Abstract
Background
Stand-alone cage-assisted anterior cervical discectomy and fusion (ACDF) has proved to be safe and effective procedure for treatment of mono-segmental cervical degenerative stenosis (CDS). However, the success rate has reported to decline as the number of levels increases. The aim of this prospective study was to evaluate the short-term results of multilevel ACDF using stand-alone polyetheretherketone (PEEK) cages.
Patients and methods
Twenty-eight patients (16 males and 12 females; mean age 40.5 years) of symptomatic multilevel CDS were enroled in this study and completed a 2-year post-operative follow-up. All patients underwent contiguous multilevel ACDF, using indirect decompression and stand-alone PEEK cages, between 2009 and 2012. Ten patients underwent two-level fusions (group I), ten underwent three-level fusions (group II), and eight underwent four-level fusions (group III). The visual analogue scales of neck and arm pain and Odom’s criteria were used to evaluate clinical outcomes. Radiological evaluation was done to evaluate: fusion, cervical sagittal angle (CSA) and cage subsidence.
Results
There was a statistical significant improvement in clinical parameters and radiological CSA values in all groups post-operatively. This improvement was well maintained till final follow-up. Subsidence and non-union were encountered in seven and two fusion levels, respectively, with no significant differences between groups. All patients were satisfied and none of them had major complications or required revision surgery.
Conclusion
With proper patient selection, meticulous surgical technique and strict post-operative cervical bracing, the less-invasive indirect anterior cervical decompression technique augmented with stand-alone PEEK cage-assisted ACDF is an efficient and safe method for the treatment of multilevel CDS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cage-assisted surgery has been introduced as a valid alternative during anterior cervical discectomy and fusion (ACDF) procedures. Cage can replace the cortical part of the tri-cortical bone graft by providing a non-resorbable anterior load-bearing support that can restore cervical alignment and physiologic disc height immediately with elimination of donor site trauma [1–3]. Nevertheless, in multilevel ACDF procedures, the use of plate is regarded a routine practice to enhance stability and to increase fusion rate [4–8]. However, plates have their shortcomings as they are costly, technically demanding (requiring more lengthy operation and exposure) and fraught with many complications (e.g. compromising anterior neck vital structures, violation of adjacent disc and plate/screw migration or dislodgment) [2, 7–11]. Furthermore, the commonly used constrained locked plates are sometimes blamed for preventing controlled amount of settling which is crucial for compression at graft/end-plate interfaces during the early stage of graft incorporation [5].
The above-mentioned plate-related problems were a stimulus for using the synthetic cages in a stand-alone fashion, without plate fixation, based on the principle of distraction–compression concept [1, 3, 9, 10, 12–19]. Clinical outcomes have been encouraging in single-level procedures [1, 15, 16, 19], while controversy exists in their use alone in multilevel ACDF settings [2, 4, 8–10, 17–19]. Problems of cage subsidence, fusion segmental kyphosis and pseudarthrosis are major concerns, particularly in multilevel settings [9, 14–19].
In the literature, there is ongoing tendency to do extensive decompression during ACDF by sacrificing the posterior longitudinal ligament (PLL) and uncovertebral joint (UVJ) osteophytes [1, 2, 4, 8–10, 13–19]. However, sacrificing these structures can increase the operative time and potentially destabilize the spine markedly [5, 12, 20, 21]. To the author’s knowledge, almost all series in the literature that have evaluated the cage subsidence issue or multilevel ACDF failures used the extensive decompression technique with sequential PLL and UVJ resection as a routine practice. Coupling this unstable situation with the absence of rigid fixation in non-plated cage-assisted ACDF, it is predictable to get high rate of failures in multilevel procedures. The author’s hypothesis that the less-invasive indirect decompression technique, with preservation of PLL and UVJs, can provide a more suitable mechanical environment for reducing cage subsidence in selected cases of multilevel ACDF. If this goal can be achieved, then cost- and morbidity-related problems surrounding additional plate fixation could be eliminated.
This prospective study was conducted to report the author’s preliminary experience with stand-alone polyetheretherketone (PEEK) cages in selected patients of cervical degenerative stenosis (CDS) who underwent indirect decompression in 2-, 3- or 4-level ACDF procedures. The used protocol was also improved to overcome the previously documented risky factors, discussed in the literature [1, 4, 5, 9, 12, 15, 16], responsible for cage subsidence and pseudoarthrosis issues (Fig. 1). The stand-alone cages were compared for efficiency, safety and complications through a spectrum of level of involvement.
