Abstract
Background
The goal of the radius diaphysis fractures in surgical treatment is restoration of bone length, rotation correction and to secure fixation that allows early mobilization. The purpose of this study is evaluating the results of intramedullary (IM) radius nail for the treatment of isolated adult diaphyseal fractures of the radius.
Materials and methods
We retrospectively reviewed adults with isolated fractures of the radius, who were treated with closed or mini open reduction with a IM radius nail between May 2008 and November 2011 and who were followed for a least 1 year. Patients with a Galeazzi fracture, a pathological fracture, or patients with nonunion after previous surgeries were excluded. All patients were allowed full range of motion without any external support. Primary outcomes were Grace and Eversmann rating, Disabilities of the Arm, Shoulder and Hand (DASH) scores.
Results
Twenty-three enrolled patients (mean age 34 years; 17 men) had 23 isolated radius fractures. Mean time to fracture union was 12 weeks (range 10–13 weeks) for radius fractures. No patient had nonunion, deep infections, or radioulnar synostosis. Follow-up ranged from 12 to 42 months. Grace and Eversmann ratings of 21 patients were excellent or good, and 2 patients were medium. Mean DASH score was 4.2 points (range 0–13.3).
Conclusions
Our experience indicates that this new IM radius nail may be considered as an alternative to plate osteosynthesis for fractures of the radius diaphysis in adults. IM nailing of radius fractures provides reliable bony union and excellent postoperative clinical results in adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A fracture of the radius diaphysis without an ulnar fracture is an unusual injury in adults. The mechanism of injury is often a high-velocity direct impact with forceful forearm pronation [1, 2]. This injury can result in significant loss of function if treated inadequately. The treatment goal for diaphyseal radius fractures in adults is to restore length to enable axial and rotational stability [3–5]. The type of fracture and localization, degree of displacement, patient age, and magnitude of the soft tissue injury are important for determining the treatment options for these injuries. In addition, an evaluation of the distal radioulnar joint (DRUJ) is important to rule out a Galeazzi injury [5, 6]. Open reduction and plate–screw osteosynthesis have been recommended by most authors [4, 7]. However, plate–screw osteosynthesis has some disadvantages, such as draining of the fracture hematoma, soft tissue damage, and disruption of the periosteal blood supply by plate compression, which can prevent periosteal revascularization [3, 4, 8].
Closed locked nailing is used for treating femoral, tibial, and humeral shaft fractures [9, 10]. However, intramedullary (IM) nails are not routinely used in the surgical treatment of radius fractures because they cannot provide sufficient rotational and linear stability in this region. However, this trend has started to change with the recent introduction of newly designed interlocking IM nails [3, 4, 8, 9, 11].
The purpose of this study was to evaluate the effectiveness and results of using new IM radius nails for the surgical treatment of adults with isolated radius diaphysis fractures.
Materials and methods
Ethical clearance was obtained from the institutional ethics committee, and informed consent was received from all patients. Patients were enrolled between May 2008 and January 2012. Standard anteroposterior and lateral radiographs of the fractured forearm taken at the time of injury were used to classify the fractures according to the system used by the Arbeitsgemeinschaft fϋr Osteosynthesefragen/Orthopedic Trauma Association [12]. The inclusion criteria were a radius diaphyseal fracture, either a closed fracture, a grade I–II or III a open fracture, or a simple segmental fracture. Patients with a Galeazzi fracture, fractures of the radial neck, pathological fractures, or patients with nonunion after previous surgeries were excluded.
The study comprised 23 adult patients with no DRUJ injury from 32 radial diaphysis fractures. Of the 23 eligible patients, 17 were males with a mean age of 34 years (range 18–65 years). The right forearm was fractured in 18 patients and the left in five. The mechanisms of injury were motor vehicle accidents in four patients, industrial accidents in four, sports injuries in three, and falls in 12. There were 19 type A (simple) fractures and four type B (wedge) fractures. Three open fractures were treated with debridement, irrigation, and IM nail fixation on the day of admission. The cases with open fractures, their preoperative preparation was done after admission to the hospital, and they were operated on within 24 h. All other fractures were stabilized within 4 days (range 1–6 days) after injury. Mean length of hospital stay was 4 days (range 3–10 days). The follow-up period was at least 12 months (range 12–44 months) for all 23 patients.
