Abstract
Introduction
Osteochondral lesions of the patellofemoral joint (OLPFJ) are defects of the cartilage surface and subchondral bone, which often require surgical treatment. Reparative treatments have shown some limitations in the long-term follow-up. The one-step bone marrow-derived cells transplantation (BMDCT) achieved good to excellent results in the treatment of osteochondral lesions of the femoral condyles. The aim of this study was to report the 48-month clinical and radiological results among 28 patients with OLPFJ treated with the one-step BMDCT technique associated with the anteromedialization tibial tuberosity (AMTT).
Materials and methods
Twenty-eight patients from 2010 to 2013 with OLPFJ underwent the BMDCT with the one-step technique associated with the AMTT. Clinical evaluation was performed at 6, 12, 18, 24, 36 and 48 months after surgery using the Kujala PF scale, the IKDC score and the Tegner activity scale. Eighteen lesions were located on patella and ten lesions on trochlea.
Results
The preoperative Kujala score improved from 68.2 ± 4.7 to 87.2 ± 1.2 at the mean final follow-up, while the IKDC subjective score improved from 55.1 ± 6.2 to 92.13 ± 5.5. Tegner scale showed an increase from 1.7 ± 1.3 preoperatively to 5.3 ± 2.7 at the final follow-up. MRI analysis at 24-month follow-up showed an overall good filling of the lesions.
Discussion and conclusions
The one-step BMDCT associated with the AMTT permitted good clinical results durable over time with a high rate of patients’ satisfaction. These results confirm the validity of the one-step technique also in patellofemoral joint.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
From the very first description of osteochondral lesions in patellofemoral joint given by the Norwegian physician M.F.L. Sinding-Larsen in 1921, it was immediately clear how treating this pathology would be difficult [1]. The articular surface of the patella is affected in 11–36% of the whole osteochondral lesions involving the knee joint [2]. Etiology of patellofemoral cartilage lesions includes chronic repetitive microtrauma or major acute trauma, frequently a patellar dislocation. The incidence of patellofemoral osteochondral lesion after a patellar dislocation is reported to be around 95% [3, 4]. Patients involved are often young adults who practice sport activities with high functional demands. Various surgical techniques addressing cartilage patellofemoral lesions have been reported in the literature. Reparative procedures, such as debridement with removal of the damaged osteochondral fragment [5], drilling and microfractures, are widely used by most authors. Even if the aim of these procedures is to allow cartilage restoration by stimulating bone marrow cells, they also stimulate the regeneration of a fibrocartilaginous tissue, which is rich in collagen type I rather than in type II. This has lower biomechanical strength and elasticity compared with hyaline native tissue [6], thus leading to decreased clinical scores over time.
In recent years, various surgical options, such as osteochondral autograft transfer (OAT) and autologous chondrocyte implantation (ACI) [7,8,9], have been proposed to restore an adequate cartilaginous layer. The latter has shown favorable results with low morbidity, as the procedure can be performed entirely arthroscopically. However, high costs, due to cell expansion, and the need of two consecutive surgeries, still remain the major drawbacks.
In the last decade, the use of bone marrow-derived cells (BMDC) for the treatment of osteochondral lesions, in both the knee and ankle joint, has increased [10,11,12]. BMDC applied with the one-step technique is a single-step procedure, with no need for cells culture or expansion, with a limited morbidity, related to bone marrow cells aspiration from the posterior iliac crest, and with decreased total costs compared to ACI.
Although patellofemoral osteochondral lesions are less frequent than condylar lesions, some studies dealing with ACI are reported in the literature [13].
Gobbi et al. recently published a non-randomized prospective trial, showing that both ACI transplantation and BMDC transplantation are effective for the treatment of large patellofemoral chondral lesions at a follow-up of at least 3 years.
Brittberg et al. [13] stated that when a patellofemoral (PF) malalignment is also present and not surgically addressed, it may affect the final clinical outcome of the PF cartilage procedure, with only 28% of the patients having good or excellent result in 36-month follow-up. Some papers and a recent systematic review have come to the conclusion that there are better clinical outcomes when also a realignment procedure was correctly performed in association with cartilage reparative procedures [14,15,16,17].