Illustrative diagram showing some important technical points used to improve the results of stand-alone cage procedures. a Multilevel cervical stenosis with collapsed discs, osteophytosis and mal-alignment. b In the absence of PLL, distraction (arrows) leads to uncontrolled separation of the bodies and realignment of the spine is difficult without cervical plates. c Preserved PLL acts as a fulcrum during gentle distraction (arrows), for opening the anterior column and restraining the distraction. Additionally, preservation of the dense cortical bone of the anterior osteophytes (asterisk) and anterior positioning of the cage (hash) are crucial for preventing subsidence. d The peripheral part of the end-plate was prepared for fusion by fine abrasion to preserve stability, while its central portion was additionally prepared with a curette to expose the cancellous bone (black irregular marker) to enhance early healing
Patient and methods
Between January 2009 and January 2012, a total of 28 patients underwent a contiguous multilevel stand-alone cage-assisted ACDF for symptomatic CDS in the author’s institution. All patients initially presented with an axial neck pain associated with cervical radiculopathy, unresponsive to a minimum of 3 months of conservative treatment, were included in this prospective study. There were 16 men and 12 women (Mean age 40.5 years, range 35–47.5 years). The inclusion criteria included cervical stenosis caused by anterior degenerative discs or osteophyte formation provided that the decompression could be resolved by discectomy alone without elimination of UVJs or PLL. Exclusion criteria included developmental cervical stenosis and cervical stenosis associated with: weakness, instability, severe kyphosis, previous surgery, infection, tumours or PLL ossification. Exclusion criteria also included cases with severe retro-vertebral stenosis that needs to drill out the end-plates or needs excessive removal of PLL for decompression [i.e. complete obliteration of the exit neural foramina in magnetic resonance imaging (MRI)]. Cases with documented vertebral osteoporosis, as proven by DEXA, and high-risk patients of non-union (e.g. corticosteroid therapy, renal failure and smoking) were also excluded.
All procedures followed were in accordance with the ethical standards of the responsible local institutional committee on human experimentation and with the Helsinki declaration of 1964 and its later amendments. Informed consent was obtained from all the patients for being included in this study. Every patient was given a code number and his anonymity was preserved (his personal data were omitted).
Surgical technique
All patients were operated through the standardized anterior approach after application of skull traction with routine use of somatosensory evoked potential or wake-up test. Levels of fusion were determined mainly according to clinical presentations and related MRI findings. Ten patients underwent 2-level fusion (group I), ten underwent 3-level fusions (group II), and eight underwent 4-level fusion (group III) for a total of 82 levels. No plate instrumentation was used. To decrease oesophageal oedema, oesophageal catheters were not allowed, while intravenous methylprednisolone and an intermittent retraction technique were used in all cases.
Segmental decompression was performed using high-resolution microscope. Annulus was incised, leaving its lateral anterior pillars, and discectomy was extended laterally up to the uncinate process, which marks the safe extent of lateral decompression. Decompression was completed indirectly by distraction without total removal of PLL or posterior osteophytes (Fig. 2). However, a mid-line small longitudinal window in PLL was created in some cases to remove accessible herniated disc fragments using special hooks. Great care was paid for removing only the cartilaginous part of end-plate and preservation of its cortical bony stock. Special care was also taken to preserve the dense cortical bone of the anterior osteophytes and to remove only their marginal portion at the plane of end-plate to obtain sufficient access to disc space (Fig. 1c). The peripheral part of end-plate was prepared for fusion by fine abrasion with a high-speed burr, while its central portion, corresponding to the central hole in the cage, was additionally prepared with a curette to expose the cancellous bone (Fig. 1d).
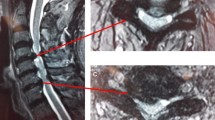
The rationale for using the indirect decompression technique in the study. a Impingement of the neural elements (red circular structure) in the foramen of collapsed mal-aligned degenerative spine. b After discectomy, distraction stretches the PLL, straightens the ligamentum flavum and increases the dimensions of neural foramen. So, the pinching on neural elements could be eliminated even in the presence of moderate size osteophytes. c Insignificant cage subsidence results in loss of some of the acquired correction. The decompression, though partially compromised, is still adequate (i.e. osteophytes is just touching the nerve root instead of kinking it) if the segment achieves early fusion, before major collapse, in a good alignment (color figure online)
ACDF was performed serially, in a proximal–distal direction, using PEEK cages over-packed with cancellous bone obtained from the anterior iliac crest by a core through a percutaneous mini-incision. Additional bone graft was packed posterior and around the cage. Cage diameter was selected to match the inherent dimensions of the patient’s disc spaces for covering a maximum of the end-plates. The cage was sized with trials without using Caspar retractor. During sizing, an additional slight manual traction was done gently via the skull traction. This gives a controlled extra-space, allowing a secure snug-fit insertion of the cage, while avoiding over-distraction. The height of the cage was 5, 6 and 7 mm in 32, 41 and 9 segments, respectively. All cages were inserted gently, using a hummer, within 1 mm of anterior vertebral body (Figs. 1c, 3). Proper cage size and position were confirmed by fluoroscopy and by its resistance to pull-out after releasing the traction. Finally, the skull traction was released to insure the absence of any possible gap at the end-plate–cage interface and to provide ideal contact surface for fusion. All patients were immobilized post-operatively with a Philadelphia collar for at least 3 months. Clinical and radiological evaluations were performed after surgery at the second day, first week, second week, and every 2 weeks till fusion. Then the patients were followed up regularly at 3-month intervals till the end of follow-up.
