Abstract
Background
It is a general belief among hip surgeons that minimally invasive surgical (MIS) approach for implantation of a total hip arthroplasty (THA) allows an improved and faster postoperative rehabilitation because of reduced muscle and soft-tissue damage, less postoperative pain and blood loss, and shorter hospital stay compared with conventional approaches. In the published relative literature though, there are controversial reports and debates on this matter. To our knowledge, there is no study on the medium-term functional results comparing MIS and traditional approaches for total hip replacement. The purpose of this prospective comparative controlled study was to compare MIS with conventional approach, on terms of pain, blood loss, and functional recovery over a follow-up period of 4 years.
Methods
In a total of 90 consecutive randomly selected adult patients, who suffered from unilateral primary hip osteoarthritis, a cementless Zweymüller-Plus THA (SL-Plus stem, Bicon screw socket) was implanted by a single senior orthopedic hip surgeon in one institution in the same period. Forty-five patients (group A) were operated using an MIS anterolateral, short incision, muscle-sparing approach and 45 (group B) with a conventional (anterolateral modified Watson-Jones) approach under partial detachment of gluteus medius and minimus. Anthropometric data, blood loss, short-form 36 questionnaire, visual analog scale pain score, and walking endurance were included in the analysis. Approach-related surgical complications (trochanter major fracture, Bicon malposition) were recorded. Data were collected postoperatively and at 4-year follow-up.
Results
Two patients of group A and eight patients of group B were excluded from the final analysis. Thus, 80 patients were eligible for the final evaluation 4 years postoperatively. Postoperative pain score was less in the MIS group. However, no differences in perioperative blood loss, functional outcome, and walking endurance were shown between groups. No difference in Bicon cup implantation angle was measured in postoperative roentgenograms between group A and B patients, no intraoperative trochanter fracture occurred in any patient of both groups.
Conclusions
The present prospective randomized study revealed no significant mid-term clinical and functional benefit for patients who underwent a THA through an MIS in comparison with those who were managed with a conventional open approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Minimally invasive surgery (MIS) techniques have gained an increased interest among orthopedic surgeons in the last decade. In the field of total hip arthroplasty (THA), a debate has started worldwide in the recent years regarding the possible clinical benefits of minimal invasive approaches as compared with the conventional ones. No clear definition exists for what constitutes MIS THA, but there is a relative consensus that THAs performed with any incision <10 cm can be included [1]. Others define it as a technique that causes no damage to the soft tissue and muscles [2].
The rationale for MIS is a minimized tissue dissection, resulting in reduced blood loss, pain, hospital stay, and faster rehabilitation [3]. Opponents believe that MIS leads to increased iatrogenic nerve injury, prosthesis malposition, and increased revision rate, because of the limited field of vision during the surgery [4, 5]. Even randomized trials showed conflicting results [6–9].
The short-term (up to 12 months) impact of intraoperative occurring muscle damage on early functional recovery and walking ability was previously reported [10, 11], but to our knowledge, medium- and long-term functional results have not been reported.
To contribute to a better understanding of the effects of MIS THA on clinical and other parameters, we conducted a prospective randomized controlled trial, comparing results of one cementless THA (Zweymüller-Plus, Smith & Nephew, Baar, Switzerland) implanted via either a minimal anterolateral approach or via the conventional modified Watson-Jones approach. Our main goal was to evaluate any short- and medium-term clinical benefits or drawbacks of using an MIS approach to implant a cementless THA.
The hypothesis in this study was that blood loss and pain level were less in patients operated with MIS approach (group A), while self-assessment short-form 36 (SF-36) scores and walking endurance were higher than in the patients operated with conventional (group B) technique.
Patients and methods
Institutional review board approval (IRB) was obtained, and all patients provided informed consent. Inclusion criteria were unilateral primary hip osteoarthritis and a body mass index of <30 kg/m2. Exclusion criteria were previous surgery, previous arthroplasties in other joints in the lower extremities, rheumatoid arthritis, developmental hip dysplasia and dislocation, and decreased mobility due to significant stiffness of the hip joint or non-joint-related factors (e.g., neurologic disease).