The aim of this study was to present the clinical outcomes at a mean final follow-up of 48 months, in a group of patients who underwent BMDCT through the one-step technique associated with an anteromedialization tibial tuberosity (AMTT).
Materials and methods
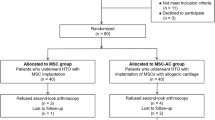
From December 2010 to November 2013, 28 consecutive patients affected by focal patellofemoral osteochondral lesions were treated with one-step BMDC transplantation associated with AMTT (Fig. 1). Inclusion criteria were: patients between 18 and 60 years old who complained of patellofemoral symptoms, like anterior knee pain, especially descending and ascending stairs, swelling, locking or knee failure who underwent conservative treatment without success for at least 6 months; grade III–IV osteochondral lesion (ICRS classification) of the patella or trochlea ranging from 1.0 to 4.00 cm2; and tibial tubercle–trochlear groove distance (TT–TG) over 18 mm measured with CT scan. Exclusion criteria were: age < 18 or > 60 years, untreated tibio-femoral misalignment, presence of kissing lesions (patella + trochlea), advanced osteoarthritis, presence of concomitant meniscal tear, concomitant anterior cruciate ligament (ACL) or posterior cruciate ligament (PCL) deficiency. Patients with infective, metabolic or inflammatory pathologies were also excluded from the study.
The study was approved by the ethics committee of the authors’ institution, and a written informed consent form was signed by all patients enrolled in this study.
Surgical technique and rationale
All patients received BMDC transplantation with the one-step technique, associated with AMTT. The one-step technique relies on the implantation of mesenchymal stem cells together with all mononuclear cells in order to transfer to the lesion site the high regenerative potential present in the bone marrow [10,11,12]. In fact, autologous bone marrow contains not only stem cells and precursor cells prone to differentiate into bone and cartilage, but also accessory cells capable of supporting angiogenesis by producing several growth factors. The day before surgery, through a Vivostat system (Vivolution A/S, 3460 Birkeroed, Denmark), a sample of 120 ml was taken from the patient’s venous blood and then processed to obtain 6 ml of platelet-rich fibrin (PRF). PRF was frozen at − 35 °C. PRF is important to obtain growth factors and a fibrin clot to fasten the implanted biomaterial.
The next day, in a sterile regimen, the patient under spinal anesthesia was positioned in prone decubitus. PRF was defrosted while the bone marrow cells aspiration was performed. A marrow needle (size 11 G 9 100 mm) was inserted into the spongy bone of the posterior iliac crest, 3 cm deep: The purpose was to fill a 20-ml syringe, internally coated with calcium–heparin solution, with 5 ml of bone marrow. Other 5 ml was aspirated after rotating the needle by 90 degrees. In order to collect 5 ml of bone marrow at each aspiration, other rotations were performed with a moderate withdrawing, as small fractions from different points allow to maximize harvesting and reduce blood dilution. The procedure was repeated 3–4 times using the same skin opening. Sixty milliliters of bone marrow was collected. The aspirated bone marrow was then concentrated, achieving 6 ml of liquid rich in nucleated cells including stem cells, monocytes, lymphocytes and bone marrow-resident cells. Cell separation and consequent concentration were performed through a Smart PReP1 device (Harvest Technologies Corp, Plymouth, MA) and a dedicated BMAC1 kit (Harvest Technologies Corp). Before fastening and setting the tourniquet at 280 mmHg, the patient was put in supine position and arthroscopy was performed through two standard approaches, anteromedial and anterolateral. Patellar tracking was observed through the anterolateral portal before and at the end of the procedure. The severity and location of cartilage damage were noted together with tracking of the patella with passive knee range of motion. The cartilage lesion was identified and debrided to obtain a stable healthy edge around the defect. At the same time, composites to be implanted were prepared: 2 ml of marrow concentrate was loaded on a hydrophilic hyaluronate membrane, sized and shaped depending on the lesion. No filling of the bone defect was applied. After cell absorption, 1 ml of PRF was added through a dedicated pen. Successively, a 6-cm lateral parapatellar incision, approximately 1 cm lateral to the patellar tendon, was performed. Longitudinal lateral parapatellar incision was performed from the inferior pole of the patella, to the distal end of the tibial tubercle. The location of the chondral lesion was also viewed through arthrotomy approach and confirmed (Fig. 2). The distal end of the osteotomy was marked 3 cm distally to the patellar tendon. A complete sagittal osteotomy under the tibial tubercle was performed. The tibial tubercle bone fragment was released and displaced 10–15 mm anteromedially. The tibial tubercle was fixed with two unicortical cancellous bone screws without washer, inserted perpendicular to the tibial tubercle, from anterior to posterior. Through the same parapatellar incision, the biomaterial was finally placed on the lesion. The biomaterial was regularized using a flat probe, and the previously provided PRF was applied on the lesions to promote fastening of the implant and regeneration stimulation (Fig. 3). Multiple flex extensions were performed to check the stability of the implant. Conventional closure of the skin was performed.