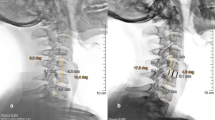
Pre-operative MRI (a) and lateral radiographs (b) of a 43-year-old male showing multilevel segmental stenosis with collapsed discs and a straight spine (0° Cobb’s angle). Immediate post-operative radiographs after 4-level stand-alone PEEK cage-assisted ACDF with 30° C2–C7 Cobb’s angle (c). Dynamic radiographs showing the absence of cage subsidence, maintained alignment and bony fusion as defined by the absence of a radiolucent gap between the graft and the end-plate, the presence of continuous bridging trabeculae between the end-plates and no more than 2 mm motion between the tips of spinous processes (*) on flexion (d) and extension (e) views
Clinical evaluation
The 10-point visual analogue scale (VAS) was used to assess neck pain and arm pain; with 0 indicating no pain and 10 points indicating the worst pain possible. Overall patient’s satisfaction was assessed according to Odom’s criteria [22] and was graded as satisfactory (excellent/good) or unsatisfactory (fair/poor) based on the improvements in patient’s clinical manifestations and the ability to regain physical activities. Dysphagia and donor site pain were considered transient when they sustained for ≤2 weeks without distressing the patient. They were considered significant when they persisted >2 weeks or when they were distressful for the patient (i.e. necessitating special intervention or intensive medications).
Radiological evaluation
Plain X-rays were taken to evaluate fusion, alignment and subsidence (Fig. 3). Fusion criteria based on continuity of the trabeculae between end-plates with the absence of lucency at the cage/end-plate interface. This was confirmed by stability on dynamic views (not more than 2 mm widening of the inter-spinous distance) or by CT in suspected fusions. Cervical alignment was measured pre-operatively, post-operatively and at 2-year follow-up by the lateral C2–C7 Cobb’s angle. Subsidence was defined ≥3 mm reduction in the fusion segmental height (FSH) at the final follow-up compared with that measured at the immediate post-operative period. The FSH was measured as the distance between the mid-points of upper and lower margins of the upper and lower vertebral bodies of each segment, respectively. Magnification differences were overcome by measuring its ratio to the body width.
Statistical analysis
The paired t test was used to detect inter-group changes of VAS scores and C2–C7 Cobb’s angle values, while ANOVA test was used to detect the intra-group changes of these parameters (Table 1). Odom’s criteria as well as the rate of cage subsidence, non-union, dysphagia and donor site pain were compared between groups using Chi-square test (Table 2). Additionally, the effects of certain variables in the study (age, sex, fusion levels, cage dimensions and patient’s compliance) were also assessed using Chi-square test.
Results
All patients completed 2-year follow-up period which was taken as an end point for result evaluation. There was no significant difference in the patient’s characteristics (P = 0.758, 0.109 and 0.905 for differences of age, sex and duration of symptoms, respectively), or in the pre-operative clinical parameters (P > 0.05) between groups. All cages were implanted successfully. The mean operative time was 98 ± 20.5 min, 122.23 ± 22.69 min and 147 ± 18.188 min (P < 0.001) in the three groups, respectively. The mean amount of bleeding was 78.2 ± 18.8 ml, 93.7 ± 21.55 ml and 123.5 ± 25.87 ml (P < 0.001) in the three groups, respectively. There were no intra-operative complications, and none of the patients experienced neurological deterioration.
There was a significant improvement (P < 0.001) in the mean VAS scores of both neck and arm pains at the second post-operative week in each group (Table 1). There were no patients with a daily demand of analgesics for radicular or axial neck pain in all groups after 1-month post-operatively. However, at 3-month follow-up, two cases had recurrent attacks of mild–moderate radicular pain after exertion, and their pain could be managed by conservative therapy. Interestingly, they were satisfied with surgery as compared to their pre-operative agonizing symptoms (intractable persistent pain). At 2-year follow-up, the improvements in VAS scores were well maintained (P > 0.05) and there were no statistically significant differences (P > 0.05) between the three groups in these scores (Table 1).