Patients were randomly assigned to receive the same cementless Zweymüller- Plus THA using an MIS approach (group A, 45 patients) or a conventional open technique (group B, 45 patients). Hips were assigned to group A or B by a computer-generated randomization schedule. No power analysis was carried out in this clinical study.
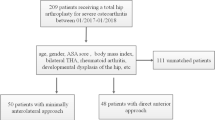
From the initial 90 patients who fulfilled the inclusion criteria and were initially enrolled in this study, 10 operated patients (two in group A and eight in group B) were lost to follow-up due to reasons non-related to the operation (e.g., unavailable or change in residence) and thus were excluded from the final evaluation. The remaining 80 patients (43 in group A and 37 in group B) were eligible and available for the final complete analysis 4 years postoperatively (Fig. 1).
We used the visual analog scale (VAS scale 0–10) for pain to assess pain intensity preoperatively, 2 weeks and 4 years postoperatively. The SF-36 self-assessment questionnaire for functional outcome was also evaluated preoperatively and 4 years postoperatively (Tables 1, 2). Hematocrit was measured on admission and discharge. The indication for blood transfusion in elective surgery in the authors’ institution is hematocrit <30 %. The baseline characteristics of all 80 patients are shown in Table 1.
All surgeries were performed by an experienced orthopedic surgeon (P.K.), who has performed more than 4,000 THAs. In all 80 cases, the same standard type of implant was used (cementless Zweymüller-Plus THA: a Bicon double-conus threaded cup with an SL-Plus tapered straight stem). The articulating pairings were ceramic-on-ceramic with a 28-mm ceramic ball head.
Surgical approaches
Minimally invasive approach
In group A, the patient was positioned on the operating table in the supine position with both lower limbs draped in a sterile fashion. An oblique skin incision measuring 8–10 cm was made, extending distally from the anterior superior iliac spine and ending at the flare of the greater trochanter. After division of the subcutaneous tissue and fascia, the interval between the tensor fasciae latae and the gluteus medius was opened bluntly with the insertion of the index finger. The vessels crossing this intramuscular space were ligated. No muscle (glutei medius and minimus and tensor fascia latae) was split or detached. The hip capsule was divided in an H-shaped fashion and preserved. The acetabulum was prepared in a traditional fashion with the use of standard reamers. For preparation of the femur, the involved lower limb was placed in external rotation under the contralateral—already draped for this maneuver—lower limb. In this position, an elevating retractor was placed posterior to the greater trochanter to lever the femur out of the wound. Further preparation of the femur was similar to that in group B and was performed with the use of specific MIS instruments. After insertion of implants (Bicon Cup and SL-stem) and control of impingement and stability, the hip capsule was sutured and a redon drainage was placed on the hip capsule.
Conventional approach
In group B, the patient was placed in the supine position with only the involved lower limb draped. A lateral skin incision approximately 16–18 cm in length was made, extending distally from the anterior superior iliac spine and ending 5 cm distally from the greater trochanter tip. Using the modified Watson-Jones anterolateral approach [12], the fasciae latae was longitudinally split and gently retracted. The gluteus minimus insertion was completely released at the trochanter major insertion. The distal third of the insertion of gluteus medius at the greater trochanter was partially released to allow adduction and external rotation for better orientation and hip dislocation and subsequently SL-Plus stem implantation. The hip capsule was subtotally resected. For preparation of the proximal part of the femur, the involved lower limb was positioned in external rotation over the contralateral not draped lower limb. After implant (Bicon cup and SL-stem) insertion and control of impingement and stability the hip, a redon drainage was intra-articularly placed.
Postoperative course
The postoperative course was the same for both groups. Mobilization started on postoperative day 1 with the use of two forearm crutches with 4-point walking. The use of two crutches was recommended for 3 weeks postoperatively. Patients were allowed to discontinue the crutches for full weight bearing as tolerated, depending on the individual level of cooperation, mobilization status, and pain intensity. All patients were discharged after a minimum hospital stay of 3 days (range 3–5 days).
