Abstract
The rising incidence of mangled extremity seen in modern trauma has lead to significant patient mortality. A lot of research is going on at microcellular level for a better understanding of tissue injury, repair and regeneration. PAX-7 is one such transcription factor, a marker of satellite stem cells in skeletal muscle. Though few studies have shown concrete evidence of increased expression of PAX-7 in the nearby injured zone in skeletal muscle post-injury, none has studied its expression in an event of mangled injury of limb in humans. We, hereby, attempted to identify whether PAX-7 expression of tissue near the zone of injury, after grievous trauma like mangled injury of extremities, actually increases, decreases or remains unaffected. A pilot study was conducted on 30 cases at a level 3 trauma centre; patients were segregated into two groups—group I with MESS score ≥ 7 and group II with score < 7. For group I patients, amputation was planned, and for group II, limb salvage surgery was planned. Skeletal muscle samples from three different zones (A, B and C) in group I, while pre- and post-debridement skeletal muscle samples in group II were sent for microscopic examination and IHC staining with PAX-7 antibody. A definite increase in PAX-7 expression, post-trauma near the zone of injury (Zone B and C in group I and post-debridement in group II), was noted. Increased expression of PAX-7 signifies increased recruitment of satellite stem cells near the injury zone, thereby reflecting the activation of skeletal muscle regeneration cascade. Hence, increased staining of PAX-7 in tissues could be a viable marker for identifying potential regeneration of skeletal muscle post-injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mangled extremity is defined as a severe injury to a limb that often leaves its viability in doubt. It has also been defined as involvement of at least 3 out of 4 systems, i.e. bone, blood vessels, nerves and soft tissue [1]. In the twenty-first century, the incidence of mangled extremity has risen in proportion to the increased number of motor vehicles on roads [2, 3].
In the present scenario, with the advent of increasing skills of surgeon in handling such trauma, along with the availability of microscopic vascular and nerve repair surgeries, innovative techniques of soft tissue cover and better antibiotics, to curb the infection, it is now possible to reconstruct even those limbs which in the past used to be amputated. Nevertheless, there is still a chance of postoperative complications like infection, wound dehiscence and healing problems, non-unions, all of which could necessitate secondary amputation after prolonged morbidity [3,4,5,6,7].
A lot of research is going on at microcellular level that has increased our understanding of concepts of tissue inflammation, repair and regeneration in recent decades. Understanding genetics and gene expression is one such pathway that has thrown some light in this aspect. PAX-7 protein is one such transcription factor, which is known to be expressed in quiescent satellite stem cells in skeletal muscle. This PAX-7 protein continues to express in satellite cell as it undergoes activation and proliferation and finally get lost when these satellite cells undergo differentiation. These satellite stem cells are actually the mesenchymal cells which gets stimulated and significantly multiply in the event of muscle trauma and differentiate into new muscle cells during muscle regeneration [8,9,10,11,12]. Hence, PAX-7 can be used as a marker of satellite cells, thereby indicating the muscle regeneration potential. Some preclinical and clinical studies have also shown the role of PAX-7 as a marker of muscle regeneration, and therefore, we have assumed that PAX-7 may play a significant role in muscle regeneration in the event of trauma [13,14,15,16,17,18,19,20,21,22]. Based on the available literature and facts, we hypothesised that expression of PAX-7 should also be altered near the zone of injury in case of mangled injuries. These altered expressions of PAX-7 in such zone may give an idea about the regeneration potential of muscle tissue and about its reparative capacity and viability.
We, thus, planned a pilot study with the aim of evaluating the expression and significance of PAX-7, if any, in traumatic limb. The staining of PAX-7 antibody was graded, and the results were compared in different specified zones, and the results are presented.
Materials and methods
A pilot study was prospectively conducted on 30 patients that presented with a mangled extremity to a level I trauma centre of North India from 1 January 2016 till 31 December 2016. All patients of age ≥ 18 years who sustained an injury of either upper or lower or both extremities, with either isolated injury or polytrauma and without medical comorbidities, were included in this study.
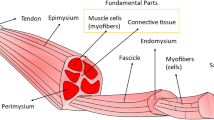
After initial resuscitation and stabilisation, all patients were segregated into two groups on the basis of MESS score. Group I patients, with MESS score ≥ 7, were taken up for primary amputation, whereas group II patients, with MESS score < 7, were planned for limb salvage. Intraoperatively skeletal muscle tissue samples were sent from three different zones in group I patients, whereas pre- and post-debridement muscle samples from the injury zone were taken in group II patients. In group I patients, three different zones were described as follows: Zone A was the zone of mangled tissue containing mostly dead and dying muscle tissues, Zone C was the zone of final amputation expected to have viable skeletal muscle fibres, while Zone B was described as intermediate zone of doubtful viability between Zone A and Zone C (Fig. 1).
