Abstract
Purpose
Biomechanical comparison between rigid and non-rigid posterior stabilization systems following lumbar interbody fusion has been conducted in several studies. However, most of these previous studies mainly focused on investigating biomechanics of adjacent spinal segments or spine stability. The objective of the present study was to compare biomechanical responses of the fusion devices when using different posterior instrumentations.
Methods
Finite-element model of the intact human lumbar spine (L1–sacrum) was modified to simulate implantation of the fusion cage at L4–L5 level supplemented with different posterior stabilization systems including (i) pedicle screw-based fixation using rigid connecting rods (titanium rods), (ii) pedicle screw-based fixation using flexible connecting rods (PEEK rods) and (iii) dynamic interspinous spacer (DIAM). Stress responses were compared among these various models under bending moments.
Results
The highest and lowest stresses in endplate, fusion cage and bone graft were found at the fused L4–L5 level with DIAM and titanium rod stabilization systems, respectively. When using PEEK rod for the pedicle screw fixation, peak stress in the pedicle screw was lower but the ratio of peak stress in the rods to yield stress of the rod material was higher than using titanium rod.
Conclusions
Compared with conventional rigid posterior stabilization system, the use of non-rigid stabilization system (i.e., the PEEK rod system and DIAM system) following lumbar interbody fusion might increase the risks of cage subsidence and cage damage, but promote bony fusion due to higher stress in the bone graft. For the pedicle screw-based rod stabilization system, using PEEK rod might reduce the risk of screw breakage but increased breakage risk of the rod itself.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the last several decades, there has been an increasing interest in using interbody fusion technique for treating degenerative spinal disorders [1,2,3]. It has been reported that the annual number of spinal fusion surgeries increased by 77 percent between 1996 and 2001 [4]. Anterior, posterior, transforaminal and lateral lumbar interbody fusion are some of the most often used surgical techniques for lumbar arthrodesis, and placement of the intervertebral cage combined with rigid posterior stabilization system such as pedicle screw-based titanium rod fixation has been considered as a gold standard for these fusion approaches [5, 6]. Although the lumbar interbody fusion is an effective treatment option to stabilize degenerative motion segment, restore lordosis and correct deformity [7], adjacent segment degeneration (ASD) has been generally regarded as a long term complication following the fusion surgery.
Studies in the literature have shown that the conventional rigid posterior fixation instrumentation may grossly alter physiologic load transfer at the instrumented level [8], and many researchers believe that the altered biomechanics may play an important role in ASD development [9, 10]. To avoid the adverse effects, several surgeons have attempted to introduce the compliant non-rigid posterior stabilization system, which could provide motion segment with flexibility and induce more uniform load distribution across spine, as an alternative to the rigid system in clinical practice [11,12,13]. Some in vitro experimental and finite element (FE) studies have also been conducted to compare the biomechanical effects of rigid and non-rigid posterior fixations [14,15,16,17]. For example, Kang et al. [16] investigated the effects of variations in material properties of the connecting rods used in pedicle screw-based stabilization system on biomechanics of the adjacent spinal segments after interbody fusion, and the results showed that disc pressure and facet joint contact force in the adjacent segments were lower when using flexible rods made of more compliant materials (e.g., PEEK) than using rigid titanium rods. Considering the fact that pedicle screw-based stabilization technique comes at costs of invasiveness, surgical time and potential nerve root injury, the non-rigid (dynamic) interspinous spacers have also been used by several surgeons as stabilization devices in lumbar interbody fusion [18, 19], and in vitro data from biomechanical tests suggested that the interspinous stabilization devices provided the fused lumbar spine similar stability as the pedicle screw-based stabilization devices [20, 21].
However, most of the previous studies mainly focused on comparing the differences in biomechanics of adjacent spinal segments or spine stability between using rigid and non-rigid posterior fixations, and very few quantitatively dealt with biomechanics of the fusion devices (intervertebral cage or stabilization system itself). Several postoperative complications associated with the fusion devices are recognized, such as cage subsidence/migration or posterior hardware failure [22, 23], and it is believed that a better understanding of biomechanics of the fusion devices is helpful for avoiding these implant-related complications. This study was designed to quantify and compare biomechanical responses of the fusion devices to bending moments at different physiological planes when instrumenting rigid and no-rigid posterior stabilization systems using three-dimensional FE model of lumbar L1–sacrum segment. The von-Mises stresses in implants and endplate were used as risk parameters associated with subsidence and mechanical failure of the fusion devices [24].