The lateral C2–C7 angle showed significant improvement (P < 0.001) in the immediate post-operative period in each group and was not changed significantly (P > 0.05) till the end of follow-up (Table 1). The obtained overall lordosis was best achieved (P < 0.001) among patients undergoing 4-level surgery and was also significant (P < 0.001) among patients undergoing 3-level surgery compared with those undergoing 2-level procedures (Table 1).
Solid fusion was obtained in 26 (92.85 %) patients. Mean time of fusion was 14.9 ± 3.2 weeks, 15.2 ± 3.74 weeks and 16.1 ± 4.02 weeks in the three groups, respectively (P = 0.537). There was no statistically significant difference (P = 0.39) between groups in the non-union rate (Table 2). Both non-united levels showed no clinical consequences.
Subsidence was encountered in seven fusion levels among five patients after 4–6 weeks following surgery with no evidence of progression beyond 2 months. Subsidence occurred in one cage in a patient of group I, three cages in two patients of group II and three cages in two patients of group III. There was no statistically significant difference (P > 0.05) between groups in the cage subsidence rate (Table 2). All subsided levels achieved solid fusion and four of these seven subsided cages were encountered at C6–C7 level (Table 3). None of the subsided levels had >50 % loss of the obtained immediate post-operative segmental disc space height. Two of the five involved patients develop the above-mentioned recurrent mild–moderate arm pain at 3-month follow-up and had no significant compression in follow-up MRI (Fig. 4).
MRI-T2 W views of a 44.5-year-old female who underwent 4-level stand-alone PEEK cage-assisted ACDF (arrows). a Pre-operative sagittal view showing stenosis at C3–C7 levels with mal-alignment. b Sagittal view at 3-month follow-up was done after C6–C7 cage subsidence and demonstrated good overall alignment and mild compression of neural elements at subsided level. c, d Axial MRI views at C6–C7 level showing the relative patency of the canal and the neural foramina at 3-month follow-up (d) as compared to the pre-operative stenosis (c) despite cage subsidence
Level C6–C7 was included in the fusion of nine cases (Table 3). Of them four showed subsidence (P = 0.003) and another one had non-union. Non-compliance was encountered in five patients (two in group I, two in group II and one in group III). Of these five patients, one developed non-union and the other three were associated with subsidence (P = 0.033) including: single-level subsidence in one case and double-level subsidence in the other two cases (Table 3). Age, sex, cage dimensions and duration of symptoms had no statistically significant effect (P > 0.05) on the subsidence rate.
Transient dysphagia occurred in five patients, while the significant one occurred in two patients without severe distress and was resolved after 4–5 weeks post-operatively. Two patients had mild transient donor- site discomfort, and none had cervical or donor site wound infections (Table 2).
All patients were satisfied after surgery and none of them required revision surgery (Table 2).
Discussion
Though it has become a routine practice to use stand-alone cages in oligo-segmental ACDF to eliminate plate and graft-related morbidity [1, 15, 16, 19], there are considerable debates for their use in multilevel ACDF procedures [2, 4, 8–10, 17–19]. Successful treatment depends on adequate decompression, restoration and maintenance of inter-vertebral disc height, realignment of the cervical curvature and achieving high fusion rate with low rate of complications [1, 7, 8, 12, 14, 16–19]. In this short-term series of multilevel cervical stenosis, PEEK cage-assisted ACDF was performed, in carefully selected patients, and additional plate fixation was not used in any patient, yet satisfactory clinical and radiological results were obtained. There were no statistically significant differences between 2-, 3-, and 4-level fusion groups in the clinical outcomes or the change of radiological parameters between immediately after surgery and the last follow-up radiographs. None of the patients exhibited major complications and none required revision surgery.
In the current series, the UVJs and PLL were preserved as decompression was achieved indirectly by disc space distraction. The posterior osteophytes, being not completely obliterating the neural foramens according to the inclusion criteria, were left for spontaneous resorption and remodelling [12, 23]. Distraction opens the vertical height and cross-sectional area of the foramina, while realignment increases its anteroposterior diameter [1, 12, 23]. Coupling this with the decompression achieved by removal of the disc, stretching of PLL and straightening of ligamentum flavum, the pinching on neural elements could be eliminated even in the presence of moderate size osteophytes (Fig. 2). There was a significant improvement in the VAS of both the arm pain (as an indicator of adequate decompression) and neck pain (as an indicator of stability and neck muscle balance). All patients had satisfactory outcomes as defined by Odom’s criteria. This supports the findings of Shen et al. [24] who found high satisfactory results after ACFD with statistically insignificant clinical differences in the presence or absence of direct UVJ decompression. Interestingly, all subsided levels in the present study had caught fusion before the progression of their subsidence. So they preserved some foraminal patency and alignment compared with their pre-operative collapsed disc status; hence, no noticeable subjective clinical consequences were observed except in two cases. The two symptomatic cases suffered from recurrent attacks of arm pain with exertion, but had no significant compression in follow-up MRI and were successfully managed by periodic conservative therapy. Abolishing of the pathological segmental movement and the better post-operative alignment in these two cases may explain the less-severe symptoms in them. Schmieder et al. [14] also reported that the height of the foramina was well maintained among the subsided cases and that symptomatic improvement is not impaired by the presence of subsidence but may, on the other hand, help fusion.