Design of the IM radius nail
The radius nail is made from a titanium alloy. It has parabolic body, a 10° angle at the proximal 3 cm, and distal interlocking features that provide three-point fixation. All fractures were stabilized with the IM radius nail (TST Rakor Tıbbi Aletler San. ve Tic. Ltd. Şti., Istanbul, Turkey). Distal static locking can be achieved by placing a locking screw inside the 17° proximal-volar angled oblique hole at its distal end. Locking screws are 2.7 mm in diameter and are available in 6, 18, 20, 22, and 24 mm lengths. Diameter choices for the radius nails are 3, 3.5, and 4 mm, and the length choices for the nail are 18, 19, 20, 21, 22, 23, and 25 cm. The same nail can be used for the right and left radius (Fig. 1).
Biomechanics analysis of the IM radius nail
A biomechanical analysis was conducted using IM radius nails of the same length and diameter placed in synthetic radius bones (Saw-bones Europe AB, Malmo, Sweden; 4th Generation Composite Radius). The radius nail was applied to all sawbones from the second extensor tunnel, and distal locking was performed with one screw. A fracture was created with a Gigli saw in the same area of the diaphysis of the sawbones, and the following four tests were applied for the biomechanical analysis: axial pressure, bending, torsion, and fatigue. An Instron static–dynamic test device was used for axial pressure, and the four-point bending and fatigue and torsion tests were conducted with a Jinan NDW-200 torsion test device (Fig. 2).
The axial pressure and static bending experiments were conducted at 10-mm/min and the bending test at 5°/min. The fatigue test used a loading rate of R = 0.1 and a frequency of 5 Hz. The tests for axial pressure, four-point bending, and torsion were terminated when there was damage to the bone or implant. The fatigue tests were based on the model reaching 1,000,000 circuits without damage. In all tests, elastomer materials were placed on the joint surfaces to simulate the loading that could be placed on the joint surfaces. The results of the axial pressure tests showed that there were no cracks or breaks in any screw or IM nail in any of the radius models. Nail bending was observed as a result of deformation arising from loading. Increased loading in the models increased the amount of twisting and displacement. A mean maximum pressure force of 669.2 ± 84.4 N was obtained for all models (Table 1).
In the results of the four-point bending test of the radius models, no damage was encountered in any of the screw connections or the synthetic bone. Increased load increased the displacement amount, and there was bending due to nail deformation. The mean maximum bending force obtained was 539.75 N for all models (Table 1).
In the torsion test results, no damage was seen in any implant, and wear was seen only in the bone models in the parts in contact with the jaws of the torsion device. As torsion moment increased, turning angle also increased. Each model displayed different tendencies in the torsion tests. The highest torsion moment and turning angle value were obtained from the first model (Table 2).
The fatigue tests revealed that a reduced load to the radius models increased the number of cycles. There was nail breakage in four radius models at the level of the diaphyseal region where the fracture line had been created. No damage was encountered in the screw connections or in the synthetic bones of the radius models during the tests (Table 3).
Surgical technique
All patients received an axillary block or general anesthesia. In all cases, closed reduction was attempted initially. If closed reduction could not be achieved, we proceeded to open reduction by placing a 2-cm incision at the fracture line. Open reduction was done to irreducible forearm fractures when it is closed, with soft tissue interposition, with 1/3 proximal displacement or butterfly fragment. For the open reduction, firstly, the level of fracture was defined with fluoroscopy, and then 2-cm mini incision was applied. After moving the nail forward to the fracture line and reduction was provided, then the nail was pushed forward to the proximal fragment.
The nail was inserted with the patient supine on a radiolucent operating table. The nail for the radial fracture was selected based on the length and diameter of the medullary canal as measured on anteroposterior and lateral radiographs of the uninjured forearm.