On plain pelvis roentgenograms, the insertion angle of the Bicon cup (angle formed from the biischial line and the frontal inclination of the cup) was measured.
The degree of periarticular ossification according to Brooker classification was postoperatively recorded on the AP plain roentgenograms of the pelvis.
Statistical analysis
Intention-to-treat analysis was used for all clinical outcome variables and was performed by an independent external statistician (P.F.). Data were analyzed with Stata version 11.2 software (StataCorp LP, College Station, Texas). Univariate analysis of continuous data was performed with the parametric t test or the nonparametric Mann–Whitney U test. Because of the relatively small sample size, continuous variables were tested on normality using the Shapiro–Wilk test. When the p value was <0.05, data were assumed to not be normally distributed, and a nonparametric test was used. Univariate statistical tests are reported as parametric unless indicated.
Treatment comparison for the primary outcomes of interest was based on linear mixed models. Linear mixed models are a generalization of ordinary least-squares linear regression models. Three-level variance component models were developed. The model was tested against the more parsimonious 2-level models. Fixed effects in the saturated model included sex, age, group, and preoperative VAS. For the final model, fixed effects were eliminated based on their effect on study group and operated side.
Reliability of the repeated measurements was determined by the model-based intra-class correlation coefficient (ICC).
Results
Baseline (preoperative) demographic and preoperative variables are presented in Table 1.
One main difference was spotted between the two groups of patients that were finally evaluated: The percentage of women in group B (conventional) is higher than in group A (79 and 70 %, respectively).
On discharge, postoperative hematocrit was on average lower in group B patients (conventional approach), but the difference was not statistically significant (p = 0.08) ( Table 2).
There was also no statistical significant difference in the amount of blood units which were transfused in the two groups (p = 0.67).
Visual analog scale scores improved significantly postoperatively in both groups. At 2 weeks postoperatively, patients with MIS (group A) reported significantly (p = 0.013) lower postoperative pain score (VAS = 0.97 ± 1.4), in comparison with patients of group B (conventional) (VAS = 2 ± 2.17), whereas there was no statistical significant difference at the final follow-up evaluation (Table 2).
Bicon cup inclination angle did not differ significantly (p = 0.517) between the two groups (average angle = 47.2° ± 3.6° for group A and 46.3° ± 2.3° for group B, respectively).
At the 4-year-follow-up evaluation, there were no significant differences in terms of the SF-36 component scores and walking capability between the two groups (Table 2).
Complications
There were no intraoperative complications.
Malpositioning of the components was not found on the postoperative radiographs in any group. No patient had any dislocation of the hip postoperatively.
No postoperative limb length discrepancy exceeded 1 cm, no Trendelenburg was shown in any patient in both groups.
There was no statistical significant difference (p = 0.241) between the Brooker grades of postoperatively detected heterotopic ossification.
Discussion
In this study, we hypothesized that patients operated with MIS approach would have less blood loss perioperatively and less pain postoperatively. The theoretically less invasive surgery (MIS) should be advantageous compared with conventional technique and thus be associated with higher SF-36 scores and walking endurance at the medium-term follow-up evaluation.
Our results did not completely justify these hypotheses. MIS approach did not have any advantage in the immediate postoperative period for the patients in terms of blood loss, except for pain intensity which according to VAS was significantly lower 2 weeks postoperatively in the MIS operated patients. Moreover, there was no significant medium-term advantage in favor of MIS patients in terms of SF-36 scores and walking endurance.
Our study has certain limitations. First, we did not mask the two different incisions. Therefore, patients and investigators were not blinded, and bias could be a result of this. The second limitation is the relatively small size of the two groups, which may explain the inability to identify any significant differences between the two groups. The third limitation is the number of patients (10) who were lost to follow-up. This may have affected our results. Finally, the conventional surgical approach for THA we used was a maximum tissue-preserving technique and may not differ significantly from what other surgeons’ regard as a minimally invasive approach. This fact may be a reason why no major differences were found between the two groups.