Materials and methods
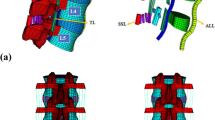
An intact L1–sacrum lumbar FE model, consisting of five vertebrae (including cancellous bone, cortical shell and endplate), five intervertebral discs (including annulus ground substance, annulus fibers, nucleus pulposus) and seven spinal ligaments, was used. The detailed procedures for model development and validation have been shown in the previous works [25, 26]. The L4–L5 segment was chosen as fusion level due to its higher prevalence in individuals suffering from disc degeneration [27], and instrumented with PEEK cage and posterior stabilization system. Anterior lumbar interbody fusion was simulated by removing anterior longitudinal ligament, anterior portions of the annulus and entire nucleus pulposus at L4–L5 level [28], and then a cage was placed within the intervertebral space and was filled with cancellous bone to simulate the embedded bone graft [24], as shown in Fig. 1a. The interface between graft and endplate, as well as cage and endplate, was defined as surface-to-surface contact, and the assigned friction coefficient for graft–endplate and cage–endplate interfaces was 0.3 and 0.8, respectively [29, 30]. Further, the following three kinds of stabilization system were considered. (i) pedicle screw-based fixation using rigid connecting rods (titanium rods), (ii) pedicle screw-based fixation using flexible connecting rods (PEEK rods) and (iii) dynamic interspinous spacer (DIAM), as shown in Fig. 1b–d, respectively. For the pedicle screw-based stabilization systems, four 6-mm-diameter, 45-mm-length pedicle screws were inserted into L4 and L5 vertebral bodies and were interconnected with 6-mm-diameter titanium or PEEK rods. The DIAM system, consisting of a “H”-shape silicone core with a polyester cover, was implanted between spinous process of L4 and L5 where the interspinous ligament was removed for DIAM insertion. For these posterior stabilization systems, a tie constraint was assigned to the implant-bone interfaces via node sharing [16, 31]. Material properties and element types given to components of the FE models are shown in Table 1 [8, 16, 24, 30,31,32,33,34].
Subsequently, caudal part of the L1–sacrum model was fully fixed with application of a 400 N compressive follower preload. Further, additional flexion, extension, lateral bending and axial rotation moments of 7.5 Nm was each imposed on superior surface of L1 vertebral body. Biomechanical responses of the models to the moments were computed using FE static analysis. The parameters in terms of von-Mises stresses in L4 inferior endplate, cage, bone graft and posterior stabilization system were used as the comparison indices. In addition, the final mesh sizes for the models were determined after a mesh sensitivity analysis. The mesh refinement was performed to consecutively generate mesh resolutions until achieving a convergence towards aforementioned parameters, with a tolerance of less than 5% between two consecutive mesh resolutions [35]. The commercial FE analysis software ABAQUS/Standard (Dassault Systems Simulia Corp., Providence, RI, USA) and pre-processing software ANSA (BETA CAE Systems S.A., Thessaloniki, Greece) were employed in this study.
Results
Figures 2, 3, 4 demonstrate stress contour plots in L4 inferior endplate, cage and bone graft, respectively, for the investigated models. It was observed that the stress was concentrated and correlated with the motion direction. For example, in extension the stress was concentrated at posterior side of the endplate, cage and bone graft for all the models; in lateral bending theses, stresses were all concentrated at the same side as lateral bending direction. Also, it was observed from the contour plots that the titanium rod system generated less stress concentration in endplate, cage and bone graft. This was due to the fact that using a rigid fixation transferred the load posteriorly; hence, the anterior support undertook less load and hence less stress concentration. Further, the peak stresses under the different loading conditions are shown in Fig. 5. Compared with using titanium rod system, when using PEEK rod and DIAM systems the peak endplate stress was increased by 2.1–33.3% and 6.3–73.3%, respectively (Fig. 5a), the peak cage stress was increased by 6.9–29.4% and 8.8–64.7%, respectively (Fig. 5b), the peak bone graft stress was increased by 4.9–19.0% and 4.9–44.2%, respectively (Fig. 5c). For the pedicle screw-based rod stabilization system, the stresses in pedicle screws and rods, as well as the ratio of peak stress in the rods to yield stress of the rod material (titanium, 750 MPa; PEEK, 100 MPa) under the different loading conditions are listed in Table 2. It was found that compared with using titanium rod system, when using PEEK rod system the screw stress was decreased by 23.1% in flexion, 12.0% in extension, 24.2% in lateral bending and 36.7% in axial rotation. The ratio range was 5.1–11.1% for titanium rod system and 10.2–15.7% for PEEK rod system, respectively.