A 2-cm dorsal–radial incision was made on the radial side of the Lister tubercle 1–1.5 cm proximal to the wrist. The extensor carpi radialis brevis tendon sheath was exposed by blunt dissection. The sheath was opened longitudinally and reflected to the radial side, and the nail was introduced from the metaphysis toward the medulla using the second tunnel with the help of a bone awl (Fig. 3a). The first, second, or fourth tunnel can also be used, according to surgeon preference. The nail was then introduced proximally by partial rotation with the help of a nail holder (Fig. 3b). If closed reduction was not established, reduction was performed under C-arm fluoroscopy control or using a mini open incision. The nail was then advanced as far proximally as possible. The nail was fully adapted with a final impactor, and distal interlocking was performed through the same incision (Fig. 3c).
Outcomes
Anteroposterior and lateral radiographs of the forearm were taken during follow-up. Union was assessed clinically and radiographically. Radiographic union was defined as an evident bridging callus on the anteroposterior, lateral, and oblique radiographs of the forearm. Clinical bone union was defined as a non-tender fracture site. The DRUJ was evaluated on the original injury films before manipulative or surgical reduction. Injury to the DRUJ was defined as >5 mm of positive ulnar variance on radiographs taken before any manipulative or surgical reduction. The degree and location of the maximum radial bow (MRB) were described by Schemitsch and Richards [13].
Postoperative hand and forearm strength were assessed with a dynamometer (Baseline hydraulic hand dynamometer, Hixon, TN, USA). Grip strength was measured when the patient was seated, with the shoulder adducted and in neutral rotation, with the elbow flexed at 90°, and the forearm and wrist in the neutral position. The average of three measurements was recorded. All measurements were taken within 2 min to avoid fatiguing the muscle. The uninjured forearm was used as a control for each patient. All measurements were done at least 12 months after surgery.
Functional outcome was assessed with the Grace and Eversmann rating system [14]. Patient-reported outcomes were assessed by the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire score [15]. Wrist flexion and extension were measured with a goniometer.
Statistical methods
In addition to defined statistical methods (mean, standard deviation, median, frequency, and ratio), the paired sample t test was used to evaluate the normal distribution of the parameters on the healthy and operated sides. Spearman’s correlation analysis was used to evaluate the relationships between parameters. Grip strength was compared between the fractured and uninjured forearms with the paired sample t test. Relationships between grip strength, pronation, and supination were assessed by Pearson’s correlation coefficient.
Alpha was set at 0.05, and all tests were two-tailed. The statistical analysis was performed using the NCSS Statistical Software (Number Cruncher Statistical System, 2007 & PASS 2008).
Results
Mean operative and fluoroscopy times showed variation with the learning curve. Mean fluoroscopy time for isolated radius fractures was about 72 s in the initial stages of our series and about 10 s at the end (Table 4). Mean recovery times did not differ significantly between patients undergoing open and closed reduction. All patients were allowed tolerably free movement without a cast or splint after postoperative day 1. Extensor pollicis longus (EPL) rupture was not seen in any of our cases. In our cases, the implant was not removed for any problem or reason.
Standard radiographs taken at the most recent follow-up showed no nonunion. Callus tissue was clearly apparent on radiographs in all cases about 5 weeks after surgery. The average healing time was 12 weeks (range 10–13 weeks) for a radius fracture (Table 4). The overall average range of motion was 84° of pronation and 82° of supination (Table 4). No significant difference was observed between the radial lengths of the fractured and uninjured forearms (p = 0.248). However, the difference of 11.73 ± 12.12 lbs in grip strength between the fractured and uninjured forearm was highly significant (p = 0.001) (Table 4).
In addition, the difference between the MRB measurements of the fractured and uninjured forearms in the current series was significant (p = 0.001). The difference of 2.30 ± 2.47 units between the “location of the MRB” percentages of the fractured and uninjured forearms was also highly significant (p = 0.001) (Table 4). When compared with the uninjured side, no significant relationship was seen in the change in forearm grip strength of the operated side with the change in MRB. Grace and Eversmann ratings of 21 patients were excellent or good, and ratings of two patients were medium. The overall mean DASH score was 4.2 (Table 4).
