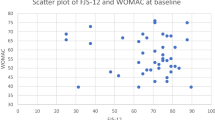
There was a positive correlation of FJS with NKSS and its sub-scores, and the correlation was moderately strong (p < 0.001; 0.37 < r < 0.47) (Table 2). There was a positive correlation of FJS with NKSS sub-components of SS and KPS but the correlation was weak (r = 0.37 and 0.25, respectively).
Discussion
FJS is generating increasing interest as a useful score and we undertook this study to identify its value in Indian patients at 1 year post TKA and compare it with one reported from other population. Additionally, we hypothesised that FJS should strongly correlate with the NKSS sub-components of satisfaction and joint perception. We did find this correlation to be positive but it was weak. Thus, this hypothesis was refuted. We also wanted to see if FJS and NKSS could be used interchangeably which could address the issue of increased respondent burden with NKSS. Our study results showed just moderate correlation between the two scores, i.e. they could not be interchanged for each other. This suggests that FJS possibly captures information which is unique and different than NKSS in the assessment of patient’s outcome post TKA.
We found the mean value of FJS at 1 year to be 66.6 (SD 25.9) which was comparable to the range from 44.8 to 88.5 reported in literature from rest of the world [8,9,10,11,12,13,14,15,16]. Beherend et al. have reported post TKA FJS of 56.3 (SD 30.5), but the exact post-operative duration at which the assessment was done was not reported [1]. Interestingly, they also studied a healthy control population with no knee/hip arthritis and reported a mean knee FJS of 71.7. Similarly, Geisinger et al. established normative values for the mean FJS as 66.8 in the United States’ general population [17]. Thus our Score of 66.6 at 1 year compares well with the score from rest of the world post TKA as well as what has been reported in the normal population.
A strong Ceiling effect impairs a scales sensitivity to change over time and ability to discriminate well between different well performing groups. We found a ceiling effect of 14% with FJS, while NKSS showed a 0% ceiling effect. We have reported 0% ceiling effect with NKSS in our earlier study also [18]. This indicates that the NKSS outperforms FJS in terms of discriminatory power. We found a low floor effect of 1% with FJS, and 0% with NKSS.
FJS is a unique score assessing satisfaction post surgery as a measure of the ability of the patient to consider the joint as normal, i.e., if you consider the joint as normal you tend to be more satisfied. Our hypothesis that forgetting the joint in activities of daily living which is captured by FJS should co-relate with natural perception of the joint captured by KPS and SS of NKSS. However, our study results showed that this was not the case. Our purpose was that if they co-relate strongly we would may be do away with FJS and get the same information with NKSS. This would help reduce the respondent burden on patient [18]. There are no other studies in literature that has looked at this comparison. Further FJS did show significant correlation with NKSS and its other sub-scores; however, the correlation was only moderate. This would suggest that the FJS and NKSS show parallel movement but may not be interchangeable with each other. FJS possibly captures information which is unique and different than NKSS in assessment of patient’s outcome post TKA.
The limitation of our study is that we cannot comment on whether our findings can be generalised to varied populations. A large, multicentric study would be needed to confirm our findings.
In conclusion, FJS at 1 year post TKA in Indian patients had a mean value of 66.6, with 14% ceiling effect and 1% floor effect. This is comparable to data from the rest of the world. FJS showed convergent validity with NKSS and its sub-scores; however, the correlation was not strong enough to suggest that scores are interchangeable. Our hypothesis that FJS should strongly correlate with the NKSS sub-components of satisfaction and joint perception was refuted. We conclude that FJS provides a unique aspect to evaluation of recovery post TKA which is different to NKSS.
References
Behrend, H., Giesinger, K., Giesinger, J. M., & Kuster, M. S. (2012). The “forgotten joint” as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. Journal of Arthroplasty, 27(3), 430–436.
Adriani, M., Malahias, M. A., Gu, A., Kahlenberg, C. A., Ast, M. P., & Sculco, P. K. (2020). Determining the validity, reliability, and utility of the forgotten joint score: a systematic review. Journal of Arthroplasty, 35(4), 1137–1144.
Robinson, P. G., Rankin, C. S., Lavery, J., Anthony, I., Blyth, M., & Jones, B. (2018). The validity and reliability of the modified forgotten joint score. Journal of Orthopaedics, 15(2), 480–485.
Wang, Z., Deng, W., Shao, H., Zhou, Y., & Li, H. (2020). Forgotten joint score thresholds for forgotten joint status and patient satisfaction after unicompartmental knee arthroplasty in chinese patients. Journal of Arthroplasty, 35(10), 2825–2829.