Discussion
To reduce ASD after lumbar interbody fusion with conventional rigid posterior fixation, non-rigid posterior stabilization systems have recently been employed to aid in spine fusion and stability. Biomechanical studies have demonstrated that the non-rigid fixation is helpful to restore segmental motion and load transfer of an intact lumbar spine after the fusion surgery [10]. However, there is a lack of studies in comparing the effect of rigid fixation and non-rigid fixation on biomechanics of fusion devices. In present study, a previously validated intact lumbar L1–sacrum FE model was used as a basis to mimic single-level (L4–L5) lumbar interbody fusion with various posterior stabilization systems. By means of these developed FE models, von-Mises stresses in implants and endplate under flexion, extension, lateral bending and axial rotation moments were computed and compared.
Pedicle screw-based flexible rod devices and dynamic interspinous spacers are two of the most used non-rigid posterior stabilization systems for lumbar interbody fusion according to the current literature [11,12,13, 16,17,18,19,20,21]. For the flexible rod system, nitinol and PEEK are some of the most common compliant materials in making of flexible rods, and we have compared biomechanics between the nitinol rod and conventional titanium rod systems in previous studies [28, 36]. For the commonly used interspinous spacers such as Coflex, DIAM, Wallis and X-STOP, previous study has shown that they have a similar effect on biomechanics of human lumbar spine in spite of their different designs [37]. Accordingly, the PEEK rod and DIAM systems were considered herein.
The results illustrated in Figs. 2 and 5a indicate that when using non-rigid fixation, the peak stress in L4 inferior endplate was higher than using rigid fixation. Previous biomechanical studies have shown that a higher stress in the endplate adjacent to the interbody cage might result in greater cage subsidence [24, 38]. Therefore, the present findings imply that application of the non-rigid fixation for lumbar interbody fusion might increase the risk of cage subsidence. Because cage subsidence occurs most commonly at the lower endplate of upper vertebra [39], only the stress in L4 inferior endplate was computed. The results illustrated in Figs. 3 and 5b indicate that when using non-rigid fixation, the peak cage stress was higher than using rigid fixation, which implies that application of non-rigid fixation for lumbar interbody fusion might increase the risk of cage damage. The results illustrated in Figs. 4 and 5c indicate that when using non-rigid fixation, the peak bone graft stress was higher than using rigid fixation, and based on Wolff’s law this higher stress might be better for promoting bony fusion. To sum up, the present results indicate that the load transmitted through the anterior spinal column was increased when using non-rigid fixation, which supports the prediction of Ponnappan et al. [14] who reported that the non-rigid fixation might provide better anterior column load-sharing profile than rigid fixation. It also confirmed in vitro experimental results of the literature [40, 41], which showed that non-rigid fixation led to less stress-shielding effect.
The stress data listed in Table 2 for the pedicle screw-based rod stabilization systems indicate that the PEEK rod led to lower peak screw stress than the titanium rod, implying that using PEEK rod could reduce the risk of screw breakage. This might also be attributed to the reduced stress shielding caused by PEEK rod, which decreased load through the posterior hardware. This finding also supports the prediction of Ponnappan et al. [14] about potential biomechanical advantages of the PEEK rod system. Furthermore, the stress data indicate that although the peak stress in PEEK rod was lower than that in titanium rod, the ratio of peak stress in the rods to yield stress of the rod material was higher for PEEK rod due to its significantly lower yield stress (yield stress of the rod material: PEEK, 100 MPa; titanium, 750 MPa), implying that the PEEK rod system might face a higher risk of rod breakage. Previous biomechanical studies reported that the rod system made of compliant material (nitinol) had a higher failure rate [36, 42], and the present results support this conclusion. To sum up, just like a coin which has two sides, the PEEK rod system has both advantages and disadvantages. Therefore, it should be carefully used in clinical practice.