The relative literature regarding benefits of MIS hip techniques for THA is controversial.
There are comparative studies that disclose no difference between MIS and standard techniques [7–9, 13, 14]. A recent double-blind randomized controlled trial [15] compared minimal versus classic technique in THA performed either via posterolateral or anterolateral approach. The conclusion was that minimal invasive approach in THA did not show a clinically relevant superior outcome in the first postoperative year. Moreover, the perioperative complication rate was rather high—though not statistically significant—in the (anterolateral) MIS group.
Ogonda et al. [9] have also shown in a prospective randomized double-blinded study of 219 total hip implantations via posterior approach, no difference in pain or analgesic consumption during the first postoperative week. DiGioia et al. [16] also found no difference between a minimally invasive and a standard posterior approach in 66 patients in terms of postoperative pain levels. Lawlor et al. [17] have shown in a large prospective study no difference in functional outcome between a minimally invasive and a normal posterior approach. Cheng et al. [5] did not observe differences for the Harris hip score in a systemic review including published trials between 1996 and 2008. In a meta-analysis including all randomized and non-randomized controlled trials, Smith et al. [18] found lower but not clinically relevant pain scores between minimally invasive and conventional exposure for THA. Our results are consistent to the above-mentioned studies since no clear advantage was shown in favor of minimal anterolateral approach in terms of postoperative recovery and functional outcome. We observed lower average short-term postoperative VAS scores in the MIS group, and this seems to be the only advantage of MIS approach for THA replacement in our study.
On the other hand, some studies in the literature have demonstrated reduced perioperative blood loss and decreased postoperative pain following implantation with MIS techniques compared with standard open techniques [6, 19–22]. In a prospective study [21], 51 patients (52 hips) were randomly allocated to a classical lateral or a minimally invasive approach (modification of the Hardinge approach). Minimally invasive THA led to shorter length of surgery, slightly better WOMAC and HHS scores at discharge, quicker recovery, and at the 3-month examination, myoglobin-rise was slightly less. The positioning of the prosthesis was good in both groups. In our series, there was no statistically significant difference in perioperative blood loss between the two groups, although a marginally less blood loss was shown in the patients who were operated with MIS approach. However, we believe that in a cementless THA, the main source of blood loss is the bone (femur and acetabulum), and this seems to be the theoretical explanation for not finding significant differences in blood loss between Groups.
Goebel et al. [22] investigated 100 patients with a minimal-incision anterior approach and 100 patients with a transgluteal lateral approach. They concluded that the implantation of a hip prosthesis through a minimal-incision anterior approach is successful in reducing postoperative pain and consumption of pain medication. Time to recovery and length of hospital stay are also influenced positively. Another recent comparative study [23] between MIS anterior approach and standard lateral approach for THA disclosed similar results. Patients operated via MIS approach had less pain during movement, limping, better Harris hip score and satisfaction after 6 weeks, which remained after 12 weeks and 1 year, but not after 2 years [23].
Dorr et al. [24] found in a prospective randomized study with 60 patients significantly less pain for the group with a 10-cm-long incision within the first 2 days compared with the group with a 20-cm-long incision. A minimally invasive lateral approach was compared in another study [25] to a normal lateral approach, in which more muscle was detached, six and 12 weeks postoperatively. The Harris hip score showed significantly better values for the MIS approach during follow-up although actual pain levels were not assessed in this study [25].
All these studies focus on the acute postoperative period, and none of them manages to prove long-term superiority of MIS techniques in terms of pain and functional recovery. The only study that reports medium-term data are a recent randomized, prospective study of 75 patients comparing the anterolateral minimally invasive (MIS) and the conventional lateral approach for THA [26]. Similar to our results, this study [26] concludes that the only advantages of the MIS approach are the smaller skin incision and possible faster rehabilitation in the first 6 weeks after surgery, and no significant long-term advantage is justified.