Previous studies [9, 13, 14, 17] reported high rates (up to 55.55 % as encountered by levels) of cage subsidence after stand-alone cage constructs in single- and double-level fusions which are alarming for their use in multilevel ACDF. In the present study, only seven (8.54 %) of the 82 inserted PEEK cages had subsided with no statistically significant differences between groups (P = 0.367). This compares with the 8.89 % subsidence rate, among 15 patients who underwent 3-level stand-alone cage-assisted ACDF, in Zou et al. series [18]. Moreover, Yang et al. [10] did not report any significant subsidence among 23 patients who underwent 3- and 4-level stand-alone cages, in their study. The latter two studies used modified stand-alone PEEK cage designs, including self-locked toothed cage designs in the former and cages with anchored spacer in the latter. However, besides the extra-costs of these designs, there may be difficulty in targeting the screw due to angulations, and these designs may compromise the bone stock by hammering or screwing through the end-plate.
Bartels et al. [15] concluded that the incidence of cage subsidence was significantly higher for C6–C7 fusion level than any other fusion levels. In the present study, four (57.14 %) of the seven subsided cages occurred at this level (P = 0.003). This can be attributed to the transitional nature of this level. So, special caution by plate augmentation should be paid for fusions extending to this level.
Bone quality and bone stock are crucial for durability of cage-assisted ACDF, and previous studies emphasized the biomechanical importance of the anterior vertebral osteophyte in providing mechanical support to the inter-body cage [15, 16, 19, 26]. In the present study, all proven osteoprotic patients or at-risk patients were excluded and careful attention was paid for preservation of dense cortical bone of osteophytes. Additionally, all cages were carefully placed within 1 mm from anterior vertebral margin, as the distance between the cage and the anterior vertebral rim was reported to correlate with the incidence of subsidence [15, 16, 19]. Furthermore, the UVJs were preserved, as they play a central role for segmental cervical stability, with the posterior aspect of the UVJ affording majority of stability [20, 21].
End-plate preparation has to provide good fusion bed, while maintaining the mechanical integrity of the bony part of the end-plate to prevent cage subsidence [12, 15, 16, 19, 25]. In this series, good fusion bed was achieved by sufficient curettage of the central area of the cartilaginous end-plate, good compression at cage/end-plate interface and iliac graft over-packing. However, the peripheral part of the end-plate, the common site for cage subsidence, was managed by fine abrasions to preserve good support to the cage. End-plate over-preparation can be suspected when subsidence appears in the peri-operative radiographs which had occurred in none of the patients.
Intra-operative over-distraction and cage over-sizing were found clinically and biomechanically associated with higher subsidence tendency [9, 15, 19, 26]. Over-distraction was successfully avoided in the present work by the followings: (1) Controlled skull traction that provided symmetrical distribution of distraction over all cervical levels and allowed precise cage size measurement. No Caspar distractor was used in the present study to avoid defects in the vertebral bodies and instability caused by over-stretching of the ligaments. (2) Preserving the PLL which is crucial for effective distraction (Fig. 1a–c), as it acts as a fulcrum during distraction–realignment manoeuver to achieve opening of the anterior column and closing the posterior column [5, 12]. (3) The microscope ensures good visualization, while avoiding unnecessary extensive release and removal of the end-plate, which may occur when decompression is done without microscope. This was particularly helpful when small central PLL windows were created to extract small sequestrated fragments. (4) The serial proximal-to-distal insertion of cages. The second disc space had never been attacked (absolutely), except after insertion of the first (proximal) one definitely. If not, one often finds that the second cage requires excessive persuasion to enter the disc space.
Unrestricted neck movements were proven, biomechanically, to cause failure in different cervical cage designs [27]. This may be a predisposing factor for cage subsidence in some studies that did not follow a definite postoperative bracing protocol [14, 15]. All patients of the present study were sharply instructed to wear rigid cervical collar for a minimum of 3 months after surgery, which correspond to the maximum time reported in the literature for the end point of progression of cage subsidence [9]. Three of the five non-compliant cases in this study were participated in vigorous activities and experienced cage subsidence and another one had non-union.