Additionally, it is also observed from Fig. 5 that biomechanical differences between using the PEEK rod and DIAM systems are not obvious in all loading direction except under lateral bending. It implies that these two systems provide similar resistance to flexion, extension and axial rotation. The relatively obvious difference under lateral bending might be explained by the fact that the DIAM device was inserted close to the rotation axis for lateral bending and hence limited its resistance to this loading [43]. Overall, the loading–sharing characteristics of DIAM system were not significantly better than those of PEEK rod system according to the present results. However, several potential advantages of such an interspinous spacer were worth discussing based on basic principle of biomechanics. For example, the interspinous spacer usually has lower stiffness than the pedicle screw-based rod device; hence, the interspinous spacer might induce less mechanical and kinematic compensation to its adjacent spinal segment and hence might lead to lower stress and motion at the adjacent segment. It implies that likelihood of ASD might be relatively lower when using the interspinous spacer, which agreed with the clinical results regarding the incidence of radiographic ASD (1% and 10.5% in interspinous spacer group and pedicle screw-based flexible rod group, respectively) [44]. Moreover, the interspinous spacer has several clinical advantages over the pedicle screw-based rod device in terms of skin incision, muscle dissection and short operative time and less intraoperative estimated blood loss [18]. Therefore, interspinous spacer might be a promising candidate posterior stabilization device.
There were several limitations in this study. The geometry of human lumbar spine varies from individual to individual, but only one lumbar FE model derived from a unique specimen was used. Material properties in the models were assumed to be linear elastic. The complex interactions between posterior instrumentations and spine were simplified to be tie constraint. The devices were simulated with the simplest geometry, and no set was used to connect the screw to the rods. The muscles were not included in present models. Although using the follower load technique mitigates the effect of ignoring muscles, the complex contributions of muscles were unable to be entirely replaced. The screw loosening and the “distraction-compression” principle [45] were also neglected. In addition, limited by the available experimental data, only the intact model was validated, and the surgical models were developed using this intact model as a baseline. Overall, the obtained biomechanical data from this study should be viewed as a comparative analysis among different surgical cases due to these inherent limitations of the model.
Conclusions
This study was designed to quantitatively compare the effect of rigid and non-rigid posterior fixation instrumentations on biomechanics of the implants used for lumbar interbody fusion by means of FE method. The results indicated that the peak stresses in endplate, fusion cage and bone graft were higher when using pedicle screw-based PEEK rod and DIAM interspinous systems than using pedicle screw-based titanium rod system, implying that non-rigid fixation might increase the risks of cage subsidence and cage damage but promote bony fusion. Furthermore, it was found that biomechanical differences between PEEK rod and DIAM systems are not significant in all loading direction except under lateral bending. Because the interspinous implantation is a less invasive technique, which has several clinical advantages over posterior pedicle screw fixation, the interspinous spacer might be a promising candidate stabilization device for spine fusion. In addition, the results indicated that when using PEEK rod for the pedicle screw fixation, the peak screw stress was lower but the ratio of peak stress in the rods to yield stress of the rod material was higher than using titanium rod, implying that using PEEK rod might reduce the risk of screw breakage but increase breakage risk of the rod itself.
References
Carragee EJ, Hurwitz EL, Weiner BK (2011) A critical review of recombinant human bone morphogenetic protein-2 trials in spinal surgery: emerging safety concerns and lessons learned. Spine J 11(6):471–491
Tartara F, Bongetta D, Pilloni G, Colombo EV, Giombelli E (2020) Custom-made trabecular titanium implants for the treatment of lumbar degenerative discopathy via ALIF/XLIF techniques: rationale for use and preliminary results. Eur Spine J 44(3):551–559