Postoperative Rehabilitation
A hinged knee brace was positioned in all patients after surgery. Continuous passive motion (CPM) (0°–35°; 1 cycle/min) was initiated on the first postoperative day for 6–8 h per day. Literature widely describes beneficial results of CPM enhancing joint nutrition, cartilage healing and lowering rate of postoperative adhesions [18]. Range of motion (ROM) was gradually increased every week, with the aim to achieve 90° of flexion 6 week postoperatively. Patients were allowed partial weight bearing, 6 weeks after surgery, due to tibial tubercle osteotomy. Return to full activity was not permitted until 8 months after surgery in order to protect the newly implanted graft maturation.
Clinical evaluation
Clinical evaluation was performed at 6, 12, 18, 24, 36 and 48 months of follow-up. All patients were requested to answer the IKDC subjective evaluation, the Tegner sports activity score, the Kujala patellofemoral scale and the EQ-5D visual analog scale, preoperatively and at the established follow-ups. All patients were preoperatively assessed for malalignment of the patellofemoral joint, including measurement of tibial tubercle–trochlear groove distance (TT–TG). TT–TG distance is the measurement currently utilized for estimating the amount of tibial tubercle medialization required. Previous studies reported a normal TT–TG between 10 and 15 mm, with a TT–TG over 20 mm considered as abnormal index [19]. High-resolution magnetic resonance imaging (MRI) evaluation was conducted preoperatively and at 24 months of follow-up.
Statistical analysis
All continuous data are expressed in terms of mean and standard deviation of the mean. Paired t test (normal distributed data) and Wilcoxon test (non-normal distributed data) were performed to test differences between follow-up times. The primary end point of this study was the mean change in the overall condition score from baseline to follow-up. The secondary end point was to investigate the relationships between grouping variables through Pearson Chi-Squared test, calculated by the exact method for small samples. Statistical analysis was carried out with the Statistical Package for the Social Sciences (SPSS) software version 15.0 (SPSS Inc., Chicago, USA).
Results
No serious adverse events were observed neither intraoperatively nor postoperatively. A statistically significant improvement in all scores was observed after 2 years of follow-up. Improvements remained stable or increased over time, as shown at the over 2-year follow-up evaluation. The IKDC objective score showed 14% normal or nearly normal knees preoperatively (3A, 1B, 22C and 2D), compared to 92% at 2-year follow-up (16A, 10B and 2C). The IKDC subjective score showed a statistically significant improvement from the preoperative condition (55.1 ± 6.2) at both 24-month (77.65 ± 9.77) and 48-month follow-up (92.13 ± 5.5) (p < 0.0005) (Fig. 4).
The Kujala patellofemoral scale showed a statistically significant increase from a mean preoperative score of 68.2 ± 4.7 to 82.2 ± 1.7 at 24 months after surgery and 87.2 ± 1.2 at 48-month follow-up (Fig. 5).
Self-assessment of quality of life (EQ-VAS) showed a significant improvement from preoperative evaluation (43.2 ± 12.8) at 2-year (68.5 ± 11.1) and 4-year follow-ups (87.4 ± 16.3) (paired t test; p < 0.0005); an improvement was also assessed when comparing the results obtained at 2- versus 4-year follow-up (paired t test; p = 0.029) (Fig. 6).