The low subsidence rates achieved in this study is strongly contradicted to those of Gercek et al. [13], who had the worst results in the literature (i.e. 62.5 % of their patients). However, they used metal cages which have different elasticity with bone. Additionally, their small number of patients (eight cases only), short period of immobilization (4–6 weeks only), big cage sizing (7–10 mm) and the differences in: selection criteria, decompression technique, evaluation methods and their variable cage positioning, make comparison impractical.
High fusion rates (≥90 %) have been reported after cage-assisted ACDF [1, 2, 9, 10, 14, 16, 18]. However, the fusion rate was reported to decline as the number of levels increases even when anterior cervical locked plate was used [7, 19, 28]. Non-union rates as high as 47 % have been reported in the literature for 3-and 4-level discectomies with plate fixation [28]. Contrary to these results, the present study found 92.86 % fusion rates in a mean time of 15.817 ± 3.474 weeks with insignificant fusion rates after 2-, 3- and 4-level stand-alone ACDF. Non-union was found at two (2.44 %) levels in two (7.14 %) asymptomatic patients at C3–C4 and C5–C6 levels in group II and III, respectively. This satisfactory fusion results in all groups can be explained by the success in adjustment of the biological and mechanical environments, biologically, by the absence of predisposing factors (e.g. osteoprosis, smoking, infection), the use of iliac crest autograft, the use of the biologically biocompatible PEEK cages and the above-mentioned optimal fusion bed preparation and mechanically, by the presence of titanium spikes and retention teeth of PEEK cage, proper disc space distraction, preservation of some natural supporting structures and the prolonged external immobilization.
It has been documented that plate augmentation has the potential to lower rate of pseudoarthrosis during ACDF procedures [4, 7–9, 17]. Song et al. [17] reported non-fusion in 2.5 % of their plated subjects compared with 21.1 % in the cage-alone group for single- and double-level ACDF. Wang et al. [4] reported 18 and 37 % incidence of non-union in plated versus non-plated multilevel ACDF, respectively. On the other hand, Cho et al. [2] and Yang et al. [10] found equivalent fusion outcomes among plated and non-plated multilevel PEEK-cage-assisted ACDF groups. This controversy in the literature can be attributed to the differences in: selection criteria, surgical technique, cage/graft characteristics, criteria used for results evaluation, patient compliance and the length of follow-up. In the current series, PEEK cages alone were successfully used, and the results were comparable to those of another series [8] in which plate augmentation was used for multilevel PEEK cage-assisted ACDF. The latter study included a series of 34 patients who underwent 3- and 4-level fusions with 100 % fusion rate in a mean time of 13.7 ± 5.1 weeks. Their complications included three cases of respiratory difficulty, four cases of at least 3-month of dysphagia and one case of 6-week hoarseness. So, the present series carries the advantage of the relative ease of surgery, and the success in avoidance of plate-related cost and morbidity.
A neutral sagittal vertical axis allows pain-free neck movement with reduction in the muscular effort necessary to maintain the upright posture [6, 14, 29]. The cervical sagittal balance, which is normally 28° in average, is usually compromised in the setting of multilevel cervical spondylosis. The cervical alignment showed a statistically significant improvement in the immediate post-operative period in all groups of the present series. Interestingly, the C2–C7 angle was not significantly changed between immediately after surgery and last follow-up radiographs in each group. The low incidence of subsidence in the present series can explain the success in maintaining the sagittal profile till the end of follow-up. Cage subsidence resulted in some straightening of cervical lordosis in all subsided cases with no major subjective clinical consequences. This is in agreement with other authors who reported radiological subsidence without leading to poorer clinical outcome in short-term follow-up [9, 14–16]. Schmieder et al. [14] stated that the occurrence of kyphosis among the subsided cases was either rare or did not result in notable clinical differences. However, the reconstruction of cervical lordosis may be crucial for long-term good clinical outcome [2, 4, 29]. In the current study, 3- and 4-level surgery had allowed significant correction of overall lordosis compared to 2-level procedure, as this correction is hardly possible by bi-segmental procedures alone.
Song et al. [6] stated that front-back surgery is effective in reducing cage subsidence rate and its subsequent mal-alignment, but they focused on management of kyphotic segments. Conversely, in biologically stable degenerative spine with moderate mal-alignment (straight spine), when extensive decompression is not indicated, the addition of a second approach seems over-treatment, especially in the light that posterior approaches are fraught with troublesome complications (axial neck pain, and C5 root problems). In the present series, the preserved UVJs, PLL and remaining anterolateral structures aid in maintaining some biological stiffness and inherited stability of the involved segments.