Chan AY, Lien BV, Choi EH et al (2020) Back pain outcomes after minimally invasive anterior lumbar interbody fusion: a systematic review. Neurosurg Focus 49(3):E3
Deyo RA, Nachemson A, Mirza SK (2004) Spinal-fusion surgery-the case for restraint. N Engl J Med 350(7):722–726
Fan W, Guo LX (2019) A comparison of the influence of three different lumbar interbody fusion approaches on stress in the pedicle screw fixation system: finite element static and vibration analyses. Int J Numer Method Biomed Eng 35(3):e3162
La Barbera L, Wilke HJ, Liebsch C et al (2020) Impact of lordotic cages in the restoration of spinopelvic parameters after dorsal lumbar interbody fusion: a retrospective case control study. Eur Spine J 29(1):36–44
Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ (2015) Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP. LLIF ALIF J Spine Surg 1(1):2–18
Ahn YH, Chen WM, Lee KY, Park KW, Lee SJ (2008) Comparison of the load-Sharing characteristics between pedicle-based dynamic and rigid rod devices. Biomed Mater 3(4):044101
Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE (2004) Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine 29(17):1938–1944
Li C, Liu L, Sh JY, Yan KZ, Shen WZ, Yang ZR (2018) Clinical and biomechanical researches of polyetheretherketone (PEEK) rods for semi-rigid lumbar fusion: a systematic review. Neurosurg Rev 41(2):375–389
Kim YS, Zhang HY, Moon BJ et al (2007) Nitinol spring rod dynamic stabilization system and Nitinol memory loops in surgical treatment for lumbar disc disorders: short-term follow up. Neurosurg Focus 22(1):E10
Yuan W, Su QJ, Liu T et al (2017) Evaluation of Coflex interspinous stabilization following decompression compared with decompression and posterior lumbar interbody fusion for the treatment of lumbar degenerative disease: a minimum 5-year follow-up study. J Clin Neurosci 35:24–29
Kuo CH, Huang WC, Wu JC et al (2018) Radiological adjacent-segment degeneration in L4–5 spondylolisthesis: comparison between dynamic stabilization and minimally invasive transforaminal lumbar interbody fusion. J Neurosurg Spine 29(3):250–258
Ponnappan RK, Serhan H, Zarda B, Patel R, Albert T, Vaccaro AR (2009) Biomechanical evaluation and comparison of polyetheretherketone rod system to traditional titanium rod fixation. Spine J 9(3):263–267
Chou WK, Chien A, Wang JL (2015) Biomechanical analysis between PEEK and titanium screw-rods spinal construct subjected to fatigue loading. J Spinal Disord Tech 28(3):E121–E125
Kang KT, Koh YG, Son J, Yeom JS, Park JH, Kim HJ (2017) Biomechanical evaluation of pedicle screw fixation system in spinal adjacent levels using polyetheretherketone, carbon-fiber-reinforced polyetheretherketone, and traditional titanium as rod materials. Compos B Eng 130:248–256
Hsieh YY, Tsuang FY, Kuo YJ, Chen CH, Chiang CJ, Lin CL (2020) Biomechanical analysis of single-level interbody fusion with different internal fixation rod materials: a finite element analysis. BMC Musculoskelet Disord 21(1):100
Kim HJ, Bak KH, Chun HJ, Oh SJ, Kang TH, Yang MS (2012) Posterior interspinous fusion device for one-level fusion in degenerative lumbar spine disease: comparison with pedicle screw fixation-preliminary report of at least one year follow up. J Korean Neurosurg Soc 52(4):359–364
Chen HM, Chen JY (2012) A novel nonpedicular screw-based fixation in lumbar spondylolisthesis. Biomed Res Int 217:5619350
Karahalios DG, Kaibara T, Porter RW et al (2010) Biomechanics of a lumbar interspinous anchor with anterior lumbar interbody fusion. Spine 12(4):372–380
Gonzalez-Blohm SA, Doulgeris JJ, Aghayev K, Lee WE III, Volkov A, Vrionis FD (2014) Biomechanical analysis of an interspinous fusion device as a stand-alone and as supplemental fixation to posterior expandable interbody cages in the lumbar spine. J Neurosurg Spine 20(2):209–219
Woods KRM, Billys JB, Hynes RA (2017) Technical description of oblique lateral interbody fusion at L1–L5 (OLIF25) and at L5–S1 (OLIF51) and evaluation of complication and fusion rates. Spine J 17(4):545–553
Palepu V, Helgeson MD, Molyneaux-Francis M, Nagaraja S (2019) The effects of bone microstructure on subsidence risk for ALIF, LLIF, PLIF, and TLIF spine cages. J Biomech Eng 141(3):031002
Faizan A, Kiapour A, Kiapour AM, Goel VK (2014) Biomechanical analysis of various footprints of transforaminal lumbar interbody fusion devices. J Spinal Disord Tech 27(4):E118–E127
Fan W, Guo LX (2018) Finite element investigation of the effect of nucleus removal on vibration characteristics of the lumbar spine under a compressive follower preload. J Mech Behav Biomed Mater 78:342–351