The positive control group, used in the study, consists of the normal skeletal muscle tissue samples that were obtained from the resection zone of bone osteosarcoma or from autopsy patients that were available in the histopathology department of our institute. All the samples were stored in sterile containers with 10% buffered formalin solution and were examined under microscope with routine haematoxylin and eosin (H&E) staining. On H&E staining, the extent of necrosis involving individual muscle fibre or large fascicular group was noted along with degree of interspersed inflammatory cells. Viable muscle fibres were clearly delineated from degenerated muscle fibre based on early morphological changes, fragmented sarcoplasm and nucleus.
A 2-µm-thick paraffin section was made afterwards for each sample, to further carry out immunohistochemistry(IHC) staining by peroxidase and anti-peroxidase method with subsequent staining with PAX-7 antibody (Abcam company, Cambridge, UK). The antibody used in our study was mouse monoclonal antibody and was standardised with control group of muscle with dilution of 1/100.
PAX-7 gives nuclear staining where the positive staining may be located either within or at periphery of the cytoplasm of individual muscle. The positive staining was scored into four groups:
-
0.
When no positive staining is observed.
-
1.
When ≤ 3 nuclei are stained positive.
-
2.
When 4–6 nuclei are stained positive.
-
3.
When > 6 nuclei are stained positive.
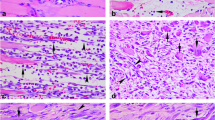
On immunohistochemistry staining, the positive staining of nuclei within or at periphery of cytoplasm was noted and graded accordingly as described above (Figs. 2a, b, 3a, b). The sample with higher grade of staining indicates higher expression of PAX7, whereas sample with no expression of PAX-7 is given a score of 0. Thus, higher PAX-7 scores imply significant activation of tissue regeneration cascade with recruitment of more and more satellite mesenchymal stem cells, expressing PAX-7, in the nearby zone of muscle injury.
Observations and results
In group I
It was noted on H&E examination that sections from Zone A showed diffuse necrosis in 100% samples with interspersed viable muscle fibres in 6.7% of samples. Whereas in Zone C, 73.3% of samples showed viable muscle fibres, out of which 18% samples also showed some amount of patchy necrosis. Rest 26% of samples from Zone C had no viable muscle fibres (Table 1). This could be attributed to incorrect zone determination intraoperatively, inadequate tissue sampling technique and inappropriate storage of samples.
On immunohistochemistry, 93% of samples from Zone A had either no or minimal expression of PAX-7 (score 0 and 1, respectively), while only 6% had score of 2 with moderate expression, with a mean score of 0.67 ± 0.617 (Fig. 2a, b). In Zone C, 73% of samples got a score of either 0 or 1, while another 13% of samples, showing moderate staining, had a score of 2. Around 13% of samples also showed significant staining with score of 3 in Zone C, with a mean score of 1 ± 1.069. In Zone B, around 87% samples had a score of either 0 or 1, while approximately 13% shared a score of either 2 or 3 (Figs. 2a, b, 3a, b; Table 2).
Photomicrographs showing immunohistochemistry staining for PAX-7 protein. a Injured muscle with PAX-7 positive nuclei along the periphery of the muscle indicating a score of 2 (Peroxidase anti-Peroxidase, ×400). b Injured muscle showing cluster of PAX-7 positive nuclei in between the degenerated muscle fibres indicating active regenerative activity (Peroxidase anti-Peroxidase, ×400)
An increasing trend towards the positive expression of PAX-7 staining was observed from Zone A to C. Despite relatively higher scores of PAX-7 in nearby zone of injury (Zone B and C) clearly indicating towards the increased expression of PAX-7 in these zones, it was not found statistically significant (Zone A–C: p value of 0.272).
In group II
On H&E examination, 100% of sections from the pre-debridement group showed diffuse necrosis with 6% of them also showing interspersed viable muscle fibres, whereas in post-debridement group, around 80% of samples had viable muscle fibres, with approx. 42% samples also having concomitant patchy necrosis. Also in 20% of samples, no viable muscle fibre could be traced (Table 1).