Another matter which is often discussed in the relevant literature is the increased rates of complications encountered after MIS approaches. A meta-analysis by Smith et al. [18] showed that minimally invasive THA is associated with a significantly increased risk of transient lateral femoral cutaneous nerve palsy (p = 0.006) with no significantly better outcome. A recent study [27] comparing minimally invasive direct anterior approach and conventional posterolateral approach showed higher early complication rate in the anterior approach group and no improvement in functional outcome compared to the posterolateral approach.
Another meta-analysis focusing on radiological and complications outcomes concluded that posterior MITHA seems to be a safe surgical procedure, without the increased risk of postoperative complication rates and component malposition rates [28]. On the other hand, the current data were not enough to reach a positive conclusion that lateral and anterolateral MIS approaches will result in increased risks of adverse effects and complications at the prosthesis site [28]. In our study, there was no difference between the two groups in terms of intraoperative and postoperative complications, cup inclination angle, and Brooker Grade of heterotopic ossification.
Conclusion
The findings of our study prove that MIS anterolateral approach for cementless THA is associated with less postoperative pain and that was the only hypothesis of our study which was finally justified. No other advantages compared to the traditional anterolateral Watson-Jones approach were recorded, in terms of blood loss, recovery and walking endurance. MIS approach is equally safe and efficient as the traditional one.
References
Woolson ST, Mow CS, Syquia JF, Lannin JV, Schurman DJ (2004) Comparison of primary total hip replacements performed with a standard incision or a mini-incision. J Bone Joint Surg Am 86(7):1353–1358
Goldstein WM, Branson JJ, Berland KA, Gordon AC (2003) Minimal-incision total hip arthroplasty. J Bone Joint Surg Am 85(Suppl 4):33–38
Howell JR, Garbuz DS, Duncan CP (2004) Minimally invasive hip replacement: rationale, applied anatomy, and instrumentation. Orthop Clin North Am 35:107–118
Berry DJ, Berger RA, Callaghan JJ, Dorr LD, Duwelius PJ et al (2003) Minimally invasive total hip arthroplasty. Development, early results, and a critical analysis. J Bone Joint Surg Am 85-A(11):2235–2246
Cheng T, Feng JG, Liu T, Zhang XL (2009) Minimally invasive total hip arthroplasty: a systematic review. Int Orthop 33:1473–1481
Chimento GF, Pavone V, Sharrock N, Kahn B, Cahill J, Sculco TP (2005) Minimally invasive total hip arthroplasty: a prospective randomized study. J Arthroplasty 20:139–144
Bennett D, Ogonda L, Elliot D, Humphreys L, Lawlor M, Beverland D (2007) Comparison of immediate postoperative walking ability in patients receiving minimally invasive and standard incision hip arthroplasty: a prospective blinded study. J Arthroplasty 22:490–495
Kim YH (2006) Comparison of primary total hip arthroplasties performed with a minimally invasive technique or a standard technique: a prospective and randomized study. J Arthroplasty 21:1092–1098
Ogonda L, Wilson R, Archbold P, Lawlor M, Humphreys P, O’Brien S, Beverland D (2005) A minimal-incision technique in total hip arthroplasty does not improve early postoperative outcomes: a prospective, randomized, controlled trial. J Bone Joint Surg Am 87:701–710
Pospischill M, Kranzl A, Attwenger B, Knahr K (2010) Minimally invasive compared with traditional transgluteal approach for total hip arthroplasty. A comparative gait analysis. J Bone Joint Surg Am 92:328–337
Müller M, Tohtz S, Springer I, Dewey M, Perka C (2011) Randomized controlled trial of abductor muscle damage in relation to the surgical approach for primary total hip replacement: minimally invasive anterolateral versus modified direct lateral approach. Arch Orthop Trauma Surg 131:179–189