Noble, P. C., Scuderi, G. R., Brekke, A. C., Sikorskii, A., Benjamin, J. B., Lonner, J. H., Chadha, P., Daylamani, D. A., Scott, W. N., & Bourne, R. B. (2012). Development of a new Knee Society scoring system. Clinical Orthopaedics and Related Research, 470(1), 20–32.
Scuderi, G. R., Bourne, R. B., Noble, P. C., Benjamin, J. B., Lonner, J. H., & Scott, W. N. (2011). The new Knee Society Knee Scoring system. Clinical Orthopaedics and Related Research, 470(1), 3–19.
Swinscow, T. D., & Campbell, M. J. (2002). Statistics at square one (10th ed.). London: BMJ Books.
Behrend, H., Zdravkovic, V., Bösch, M., & Hochreiter, B. (2019). No difference in joint awareness after TKA: a matched-pair analysis of a classic implant and its evolutional design. Knee Surgery, Sports Traumatology, Arthroscopy, 27(7), 2124–2129.
Blevins, J. L., Carroll, K. M., Burger, J. A., Pearle, A. D., Bostrom, M. P., Haas, S. B., Sculco, T. P., Jerabek, S. A., & Mayman, D. J. (2020). Postoperative outcomes of total knee arthroplasty compared to unicompartmental knee arthroplasty: a matched comparison. The Knee, 27(2), 565–571.
Boyle, K. K., Nodzo, S. R., Ferraro, J. T., Augenblick, D. J., Pavlesen, S., & Phillips, M. J. (2018). Uncemented vs cemented cruciate retaining total knee arthroplasty in patients with body mass index greater than 30. Journal of Arthroplasty, 33(4), 1082–1088.
Carlson, V. R., Post, Z. D., Orozco, F. R., Davis, D. M., Lutz, R. W., & Ong, A. C. (2018). When does the knee feel normal again: a cross-sectional study assessing the forgotten joint score in patients after total knee arthroplasty. Journal of Arthroplasty, 33(3), 700–703.
French, S. R., Munir, S., & Brighton, R. (2020). A single surgeon series comparing the outcomes of a cruciate retaining and medially stabilized total knee arthroplasty using kinematic alignment principles. Journal of Arthroplasty, 35(2), 422–428.
Jones, C. W., Jacobs, H., Shumborski, S., Talbot, S., Redgment, A., Brighton, R., & Walter, W. L. (2020). Sagittal stability and implant design affect patient reported outcomes after total knee arthroplasty. Journal of Arthroplasty, 35(3), 747–751.
Nedopil, A. J., Howell, S. M., & Hull, M. L. (2020). Deviations in femoral joint lines using calipered kinematically aligned TKA from virtually planned joint lines are small and do not affect clinical outcomes. Knee Surgery, Sports Traumatology, Arthroscopy, 28(10), 3118–3127.
Puliero, B., Blakeney, W. G., Beaulieu, Y., & Vendittoli, P. A. (2019). Joint perception after total hip arthroplasty and the forgotten joint. Journal of Arthroplasty, 34(1), 65–70.
Samy, D. A., Wolfstadt, J. I., Vaidee, I., & Backstein, D. J. (2018). A retrospective comparison of a medial pivot and posterior-stabilized total knee arthroplasty with respect to patient-reported and radiographic outcomes. Journal of Arthroplasty, 33(5), 1379–1383.
Giesinger, J. M., Behrend, H., Hamilton, D. F., Kuster, M. S., & Giesinger, K. (2019). Normative values for the forgotten joint score-12 for the US general population. Journal of Arthroplasty, 34(4), 650–655.
Maniar, R. N., Maniar, P. R., Chanda, D., Gajbhare, D., & Chouhan, T. (2017). What is the responsiveness and respondent burden of the new knee society score? Clinical Orthopaedics and Related Research, 475(9), 2218–2227.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Each author certifies that he or she has no commercial associations that might pose a conflict of interest in connection with the submitted article. Disclosure of one of the Co-Authors outside the submitted work: (1) Depuy India—receives consultant fees. (2) Indian Society of Hip and Knee Surgeon—Trustee, Past President and Board Member.
Ethical Approval
The study has been approved by Lilavati Kirtilal Mehta Medical Trust Research Centre (Institutional Ethics Committee).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Maniar, R.N., Dhiman, A., Maniar, P.R. et al. Forgotten Joint Score Post Total Knee Arthroplasty and Its Correlation with the New Knee Society Score. JOIO 55, 1175–1179 (2021). https://doi.org/10.1007/s43465-021-00452-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-021-00452-z