The pre-injury Tegner score was 6.5 ± 2.1, while the preoperative value was 2.27 ± 1.3. This improved to 5.7 ± 2.6 at 2-year follow-up and to 5.3 ± 2.7 at the final follow-up. The level of sport activity at 2 and 4 years was significantly lower compared to the pre-injury level (paired t test; p < 0.0005); however, these results showed a statistically significant improvement (paired t test; p < 0.0005) stable over time, with no significant difference between the 2- and the 4-year follow-ups (Fig. 7).
A further evaluation was performed to analyze the influence of the lesion site on the Kujala PF score. Patients with trochlear defects achieved a final mean Kujala PF score of 88.3 ± 1.2 which was higher compared to patients with patellar defects (83.7 ± 2.3), although a statistically significant difference was not reached (Figs. 8, 9). Furthermore, Kujala PF scores were not statistically influenced by the age of the patients, but better results were achieved by patients in the 30–40 age group (Fig. 10).
MRI control at 24-month follow-up, by means of the MOCART score, showed a regeneration of subchondral bone and cartilaginous tissue. A relationship was found between Kujala PF score at 24 months and signal intensity, although not statistically significant. Patients with hyperintense signal (11 patients) had a IKDC score of 82 ± 1.3 at 24-month follow-up, while patients with isointense signal (19 patients) had a Kujala PF score of 85.1 ± 5. No other correlation was found between clinical score and MOCART parameters.
Discussion
Several treatments have taken place in the last two decades for the treatment of osteochondral lesions of the patellofemoral joint, including microfractures, debridement/chondroplasty, periosteal transplantation and ACI. The microfracture technique is able to provide a short-term clinical improvement, which is affected by a clinical deterioration over time, mainly due to the lower quality of the regenerated tissue [20, 21]. Lorentzon et al. described 65% excellent results in 26 patients treated with periosteal transplantation without any chondrocytes for patellar full-thickness chondral defects, even if after a mean follow-up of 42 months, only 46% of them were able to resume sports [21]. Another study by Schonholtz and Ling reported 49% of good or excellent results in 41 knees affected by patellar chondropathies and treated by chondroplasty technique [22]. Even though 78% of study participants reported satisfactory results after a mean follow-up of 40 months, biopsy samples showed a low-quality cartilaginous tissue. On the other hand, Minas and Bryant reached 71% of good or excellent results when treating patellofemoral chondropathies with first-generation ACI [15]. In spite of this, after a mean follow-up of 2 years, a failure rate of 18% was noted [23]. Even if many new surgical methods have been proposed, a clear superiority of one technique versus the others has not been documented.
Mesenchymal stem cells represent 2–3% of the total mononuclear cells in bone marrow and have the ability to differentiate into various lineages, including osteoblasts and chondroblasts [26,27,28,29]. The rationale of the one-step technique is the idea to transplant the entire bone marrow cellular pool instead of isolated and expanded mesenchymal stem cells. BMDC transplantation, associated with patellar realignment, has shown to be able to achieve satisfactory mid-term results throughout a one-step technique with considerably lower costs compared to others techniques, such as ACI. The first surgical treatment for patellar chondral lesions with ACI performed by Brittberg et al. [24] achieved only 28% of good/excellent result at 36 months of follow-up. In recent years, some studies of ACI combined with the correction of associated factors have shown favorable results [14, 16, 25]. In order to achieve a better final score, we decided to combine BMDC with AMTT, even though we were aware of the greater morbidity after a realignment procedure.
The present study showed a significant improvement in both the objective and subjective IKDC score and the Kujala PF score at the mean final follow-up of 4 years. With regard to sports activity assessed by the Tegner score, a gradual increase at each follow-up was observed, even though pre-injury activity level was never reached. Pain relief assessment, evaluated with the EQ-VAS, significantly improved at each follow-up, with the greatest improvement between the evaluations at 36 and 48 months. A further evaluation was performed in order to investigate the role of the lesions site, thus comparing the values of the Kujala PF score with the injury site. Patients with isolated trochlear lesion achieved better clinical scores than those with isolated patellar. Even though the reason was unclear, we hypothesized that the greater amount of bone marrow in the trochlear groove influenced cartilage regeneration in a positive manner.