Discussion
Fractures of the isolated radius diaphysis are relatively rare injuries. In adults, the treatment concept for an isolated radius fracture is less well accepted and usually describes Galeazzi fractures alone [1, 2, 16]. Several studies have indicated that diaphyseal radius fractures without radioulnar dislocation occur more frequently than Galeazzi lesions [17, 18]. DRUJ involvement did occur in all cases in the current study of isolated radius diaphysis fractures. In a series of 36 patients with radius diaphysis fractures by Ring, nine (25 %) had DRUJ involvement [18]. In this study, 23 patients without DRUJ injury among 32 patients with radius diaphyseal fractures were included. The rate of DRUJ involvement in our series is 28 %. As in all fractures, the functional and successful outcome of an isolated radius diaphysis fracture depends on preserving the proper interaction between neighboring joints and adequate fixation. Thus, different treatment methods can be applied [7, 9, 11, 14, 18].
It is generally accepted that surgical management is the ideal treatment of adult displaced diaphyseal radius fractures. Plate osteosynthesis is the most common procedure of choice for treating radius fractures [3, 4]. In the treatment of forearm fractures with plate–screw osteosynthesis, different union rates have been reported. Anderson et al. [19] treated 330 forearm fractures of 258 patients by using compression plates, and they achieved 96.3 % union rate in ulna fractures and 97.8 % in radius fractures. Moed et al. [20] in their 50 patients with mostly open fractures applied immediate internal fixation with plate–screw achieved 91 % union rate. In other studies, the union rates have been reported as between 87 and 98 % [21–23]. In all of the patients we applied IM nailing, in our series, we achieved 100 % union.
In terms of functional recovery and results, Leung and Chow [23] in the patients they used dynamic compression plate had excellent and good results with 98 %. Moed et al. [20] had 85 % excellent and good result in their 50 patients they treated with plate–screw method. Also, Schemitsch and Richards [13] reported 80 % excellent and good functional result in their 55 patients they applied plate–screw method. In our existing study, we used IM radius nail in our 23 cased series we had 91.3 excellent and good, 8.7 % medium results.
There are different views about the union time fixation of forearm fractures with plate–screw in adults. Anderson et al. [19] achieved union in average of 7.4 weeks in patients done with open reduction and plate–screw fixation. Leung and Chow [23] used two different implants in the treatment of forearm fractures; they reported mean union time as 17 weeks in the group of patients whom they used limited contact dynamic compression plate (LC-DCP) with. Stevens and ten Duis [22] reported in the cases they used LCP plates that they had union in 33 weeks, in the patients they used DCP plates they had union in 22 weeks. In contrast, Gao et al. [3] who used closed locked intramedullary nail in their treatment reported the average union time of 10 weeks for closed fractures, 14 weeks for open fractures. Lee et al. [4] reported the mean union time of 14 weeks in 27 patients, Weckbach et al. [9] in 29 patients the mean union time of 4.4 months. In our series, the mean union time is 12 weeks in the cases with isolated radius diaphysis fractures treated with IM nail.
The first IM nail results were reported by Sage and Smith [24], and subsequently, various nails were developed to stabilize forearm fractures [4]. In the study by Sage et al. the IM nail was protected with a long arm cast for 3 months. A 6.2 % nonunion rate was reported, as well as difficulty restoring normal forearm motion [24]. Weckbach et al. [9] treated 33 forearms with fractures of the radius, ulna, or both bones with the new IM nail and reported a 97.5 % union rate at 4.4 months with an average DASH score of 13.7, and full range of motion restored in 86 % of cases. Lee et al. [4] applied precontoured fluted IM nails in 38 patients with either isolated or combined fractures of the radius and ulna. They achieved 92 % good to excellent results with an average DASH score of 15. In our series, we did not see nonunion, and union time was similar to that of plate osteosynthesis.
The radius nail that we used in our series provides rotational stability by means of its parabolic body. It also minimizes scope usage and does not require an additional incision for distal locking. Furthermore, the proximal and distal design of the radius nail contributes to restoring radial bowing and radial length. In our study, no significant difference was observed between the measurements of the radial length in the fractured and uninjured forearms.