Guo LX, Fan W (2018) Dynamic response of the lumbar spine to whole-body vibration under a compressive follower preload. Spine 43(3):E143–E153
Cheung KMC, Karppinen J, Chan D et al (2009) Prevalence and pattern of lumbar magnetic resonance imaging changes in a population study of one thousand forty-three individuals. Spine 34(9):934–940
Fan W, Guo LX (2020) The effect of non-fusion dynamic stabilization on biomechanical responses of the implanted lumbar spine during whole-body vibration. Comput Method Progr Biomed 192:105441
Agarwal A, Palepu V, Agarwal AK, Goel VK, Yildirim ED (2013) Biomechanical evaluation of an endplate-conformed polycaprolactone-hydroxyapatite intervertebral fusion graft and its comparison with a typical nonconformed cortical graft. J Biomech Eng 135(6):061005
Polikeit A, Ferguson SJ, Nolte LP, Orr TE (2003) Factors influencing stresses in the lumbar spine after the insertion of intervertebral cages: finite element analysis. Eur Spine J 12(4):413–420
Lo HJ, Chen CS, Chen HM, Yang SW (2019) Application of an interspinous process device after minimally invasive lumbar decompression could lead to stress redistribution at the pars interarticularis: a finite element analysis. BMC Musculoskelet Disord 20:213
Schmidt H, Heuer F, Drumm J, Klezl Z, Claes L, Wilke HJ (2007) Application of a calibration method provides more realistic results for a finite element model of a lumbar spinal segment. Clin Biomech 22(4):377–384
Más Y, Gracia L, Ibarz E, Gabarre S, Peña D, Herrera A (2017) Finite element simulation and clinical followup of lumbar spine biomechanics with dynamic fixations. PLoS ONE 12(11):e0188328
Zhang MZ, Pu F, Xu LQ et al (2016) Long-term effects of placing one or two cages in instrumented posterior lumbar interbody fusion. Int Orthop 40(6):1239–1246
Ayturk UM, Puttlitz CM (2011) Parametric convergence sensitivity and validation of a finite element model of the human lumbar spine. Comput Methods Biomech Biomed Eng 14(8):695–705
Fan W, Guo LX, Zhao D (2019) Stress analysis of the implants in transforaminal lumbar interbody fusion under static and vibration loadings: a comparison between pedicle screw fixation system with rigid and flexible rods. J Mater Sci Mater Med 30:118
Lee CH, Kim YE, Lee HJ, Kim DG, Kim CH (2017) Biomechanical effects of hybrid stabilization on the risk of proximal adjacent-segment degeneration following lumbar spinal fusion using an interspinous device or a pedicle screw-based dynamic fixator. J Neurosurg Spine 27(6):643–649
Zhang ZJ, Fogel GR, Liao ZH, Sun YT, Liu WQ (2018) Biomechanical analysis of lumbar interbody fusion cages with various lordotic angles: a finite element study. Comput Methods Biomech Biomed Eng 21(3):247–254
Cho CB, Ryu KS, Park CK (2010) Anterior lumbar interbody fusion with stand-alone interbody cage in treatment of lumbar intervertebral foraminal stenosis: comparative study of two different types of cages. J Korean Neurosurg Soc 47(5):352–357
Bozkus H, Senoglu M, Baek S et al (2010) Dynamic lumbar pedicle screw-rod stabilization: in vitro biomechanical comparison with standard rigid pedicle screw-rod stabilization Laboratory investigation. J Neurosurg Spine 12(2):183–189
Gornet MF, Chan FW, Coleman JC et al (2011) Biomechanical assessment of a PEEK rod system for semi-rigid fixation of lumbar fusion constructs. J Biomech Eng 133(8):081009
Kim K, Park WM, Kim YH, Lee S (2010) Stress analysis in a pedicle screw fixation system with flexible rods in the lumbar spine. Proc Inst Mech Eng H 224(3):477–485
Godzik J, Kalb S, Martinez-del-Campo E et al (2016) Biomechanical evaluation of the CD HORIZON spire Z spinal system with pedicle and facet fixation. Spine 41(15):E902–E907
Chou PH, Lin HH, An HS, Liu KY, Su WR, Lin CL (2017) Could the topping-off technique be the preventive strategy against adjacent segment disease after pedicle screw-based fusion in lumbar degenerative diseases? A Syst Rev Biomed Res Int 2017:4385620
Bagby GW (1988) Arthrodesis by the distraction-compression method using a stainless steel implant. Orthopedics 11(6):931–934
Acknowledgements
This project is supported by National Natural Science Foundation of China (Grant No. 52005089, 51875096) and Fundamental Research Funds for the Central Universities (Grant No. N2103010).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fan, W., Guo, LX. & Zhang, M. Biomechanical analysis of lumbar interbody fusion supplemented with various posterior stabilization systems. Eur Spine J 30, 2342–2350 (2021). https://doi.org/10.1007/s00586-021-06856-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06856-7