Dysphagia is a concern after anterior cervical plating due to prolonged intra-operative oesophageal retraction and/or due to the local post-operative plate prominence, especially with long plates in conjunction with multilevel ACDF [2, 7, 8, 10, 11]. In their systemic review, including seven different studies evaluating post-ACDF dysphagia, Cho et al. [11] found up to 71, 50.2 and 14 % incidence of dysphagia at 2 weeks, 1 month and 1 year, respectively. The use of inter-vertebral cervical cages, which are settled below the vertebral surface, the intermittent retraction technique, the intra-operative administration of intravenous methylprednisolone and the relatively time-saving (with neither plates nor extensive decompression) procedure could reduce these problems. In the current study, five patients (17.86 %) had transient dysphagia (<2 weeks), and only other two patients (7.14 %) had significant dysphagia (>2 weeks, but not distressful) that recovered totally within 3–4 weeks after surgery.
Donor site morbidity with 50 % incidence of early ambulatory difficulty and 26 % incidence of chronic persistent pain, with long-term functional impairment, was reported after harvesting autogenous tri-cortical iliac grafts for single-level ACDF procedures [30]. This is prone to be higher in traditional multilevel settings due to big purchase of bone mass with extensive dissection. In the present study, as in some other studies [1, 7, 8, 13], the cervical cage was filled with cancellous autologous iliac crest graft harvested with a corer through a percutaneous stab incision. Therefore, donor site morbidity was minimized with a tolerable occasional pain occurred in only two patients (7.14 %).
Regarding the motion-preserving alternatives, multilevel cervical discectomy is a definite contraindication for total disc replacement [31], while the mal-aligned cervical spine is not a good candidate for non-instrumented posterior decompression techniques, as post-laminectomy instability and progressive kyphosis are major concerns. Additionally, fusion is the gold standard for abolishing pain of symptomatic degenerative mal-aligned spine. All of our patients had pre-operative axial neck pain and radiological evidence of spondylosis in a mal-aligned cervical spine.
Our preliminary experience with the indirect decompression technique and stand-alone PEEK cages for contiguous multilevel ACDF, outcomes have been encouraging, However, special caution should be paid for fusions extended to C6–C7 level and when the patient is hesitated, pre-operatively, in accepting the post-operative protocol and bracing. The prospective nature of this study enables the author to limit his indications and to improve his technique. The indications, though limited, can be extremely useful in some patients to avoid unnecessary instrumentation with the hazards and the expenses of the additional plate fixation. Another shortcoming is the short period of follow-up which is insufficient for commenting on adjacent segment changes with its possible effect on sagittal alignment and development of new pain. A long-term follow-up study, with a larger number of patients and control groups including plated ACDF and/or direct decompression technique, should be performed to further investigate the efficacy of stand-alone cages for the treatment of 3- and 4-level CDS.
Conclusion
With proper patient selection, meticulous surgical technique and strict post-operative cervical bracing, the less-invasive indirect anterior cervical decompression technique augmented with stand-alone PEEK cage-assisted ACDF is an efficient and safe method for the treatment of multilevel CDS.
References
Cho DY, Liau WR, Lee WY, Liu JT, Chiu CL, Sheu PC (2002) Preliminary experience using a polyetheretherketone (PEEK) cage in the treatment of cervical disc disease. Neurosurgery 51(6):1343–1349
Cho DY, Lee WY, Sheu PC (2004) Treatment of multilevel cervical fusion with cages. Surg Neurol 62:378–385
Chou Y, Chen DC, Hsieh WA et al (2008) Efficacy of anterior cervical fusion: comparison of titanium cages, polyetheretherketone (PEEK) cages and autogenous bone grafts. J Clin Neurosci 15(11):1240–1245
Wang JC, McDonough PW, Endow KK, Delamater RB (2001) Increased fusion rates with cervical plating for three-level anterior cervical discectomy and fusion. Spine 26:643–647
Stewart TJ, Schlenk RP, Benzel EC (2007) Multiple level discectomy and fusion. Neurosurgery 60:S143–S148
Song K, Johnson J, Choi B (2010) Anterior fusion alone compared with combined anterior and posterior fusion for the treatment of degenerative cervical kyphosis. J Bone Joint Surg 92-B:1548–1552