The radius has a complex geometric structure due to its anatomical shape. A good functional outcome can be achieved by restoring normal radial bowing [13]. However, laboratory studies have shown that no significant functional impairment will result if angular or rotational malunion of the forearm bones is <10° in any plane [13, 25]. Full anatomical integrity of the bone may be provided with open reduction and plate–screw application, but even in this condition, the loss of rotational function can be seen in the forearm. Because the loss of rotational function is not only associated with failure of providing full anatomical integrity of the bone; this condition can also be caused by various reasons such as soft tissue fibrosis, narrowing of the interosseous distance, the relative increase in radial length [4, 23]. In the current study, a significant difference was observed between the fractured and uninjured forearms in the measurements of both the MRB and the location of the MRB. However, functional results did not differ significantly between the fractured and uninjured forearms. We think that the reason for the similar results, in addition to the anatomical features of the IM nails, is that the surgery was less invasive and that full movement without additional fixation was allowed immediately after surgery.
No significant relationship was observed between the changes in MRB and forearm grip strength in our operated patients. The reason for this was thought to be that as the nail radius was compatible with normal anatomy, movements and functional use were started immediately without the need for any additional postoperative support.
Proximal interlocking is one of the important problems with IM radius nails. Iatrogenic posterior interosseous nerve injury may be observed during proximally locked intramedullary nailing. We did not use a locking screw for proximal stability. Because there are no extra incision requirements for proximal locking, there is no risk of posterior interosseous nerve damage to this radius nail. Therefore, we did not observe this complication in our series. In addition, damage to the superficial branch of the radial nerve can be avoided by careful preparation at the site of Lister’s tubercle. No nerve damage was seen in our series.
We achieved closed reduction in 20 of 23 fractures, but three had to be reduced through open incisions. Union was obtained in all fractures, and we did not perform grafting in any of our patients.
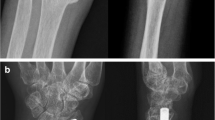
We found that interlocking IM radius nails can be used to treat adult radius diaphyseal fractures. The radius nail is not useful at one entry point (first tunnel); however, it may be performed safely through the second or fourth tunnel. These nails do not require a guide for distal interlocking. Furthermore, they do not need an additional incision for distal interlocking and allow immediate postoperative motion without additional support (Figs. 4, 5, 6, 7).
In conclusion, plate fixation remains the gold standard for treating adult radius diaphysis fractures [1, 2]. However, the newly designed IM nails are an excellent alternative for these fractures. The important advantages of IM radius nail we use in our study are the short time of operation, limited soft tissue dissection, improved cosmesis, significantly short of fluoroscopy time, quick and easy application, and allowing early functional movement without any additional fixation was allowed immediately after surgery. Therefore; we recommend radius interlocking IM nails to treat radius diaphyseal fractures in adults. The IM radius nail results in a union rates similar to those provided by plate fixation. Additionally, the functional and clinical results are very good. So, we think that the new radius nail is an important alternative to plate–screw osteosynthesis.
References
Jupiter JB, Kellam JF (2003) Diaphyseal fractures of the forearm. In: Browner BD, Kellam JF, Levine AM et al (eds) Skeletal trauma: fractures, dislocations and ligamentous injuries, 3rd edn. WB Saunders, Philadelphia, pp 1363–1403
Richards R (2001) Fractures of the shafts of the radius and ulna. In: Bucholz RW, Heckman JD et al (eds) Rockwood and Green’s fractures in adults. Lippincott, Philadelphia, pp 869–920
Gao H, Luo CF, Zhang CQ et al (2005) Internal fixation of diaphyseal fractures of the forearm by interlocking intramedullary nail: short-term results in eighteen patients. J Orthop Trauma 19:384–391