On immunohistochemistry staining in pre-debridement group, 67% samples had a score of either 0 or 1, while a score of 2 and 3 was seen in another 27% and 6% of samples, respectively, with a mean of 1.07 ± 0.961. In post-debridement group, around 47% and 33% samples had a score of 2 and 3, respectively, with moderate to significant staining with a mean of 2.07 ± 0.884. While only 20% showed a score of either 0 or 1 with either no or minimal staining (Figs. 2a, b, 3a, b; Table 2).
The data above clearly showed relatively increased expression of PAX-7 with higher score of 2 and 3 in post-debridement samples in group II patients, thus indicating a more marked tissue regeneration response in nearby healthy muscle tissue in zone of injury. Also, this increase was found to be statistically significant with p value 0.007.
Discussion
The rising incidence of mangled extremity along with aftermath of social, psychological and functional impairment of patient has put a significant economical burden over the society. Not only the surgery, whether amputation or limb salvage, but also its complications in postoperative period has a great impact on patient and the society as a whole. Along with various conventional measures and innovative techniques like thorough debridement, high-grade antibiotics, early vascular and microscopic nerve repair, etc., many different perspectives are now being considered in order to better tackle these problems [2, 3, 6]. A lot of research work is going on at gene level that enlightens us, altogether, with new concepts of tissue healing and reparative process. PAX-7 is one such transcription factor that attracted many researches in recent decades based on its potential to recruit and stimulate more and more mesenchymal satellite stem cells following muscle injury. Few studies have clearly demarcated that PAX-7 protein is able to drive transcription in quiescent, activated and proliferating satellite cells. Further, the expression of PAX-7 is downregulated in those satellite stem cells that undergo terminal differentiation but is maintained and remains transcriptionally active in those that opt out of immediate differentiation [8,9,10,11,12,13, 23]. Various English studies have shown that the increased expression of PAX-7 in skeletal muscle post-injury may predict the good outcome after surgery and may fasten the recovery process [16,17,18,19,20,21,22,23].
Keeping the future potential of PAX-7 in mind, we conducted a pilot study including 30 patients that reported to the emergency department of our institute. In this study, young male constitutes the majority, with 56.6% of patients falling in age group of 20–40 years. Out of 30, only two were female and rest were males. Road traffic accident was being the most common mode of injury (Table 3).
An extensive literature search was done beforehand (Table 4). Around 1297 and 1139 articles in Pubmed and Medline database could be found on PAX-7, respectively. On further refining our search, total of 69 articles with MeSH (PAX-7 and muscle regeneration and immunohistochemistry) could be traced in Pubmed. Out of these 69 studies, 10 most relevant studies were included in the final review after screening all abstracts, removing duplicates and obtaining full text. These studies highlight the different aspects of PAX-7 and PAX-7 positive satellite stem cells of skeletal muscle, in either human or animal study population (Table 5).
These studies, mostly, as indirect evidence enlightens the indispensable role of PAX-7 in regenerative process of skeletal muscle in different physiological and pathological scenarios such as neuromuscular dystrophies and in the stressful event such as muscle injury as a result of trauma and strenuous physical training and detraining (Table 5). Till now, no literature could be traced that highlights the role of PAX-7 in mangled extremity (MeSH: PAX-7 and mangled extremity; PAX-7 and mangled extremity and immunohistochemistry; PAX-7 and MESS score) (Table 4).
Satellite cells are the stem cells present between the sarcolemma of the myofibre and basement membrane, first recognised in frog skeletal muscle by electron microscopy. The CD 56 and PAX-7 are the two potential surface marker for identification of these satellite cells. The most important feature of satellite cell is their ability to enter the cell cycle, unlike regular myonuclei, and thereby replenishing its own population and regenerating muscle fibre in the event of injury. It will be very unlikely that in resting state, high number of satellite cells is active [8,9,10,11,12]. Mackey et al. in their study observed varying proportion of activated satellites cells in resting state, in single bout of isometric muscle stimulation and in event of light and heavy resistance training. He observed maximum recruitment of satellite cells (mean 10%) in single bout of isometric stimulation group whereas minimum (mean 1.3%) in resting group [13].