Bertin KC, Röttinger H (2004) Anterolateral mini-incision hip replacement surgery. A modified Watson-Jones approach. Clin Orthop 429:248–255
Nakamura S, Matsuda K, Arai N, Wakimoto N, Matsushita T (2004) Mini-incision posterior approach for total hip arthroplasty. Int Orthop 28:214–217
Sculco TP (2004) Minimally invasive total hip arthroplasty: in the affirmative. J Arthroplasty 19(4 suppl 1):78–80
Goosen JH, Kollen BJ, Castelein RM, Kuipers BM, Verheyen CC (2011) Minimally invasive versus classic procedures in total hip arthroplasty: a double-blind randomized controlled trial. Clin Orthop Relat Res 469(1):200–208
DiGioia AM, Plakseychuk AY, Levison TJ, Jaramaz B (2003) Mini-incision technique for total hip arthroplasty with navigation. J Arthroplasty 18:123–128
Lawlor M, Humphreys P, Morrow E, Ogonda L, Bennett D, Elliott D et al (2005) Comparison of early postoperative functional levels following total hip replacement using minimally invasive versus standard incisions. A prospective randomized blinded trial. Clin Rehabil 19:465–474
Smith TO, Blake V, Hing CB (2011) Minimally invasive versus conventional exposure for total hip arthroplasty: a systematic review and meta-analysis of clinical and radiological outcomes. Int Orthop 35(2):173–184
Wohlrab D, Hagel A, Hein W (2004) Advantages of minimally invasive total hip replacement in the early phase of rehabilitation. Z Orthop Ihre Grenzgeb 142(6):685–690 (in German)
Murphy SB, Tannast M (2006) Conventional vs minimally invasive total hip arthroplasty. A prospective study of rehabilitation and complications. Orthopade 35(761–764):766–768 (in German)
Mazoochian F, Weber P, Schramm S, Utzschneider S, Fottner A, Jansson V (2009) Minimally invasive total hip arthroplasty: a randomized controlled prospective trial. Arch Orthop Trauma Surg 129(12):1633–1639
Goebel S, Steinert AF, Schillinger J, Eulert J, Broscheit J, Rudert M, Nöth U (2012) Reduced postoperative pain in total hip arthroplasty after minimal-invasive anterior approach. Int Orthop 36(3):491–498
Ilchmann T, Gersbach S, Zwicky L, Clauss M (2013) Standard transgluteal versus minimal invasive anterior approach in hip arthroplasty: a prospective, Consecutive Cohort Study. Orthop Rev (Pavia) 5(4):e31
Dorr LD, Maheshwari AV, Long WT, Wan Z, Sirianni LE (2007) Early pain relief and function after posterior minimally invasive and conventional total hip arthroplasty. A prospective, randomized, blinded study. J Bone Joint Surg Am 89:1153–1160
Lux EA, Stamer U, Meissner W, Moser K, Neugebauer E, Wiebalck A (2008) Postoperative pain after ambulatory surgery. Schmerz 22:171–175
Landgraeber S, Quitmann H, Güth S, Haversath M, Kowalczyk W, Kecskeméthy A, Heep H, Jäger M (2013) A prospective randomized peri- and post-operative comparison of the minimally invasive anterolateral approach versus the lateral approach. Orthop Rev (Pavia) 5(3):e19
Spaans AJ, van den Hout JA, Bolder SB (2012) High complication rate in the early experience of minimally invasive total hip arthroplasty by the direct anterior approach. Acta Orthop 83(4):342–346
Yang B, Li H, He X, Wang G, Xu S (2012) Minimally invasive surgical approaches and traditional total hip arthroplasty: a meta-analysis of radiological and complications outcomes. PLoS One 7(5):e37947 Epub 2012 May 24
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Repantis, T., Bouras, T. & Korovessis, P. Comparison of minimally invasive approach versus conventional anterolateral approach for total hip arthroplasty: a randomized controlled trial. Eur J Orthop Surg Traumatol 25, 111–116 (2015). https://doi.org/10.1007/s00590-014-1428-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-014-1428-x