Song KJ, Taghavi CE, Hsu MS, Lee KB, Kim GH, Song JH (2010) Plate augmentation in anterior cervical discectomy and fusion with cage for degenerative cervical spinal disorders. Eur Spine J 19(10):1677–1683
Song K-J, Yoon S-J, Lee K-B (2012) Three- and four-level anterior cervical discectomy and fusion with a PEEK cage and plate construct. Eur Spine J 21(12):2492–2497
Fujibayashi S, Neo M, Nakamura T (2008) Stand-alone interbody cage versus anterior cervical plate for treatment of cervical disc herniation: sequential changes in cage subsidence. J Clin Neurosci 5:1017–1022
Yang L, Gu Y, Liang L, Gao R, Shi S, Shi J, Yuan W (2012) Stand-alone anchored spacer versus anterior plate for multilevel anterior cervical discectomy and fusion. Orthopedics 35(10):1503–1510
Cho SK, Lu Y, Lee D-H (2013) Dysphagia following anterior cervical spinal surgery. A systematic review. Bone Joint J 95-B:868–873
An HS, Evanich CJ, Nowicki BH, Haughton VM (1993) Ideal thickness of Smith-Robinson graft for anterior cervical fusion. Spine 18:2043–2047
Gercek E, Arlet V, Delisle J, Marchesi D (2003) Subsidence of stand-alone cervical cages in anterior interbody fusion: warning. Eur Spine J 12(5):513–516
Schmieder K, Wolzik-Grossmann M, Pechlivanis I, Engelhardt M, Scholz M, Harders A (2006) Subsidence of the wing titanium cage after anterior cervical interbody fusion: 2-year follow-up study. J Neurosurg Spine 4(6):447–453
Bartels RH, Donk RD, Feuth T (2006) Subsidence of stand-alone cervical carbon fiber cages. Neurosurgery 58(3):502–508
Barsa P, Suchomel P (2007) Factors affecting sagittal malalignment due to cage subsidence in standalone cage assisted anterior cervical fusion. Eur Spine J16(9):1395–1400
Song KJ, Taghavi C, Lee KB, Song JH, Eun JP (2009) The efficacy of plate construct augmentation versus cage alone in anterior cervical fusion. Spine 34(26):2886–2892
Zhou J, Li X, Dong J, Zhou X, Fang T, Lin H, Ma Y (2011) Three-level anterior cervical discectomy and fusion with self-locking stand-alone polyetheretherketone cages. J Clin Neurosci 18(11):1505–1509
Yang JJ, Yu CH, Chang BS, Yeom JS, Lee JH, Lee CK (2011) Subsidence and nonunion after anterior cervical interbody fusion using a standalone polyetheretherketone (PEEK) cage. Clin Orthop Surg 3(1):16–23
Kotani Y, McNulty P, Abumi K, Cunningham B, Kaneda K, McAfee P (1998) The role of anteromedial foraminotomy and the uncovertebral joints in the stability of the cervical spine: a biomechanical study. Spine 23:1559–1565
Chen TY, Crawford NR, Sonntag VKH, Dickman C (2001) Biomechanical effects of progressive anterior cervical decompression. Spine 26:6–13
Odom GL, Finney W, Woodhall B (1958) Cervical disk lesions. J Am Med Assoc 166:23–28
Bayley JC, Yoo JU, Kruger DM, Schlegel J (1995) The role of distraction in improving the space available for the cord in cervical spondylosis. Spine 20:771–775
Shen FH, Samartzis D, Khanna N, Goldberg EJ, An HS (2004) Comparison of clinical and radiographic outcome in instrumented anterior cervical discectomy and fusion with or without direct uncovertebral joint decompression. Spine J 4(6):629–635
Lim TH, Kwon H, Jeon CH, Kim JG, Sokolowski M, Natarajan R, An HS, Andersson GB (2001) Effect of endplate conditions and bone mineral density on the compressive strength of the graft-endplate interface in anterior cervical spine fusion. Spine 26:951–956
Truumees E, Demetropoulos CK, Yang KH, Herkowitz HN (2002) Effects of disc distractive forces on graft compression in an anterior cervical discectomy model. Spine 27:2441–2445
Wilke HJ, Kettler A, Goetz C, Claes L (2000) Subsidence resulting from simulated postoperative neck movements: an in vitro investigation with a new cervical fusion cage. Spine 25:2762–2770
Bolesta MJ, Rechtine GR, Chrin AM (2000) Three- and four-level anterior cervical discectomy and fusion with plate fixation: a prospective study. Spine 25(16):2040–2046
Harrison DE, Harrison DD, Janik TJ, William Jones E, Cailliet R, Normand M (2001) Comparison of axial and flexural stresses in lordosis and three buckled configurations of the cervical spine. J Clin Biomech 16(4):276–284
Silber JS, Anderson DG, Daffner SD, Brislin BT, Leland JM, Hilibrand AS, Vaccaro AR, Albert TJ (2003) Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine 28(2):134–139
Auerbach JD, Jones KJ, Fras CI, Balderston JR, Rushton SA, Chin KR (2008) The prevalence of indications and contraindications to cervical total disc replacement. Spine J 8(5):711–716
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
El-Tantawy, A. Is it possible to eliminate the plate-related problems and still achieve satisfactory outcome after multilevel anterior cervical discectomy?. Eur J Orthop Surg Traumatol 25 (Suppl 1), 135–145 (2015). https://doi.org/10.1007/s00590-015-1611-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-015-1611-8