Lee YH, Lee SK, Chung MS et al (2008) Interlocking contoured ıntramedullary nail fixation for selected diaphyseal fractures of the forearm in adults. J Bone Joint Surg Am 90:1891–1898
Reilly TJ (2002) Isolated and combined fractures of the diaphysis of the radius and ulna. Hand Clin 18:179–194
Rettig ME, Raskin KB (2001) Galeazzi fracture-dislocation: a new treatment oriented classification. J Hand Surg 26A:228–235
Hertel R, Pisan M, Lambert S et al (1996) Plate osteo-synthesis of diaphyseal fractures of the radius and ulna. Injury 27:545–548
Višńa P, Beitl E, Pilný J et al (2008) Interlocking nailing of forearm fractures. Acta Chir Belg 108:333–338
Weckbach A, Blattert TR, Weisser Ch (2006) Interlocking nailing of forearm fractures. Arch Orthop Trauma Surg 126:309–315
Brumback RJ, Virkus WW (2000) Intramedullary nailing of the femur: reamed versus nonreamed. J Am Acad Orthop Surg 8:83–90
Bansal H (2011) Intramedullary fixation of forearm fractures with new locked nail. Indian J Orthop 45:410–416
Marsh JL, Slongo TF, Agel J et al (2007) Fracture and dislocation classification compendium 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma 21:S1–S133
Schemitsch EH, Richards RR (1992) The effect of malunion on functional outcome following plate fixation of fractures of both ones of the forearm in the adult. J Bone Joint Surg Am 74:1068–1078
Grace TG, Eversmann WW Jr (1980) Forearm fracture: treatment by rigid fixation with early motion. J Bone Joint Surg Am 62:433–438
Hudak PL, Amadio PC, Bombardier C (1996) Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med 29:602–608
Carr A, Worlock PH (1996) Forearm fractures. In: Gregg PJ, Stevens J, Worlock PH (eds) Fractures and dislocations: principles of management. Blackwell Sciences, London, pp 435–446
Rettig ME, Raskin KB (2001) Galeazzi fracture-dislocation: a new treatment-oriented classification. J Hand Surg Am 26:228–235
Ring D, Rhim R, Carpenter C et al (2006) Isolated radial shaft fractures are more common than Galeazzi fractures. J Hand Surg Am 31:17–21
Anderson LD, Sisk D, Tooms RE, Park WI III (1975) Compression-plate fixation in acute diaphyseal fractures of the radius and ulna. J Bone Joint Surg Am 57:287–297
Moed BR, Kellam JF, Foster RJ et al (1986) Immediate internal fixation of open fractures of the diaphysis of the forearm. J Bone Joint Surg Am 68:1008–1017
Stern PJ, Drury WJ (1983) Complications of plate fixation of forearm fractures. Clin Orthop Relat Res 175:25–29
Stevens CT, ten Duis HJ (2008) Plate osteosynthesis of simple forearm fractures: LCP versus DC plates. Acta Orthop Belg 74:180–183
Leung F, Chow SP (2003) A prospective, randomized trial comparing the limited contact dynamic compression plate with the point contact fixator for forearm fractures. J Bone Joint Surg Am 85:2343–2348
Sage FP, Smith H (1957) Medullary fixation of forearm fractures. J Bone Jt Surg 39:91–98
Mattehews LS, Kaufer H, Garver DF et al (1982) The effect on supination-pronation of angular malalignment of fractures of both bones of the forearm. J Bone Joint Surg Am 64:14–17
Lee SK, Kim KJ, Lee JW et al (2013) Plate osteosynthesis versus intramedullary nailing for both forearm bones fractures. Eur J Orthop Surg Traumatol. doi:10.1007/s00590-013-1242-x
Ozkaya U, Kiliç A, Ozdoğan U et al (2009) Comparison between locked intramedullary nailing and plate osteosynthesis in the management of adult forearm fractures. Acta Orthop Traumatol Turc 43:14–20
Droll KP, Perna P, Potter J et al (2007) Outcomes following plate fixation of fractures of both bones of the forearm in adults. J Bone Joint Surg Am 89:2619–2624
Henle P, Ortlieb K, Kuminack K et al (2011) Problems of bridging plate fixation for the treatment of forearm shaft fractures with the locking compression plate. Arch Orthop Trauma Surg 131:85–91
Conflict of interest
The authors declare no conflict of interest regarding this paper. No authors received any outside or industry funding or grants in support of conducting or preparing this research for publication. The radius nail which is used in this work is developed by Prof. Dr. Fuat Akpinar. It is manufactured by TST Rakor Tıbbi Aletler San and Tic.Ltd. Şti., Istanbul/Turkey.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Saka, G., Saglam, N., Kurtulmus, T. et al. Treatment of isolated diaphyseal fractures of the radius with an intramedullary nail in adults. Eur J Orthop Surg Traumatol 24, 1085–1093 (2014). https://doi.org/10.1007/s00590-013-1398-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-013-1398-4