Lepper et al. [14] in their study demonstrated that “the genetic ablation of PAX-7 positive satellite stem cells completely blocks regenerative myogenesis either following injury to the tibialis anterior (TA) muscle in a mice”. Likewise, Seale et al. [15] in their study showed that the adult satellite stem cells taken from uninjured muscle of mice have no regeneration potential, whereas on the other hand, stem cells isolated from regenerating muscle were capable of giving rise to myoblast expressing PAX-7 as transcription factor. These studies signify the role of PAX-7 as an important regulator of muscle regeneration and repair in the event of muscle injury.
In a study conducted by Hamilton et al. [16] on 29 patients, the preoperative and postoperative muscle power and post-total knee replacement were graded and compared. The results were correlated with the degree of expression of PAX-7 positive satellite cells in biopsies taken from vastus lateralis at the time of surgery. He observed a strong correlation of satellite cell number and expression of PAX-7 with the improvement in patient power output postoperatively. The study highlights the indispensable regenerative reserves of skeletal muscle in the form of PAX-7 positive satellite cells that are recruited and activated in the stressful event like surgery, thereby optimising the adequate muscle power and strength.
Based on these indirect but concrete evidence from the literature, we believe that there may be some potential role of Pax-7 in influencing and guiding the postoperative event up to some extent [8,9,10,11,12,13,14,15,16,17,18,19,20,21,22]. This study has been conducted in order to further extend the utility of PAX-7 and satellite cells in the clinical setting of trauma and muscle injury.
In our study, all the sections were thoroughly examined under microscope with PAX-7 antibody stain. A differential staining pattern of PAX-7, thus observed in samples from both the groups. In group I patient, higher expression of PAX-7 with scores of 2 and 3 was noted in Zone C followed by Zone B as compared to Zone A. Likewise, the similar trend of staining was observed in group II patients on comparison of post-debridement samples with pre-debridement samples. We also noted this increasing trend of staining as statistically significant in only group II patients. The data from our study clearly showed increased expression of PAX-7 in the nearby areas of injury as a consequence of activation of tissue reparative cascade that subsequently deploy more and more satellite mesenchymal cells.
Moreover, higher expression of PAX-7 indicates greater strength of this reparative cascade that may fasten the recovery process and may lead to early rehabilitation and less wound complications [15,16,17,18,19,20,21,22]. So, we believed that patients with higher staining scores of PAX-7 in Zone C or post-debridement may exhibit lesser postoperative complication due to higher activation of regenerating and repairing cascade. Although no clear cut relation could be established between PAX-7 and the postoperative complications like infection and wound dehiscence in our study, the potential of PAX-7 in future could not be under-emphasised and neglected.
These shortcomings of studies could be attributed to small study group, limited resources and paucity of literature in existence. More research work, better resources and larger studies need to be conducted in future in order to further strengthen our hypothesis.
Conclusion
It was concluded that the expression of PAX-7 is definitely increased in the muscle tissue near the zone of injury in an attempt to accelerate the repair and regeneration of tissue.
It further strengthens our hypothesis that the PAX-7 has a definite role to play in predicting the regeneration ability and potential of traumatised muscle fibres and thereby may predict for better surgical outcome. Therefore, we strongly believe that, if explored meticulously in future, PAX-7 may have a predictive role, in association with various other blood or tissue markers, in deciding for limb salvage versus amputation or in predicting chances of postoperative complications like infection, delayed amputation, revision surgery, etc. However, many more studies may need to be conducted in near future with larger study cohorts and better resources in order to substantiate the exact role of PAX-7 markers in patients with mangled extremity. This study is just a baby step and a food for thought towards the various discoveries that need to be addressed in future.