Major drawbacks of this study are the lack of a control group where the same surgical procedures (AMTT) could be associated with another cartilage repair technique, the limited number of patients and the lack of byoptic samples or a T2-mapping MRI evaluation. Nevertheless, to our knowledge there are only a few studies in the literature and the majority are case reports, which use mesenchymal stem cell to repair cartilage lesions in the femoral patella [30,31,32]. Furthermore, we have not found any mention of the combination with any realignment procedure.
Conclusions
The particular anatomy of PF joint characterized by high content of bone marrow is suitable for biological chondral repair. The correction of background factors, such as malalignment with AMTT, led to significant improvement in every clinical score from the pre-op situation to the final mean follow-up. MRI examination showed a promising growth of bone and cartilage, nearly complete defect filling and satisfactory integration of the graft at follow-up in 80% of cases. Although further studies with longer follow-up are required to confirm these results, the one-step technique has proven to be a good and reliable option for patella femoral chondral lesions, able to overcome the major drawbacks of previous techniques with comparable results.
References
Anderson DM, Michelle AE (2004) Mosby’s medical, nursing, and allied health dictionary, vol 6. Piccin, Venice
Curl WW, Krome J, Gordon ES, Rushing J, Smith BP, Poehling GG (1997) Cartilage injuries: a review of 31,516 knee arthroscopies. Arthroscopy 13:456–460
Hunziker EB (2002) Articular cartilage repair: basic science and clinical progress: a review of the current status and prospects. Osteoarthr Cartil 10:432–463
Nomura E, Inoue M, Kurimura M (2003) Chondral and osteochondral injuries associated with acute patellar dislocation. Arthroscopy 19:717–721
Messner K, Maletius W (1996) The long-term prognosis for severe damage to weight-bearing cartilage in the knee: a 14-year clinical and radiographic follow-up in 28 young athletes. Acta Orthop Scand 67:165–168
Hangody L, Kish G, Karpati Z, Szerb I, Udvarhelyi I (1997) Arthroscopic autogenous osteochondral mosaicplasty for the treatment of femoral condylar articular defects: a preliminary report. Knee Surg Sports Traumatol Arthrosc 5:262–267
Peterson L, Minas T, Brittberg M et al (2000) Two- to 9-year outcome after autologous chondrocyte transplantation of the knee. Clin Orthop 374:212–234
Gobbi A, Kon E, Berruto M, Filardo G, Delcogliano M, Boldrini L, Bathan L, Marcacci M (2009) Patellofemoral full-thickness chondral defects treated with second-generation autologous chondrocyte implantation: results at 5 years’ follow-up. Am J Sports Med 37(6):1083–1089
Macmull S, Jaiswal PK, Bentley G, Skinner JA, Carrington RWJ, Briggs TW (2012) The role of autologous chondrocyte implantation in the treatment of symptomatic chondromalacia patellae. Int Orthop 36(7):1371
Cavallo C, Desando G, Cattini L, Cavallo M, Buda R, Giannini S, Facchini A, Grigolo B (2013) Bone marrow concentrated cell transplantation: rationale for its use in the treatment of human osteochondral lesions. J Biol Regul Homeost Agents 27(1):165–175
Giannini S, Battaglia M, Buda R, Cavallo M, Ruffilli A, Vannini F (2009) Surgical treatment of osteochondral lesions of the talus by open-field autologous chondrocyte implantation: a 10-year follow-up clinical and magnetic resonance imaging T2-mapping evaluation. Am J Sports Med 37(Suppl 1):112S–118S
Giannini S, Buda R, Faldini C et al (2005) Surgical treatment of osteochondral lesions of the talus (OLT) in young and active patients: guidelines for treatment and evolution of the technique. J Bone Joint Surg Am 87:28–41
Brittberg M, Lindahl A, Nilsson A, Ohlsson C, Isaksson O, Peterson L (1994) Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med 331(14):889–895
Mandelbaum B, Browne JE, Fu F, Micheli LJ, Moseley JB, Erggelet C, Anderson AF (2007) Treatment outcomes of autologous chondrocyte implantation for full-thickness articular cartilage defects of the trochlea. Am J Sports Med 35(6):915–921