References
Scalea TM, DuBose J, Moore EE, West M, Moore FA et al (2012) Western Trauma Association critical decisions in trauma: management of the mangled extremity. J Trauma Acute Care Surg 72(1):86–93
Gopinathan NR, Santhanam SS, Saibaba B, Dhillon MS (2017) Epidemiology of lower limb musculoskeletal trauma with associated vascular injuries in a tertiary care institute in India. Indian J Orthop 51(2):199
Harris AM, Althausen PL, Kellam J, Bosse MJ, Castillo R (2009) Lower Extremity Assessment Project (LEAP) Study Group. Complications following limb-threatening lower extremity trauma. J Orthop Trauma 23(1):1–6
Ball CG, Rozycki GS, Feliciano DV (2009) Upper extremity amputations after motor vehicle rollovers. J Trauma 67:410–412
Bosse MJ, MacKenzie EJ, Kellam JF, Burgess AR, Webb LX et al (2002) An analysis of outcomes of reconstruction or amputation after leg-threatening injuries. N Engl J Med 347:1924–1931
Gupta A, Wolff TW (1995) Management of the mangled hand and forearm. J Am Acad Orthop Surg 3:226–236
Korompilias AV, Beris AE, Lykissas MG, Vekris MD, Kontogeorgakos VA et al (2009) The mangled extremity and attempt for limb salvage. J Orthop Surg Res 4:4
Relaix F, Montarras D, Zaffran S, Gayraud-Morel B, Rocancourt D et al (2006) Pax3 and Pax7 have distinct and overlapping functions in adult muscle progenitor cells. J Cell Biol 172(1):91–102
Yin H, Price F, Rudnicki MA (2013) Satellite cells and the muscle stem cell niche. Physiol Rev 93(1):23–67
Von Maltzahn J, Chang NC, Bentzinger CF, Rudnicki MA (2012) Wnt signaling in myogenesis. Trends Cell Biol 22(11):602–609
Birbrair A, Delbono O (2015) Pericytes are essential for Skeletal Muscle Formation. Stem Cell Rev Rep 11(4):547–548
Von Maltzahn J, Jones AE, Parks RJ, Rudnicki MA (2013) Pax7 is critical for the normal function of satellite cells in adult skeletal muscle. Proc Natl Acad Sci 110(41):16474–16479
Mackey AL, Kjaer M, Charifi N, Henriksson J, Bojsen-Moller J et al (2009) Assessment of satellite cell number and activity status in human skeletal muscle biopsies. Muscle Nerve 40(3):455–465
Lepper C, Partridge TA, Fan CM (2011) An absolute requirement for Pax7-positive satellite cells in acute injury-induced skeletal muscle regeneration. Development 138(17):3639–3646
Seale P, Sabourin LA, Girgis-Gabardo A, Mansouri A, Gruss P et al (2000) Pax7 is required for the specification of myogenic satellite cells. Cell 102(6):777–786
Hamilton DF, McLeish JA, Gaston P, Simpson AH (2013) Muscle ‘regenerative potential’ determines physical recovery following total knee replacement. Bone Jt Res 2(4):70–78
Oustanina S, Hause G, Braun T (2004) Pax7 directs postnatal renewal and propagation of myogenic satellite cells but not their specification. EMBO J 23(16):3430–3439
Seale P, Ishibashi J, Scimè A, Rudnicki MA (2004) Pax7 is necessary and sufficient for the myogenic specification of CD45+:Sca1+ stem cells from injured muscle. PLoS Biol 2(5):E130
Kadi F, Schjerling P, Andersen LL, Charifi N, Madsen JL et al (2004) The effects of heavy resistance training and detraining on satellite cells in human skeletal muscles. J Physiol 558(Pt 3):1005–1012
Kadi F, Charifi N, Denis C, Lexell J, Andersen JL et al (2005) The behaviour of satellite cells in response to exercise: what have we learned from human studies? Pflugers Arch 451(2):319–327
Sambasivan R, Yao R, Kissenpfennig A, Van Wittenberghe L, Paldi A et al (2011) Pax7-expressing satellite cells are indispensable for adult skeletal muscle regeneration. Development 138(17):3647–3656
Noehren B, Andersen A, Hardy P, Johnson DL, Ireland ML et al (2016) Cellular and morphological alterations in the vastus lateralis muscle as the result of ACL injury and reconstruction. JBJS 98(18):1541–1547
Zammit PS, Relaix F, Nagata Y, Ruiz AP, Collins CA et al (2006) Pax7 and myogenic progression in skeletal muscle satellite cells. J Cell Sci 119(Pt 9):1824–1832
Acknowledgements
This work has been funded by Indian Council of Medical Research (ICMR) (No.3/2/Sept.2016/PG-Thesis-HRD(8) Dated: 4.10.2016), Department of Health Research, New Delhi, and constituted part of a thesis submitted by the principal author.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest from any of the authors.
Ethical approval
The study was approved by the Institute’s Ethical Committee and was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was taken from the patients at the time of enrolment and the study procedure was explained in detail to all the enrolled patients and they were made to understand that they could withdraw from the study at any point of the study period. The study has not altered any of the management protocols of these patients. Identity of the participants was kept confidential.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kansal, R., Kanojia, R.K., Kumar, V. et al. Role of PAX-7 as a tissue marker in mangled extremity: a pilot study. Eur J Orthop Surg Traumatol 29, 1131–1140 (2019). https://doi.org/10.1007/s00590-019-02410-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-019-02410-w