Minas T, Bryant T (2005) The role of autologous chondrocyte implantation in the patellofemoral joint. Clin Orthop Relat Res 436:30–39
Peterson L, Brittberg M, Kiviranta I, Akerlund EL, Lindahl A (2002) Autologous chondrocyte transplantation: biomechanics and long-term durability. Am J Sports Med 30(1):2–12
Trinh T, Harris J, Siston R, Flanigan D (2013) Improved outcomes with combined autologous chondrocyte implantation and patellofemoral osteotomy versus isolated autologous chondrocyte implantation. Arthroscopy 29(3):566–574
Salter RB (1994) The physiological basis of continous passive motion for articular cartilage healing and regeneration. Hand Clin 10:211–219
Ding DY, Kanevsky R, Strauss EJ, Jazrawi LM (2016) Anteromedialisation tibial tubercle osteotomy for recurrent patellar instability in young active patients: a retrospective case series. Injury 47(3):7373–41
Kreuz PC, Steinwachs MR, Erggelet C et al (2006) Results after microfracture of full-thickness chondral defects in different compartments in the knee. Osteoarthr Cartil 14:1119–1125
Saris DB, Vanlauwe J, Victor J et al (2008) Characterized chondrocyte implantation results in better structural repair when treating symptomatic cartilage defects of the knee in a randomized controlled trial versus microfracture. Am J Sports Med 36:235–246
Lorentzon R, Alfredson H, Hildingsson C (1998) Treatment of deep cartilage defects of the patella with periosteal transplantation. Knee Surg Sports Traumatol Arthrosc 6:201
Schonholtz GJ, Ling B (1985) Arthroscopic chondroplasty of the patella. Arthroscopy 1:92–96
Brittberg M, Lindahl A, Nilsson A, Ohlsson C, Isaksson O, Peterson L (1994) Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med 331:889–895
Farr J II (2008) Autologous chondrocyte implantation and anteromedialization in the treatment of patellofemoral chondrosis. Orthop Clin N Am 39:329–335
Bosnakovski D, Mizuno M, Kim G, Takagi S, Okumura M, Fujinaga T (2006) Chondrogenic differentiation of bovine marrow mesenchymal stem cells (MSCs) in different hydrogels: influence of collagen type II extracellular matrix on MSC chondrogenesis. Biotechnol Bioeng 93:1152–1163
Dominici M, Pritchard C, Garlits JE, Hofmann TJ, Persons DA, Horwitz EM (2004) Hematopoietic cells and osteoblasts are derived from a common marrow progenitor after bone marrow transplantation. PNAS 101:11761–11766
Kacena MA, Gundberg CM, Horowitz MC (2006) A reciprocal regulatory interaction between megakaryocytes, bone cells and hematopoietic stem cells. Bone 39:978–984
Longobardi L, O’Rear L, Aakula S, Johnstone B, Shimer K, Chytil A, Horton WA, Moses HL, Spagnoli A (2006) Effect of IGF-I in the chondrogenesis of bone marrow mesenchymal stem cells in the presence or absence of TGF-beta signaling. J Bone Miner Res 21:626–636
Tsujii A, Hiramatsu K, Shimomura K, Kobayashi M, Mera H, Wakitani S, Nakamura N, Horibe S, Mitsuoka TJ (2018) Long-term results of autologous bone marrow mesenchymal stem cell transplantation for cartilage defects in the patella: Two case reports with more than 18 years of follow-up. Orthop Sci S0949–2658(18):30036–30038
Wakitani S, Nawata M, Tensho K, Okabe T, Machida H, Ohgushi H (2007) Repair of articular cartilage defects in the patello-femoral joint with autologous bone marrow mesenchymal cell transplantation: three case reports involving nine defects in five knees. J Tissue Eng Regen Med 1(1):74–79
Wakitani S, Mitsuoka T, Nakamura N, Toritsuka Y, Nakamura Y, Horibe S (2004) Autologous bone marrow stromal cell transplantation for repair of full-thickness articular cartilage defects in human patellae: two case reports. Cell Transpl 13(5):595–600
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Buda, R., Baldassarri, M., Perazzo, L. et al. A useful combination for the treatment of patellofemoral chondral lesions: realignment procedure plus mesenchymal stem cell—retrospective analysis and clinical results at 48 months of follow-up. Eur J Orthop Surg Traumatol 29, 461–470 (2019). https://doi.org/10.1007/s00590-018-2310-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-018-2310-z