Abstract
Lumbar spinal fusion using rigid rods is a common surgical technique. However, adjacent segment disease and other adverse effects can occur. Dynamic stabilization devices preserve physiologic motion and reduce painful stress but have a high rate of construct failure and reoperation. Polyetheretherketone (PEEK) rods for semi-rigid fusions have a similar stiffness and adequate stabilization power compared with titanium rods, but with improved load sharing and reduced mechanical failure. The purpose of this paper is to review and evaluate the clinical and biomechanical performance of PEEK rods. A systematic review of clinical and biomechanical studies was conducted. A literature search using the PubMed, EMBASE, and Cochrane Library databases identified studies that met the eligibility criteria. Eight clinical studies and 15 biomechanical studies were included in this systematic review. The visual analog scale and the Oswestry disability index improved significantly in most studies, with satisfactory fusion rates. The occurrence of adjacent segment disease was low. In biomechanical studies, PEEK rods demonstrated a superior load-sharing distribution, a larger adjacent segment range of motion, and reduced stress at the rod-screw/screw-bone interfaces compared with titanium rods. The PEEK rod construct was simple to assemble and had a reliable in vivo performance compared with dynamic devices. The quality of clinical studies was low with confounding results, although results from mechanical studies were encouraging. There is no evidence strong enough to confirm better outcomes with PEEK rods than titanium rods. More studies with better protocols, a larger sample size, and a longer follow-up time are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A spinal fusion is traditionally regarded as the “gold standard” surgery for treating discogenic low back pain, degenerative spondylolisthesis, low-grade isthmic spondylolisthesis, and other lumbar segment degeneration [42]. The main purpose of a fusion surgery is to produce a rigid fusion between the targeted vertebral levels. The mechanical properties of the implant material have a significant impact on the quality and efficacy of a fusion. The widely used titanium rods can provide a high degree of rigidity to the spine, leading to high fusion rates. However, disadvantages of titanium rods such as “over-stabilization,” stress shielding, and adjacent segment degeneration (ASD) have been discussed by many prior authors. Polyetheretherketone (PEEK) rods were introduced to overcome these disadvantages and theoretically have better biomechanical and clinical advantages. As dynamic stabilization, flexible stabilization, or semi-rigid fixation methods for spinal stabilization and fusion have become more popular, PEEK has become a promising candidate material for spinal fusions.
The material properties of PEEK rods (3.2 GPa) are between those of titanium rods (110 GPa) and other dynamic devices, such as DYNESYS, NFlex, etc. [20]. The typical PEEK rod and titanium alloy pedicle screw construct is shown in Fig. 1. This system can achieve a critical balance between sufficient stabilization and symptom relief, mediated by a successful fusion and the reduced interruption of physiologic motion that reduces the risk of ASD. Reports discussing PEEK rods are rare and mostly discuss the results of biomechanical testing. Of those clinical studies available, only articles with a short follow-up period are available. Here, we performed a systematic review to collect and analyze all data available regarding the clinical and biomechanical evaluation of PEEK rods in lumbar spinal fusions.
Objective
The objective of this systematic review was to collect and analyze all the available information regarding the use of PEEK rods in the semi-rigid fusion of the lumbar spine. Clinical and biomechanical data was assessed to compare the performance of PEEK and titanium rods. We hoped to answer the following questions: (1) Do PEEK rods provide comparable fusion rates to titanium rods? (2) Can PEEK rods lower the probability of ASD? (3) What are the mechanical advantages and disadvantages of PEEK rods and will these produce negative long-term outcomes?
Materials and methods
Protocol
The senior authors (Yan and Yang) preset the topic. Later, the topic was developed into detailed clinical questions described above. Discussions were held to develop the detailed eligibility criteria, search strategy, inclusion/exclusion of candidate articles, solutions when dilemma was met, etc. Webinars were held between authors from different institutions. The specific protocol was described below.
Inclusion criteria
All papers that evaluated the utility and outcomes of PEEK rods in lumbar spinal fusions were included in this systematic review. Articles that met the following criteria were included: (1) clinical studies in which a patient cohort underwent a PEEK rod fusion and had a specified follow-up period, (2) clinical studies evaluating construct failure or a retrieval analysis, and (3) biomechanical studies using cadaveric specimens or finite element models to test the strength, durability, fatigue, and other mechanical properties of PEEK rods, range-of-motion analyses, disc or facet pressure analyses, changes in load-sharing distribution post-fusion, and all other qualities of PEEK rods or spinal fusions measured in vitro.
Exclusion criteria
The following types of articles were excluded: (1) articles discussing materials other than PEEK rods, (2) articles in which the full texts were not available, (3) case reports, and (4) studies in which the indications for PEEK rods was not specified.
Literature search
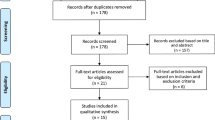
After the eligibility criteria were established, we conducted a literature search in PubMed, EMBASE, and the Cochrane Library using the following keywords or phrases in various combinations: “peek rod(s),” “polyetheretherketone rod(s),” “poly ether ether ketone rod(s),” “semi-rigid fusion,” and “semirigid fusion.” The references from articles included in the final review process were retrieved and assessed using our eligibility criteria. Further detail on the articles produced during our reference evaluation can be seen in Fig. 2. Our final reference update was February 7, 2016.
Study selection
Two authors (Li and Liu) were responsible for article selection and worked independently to generate their reference list. Dr. Liu is a rheumatologist and he was invited in this study to critically and objectively select the articles that met eligibility criteria and extract the data from enrolled studies as a third-party reviewer with a less-related clinical subspecialty background. The two authors worked independently. The abstracts of each article were reviewed, and further full-text reviews were performed if the use of PEEK rods for/or lumbar semi-rigid fusion was discussed. If inconsistent opinions were found, an attempt at a consensus was made. If that failed, other authors were invited into the discussion until a consensus opinion evolved. Data extracted from enrolled articles is listed in Tables 1 and 2.
Quality assessment of each article and consensus recommendations
Quality assessment was performed on each of the selected clinical studies using rating schemes published by The Journal of Bone & Joint Surgery [46] and modified by Norvell et al. [34]. There were no schemes or questionnaires available to evaluate the quality of the biomechanical studies. The rating scores were recorded on a data extraction table (Table 1). After analyzing all the included studies, recommendations were made. The quality of evidence and the strength of the recommendation scores were assessed using a modified Delphi approach by applying the Grades of Recommendation, Assessment, Development and Evaluation (GRADE) criteria [16].
Results
Study selection
The process we employed for identifying and analyzing studies is shown in Fig. 2. A total of 297 articles were identified from 3 databases (112 articles from PubMed, 185 from EMBASE, and no articles from Cochrane). After removing the duplicates, 195 articles were left for abstract review. We excluded 106 additional articles for obvious irrelevance, leaving 89 studies for title and abstract review. Following this review, 28 articles underwent a comprehensive full-text review. Twenty-three studies met the eligibility criteria. Data was extracted and the quality of each individual study was assessed.
Quality assessment
In this systematic review, we wanted to collect all the available information about the clinical applications and biomechanical properties of PEEK rods. The majority of the available clinical studies were case series and therefore had low quality of evidence grades according to our grading system. A retrospective cohort design was used by two of the clinical articles. One article described the in vivo changes and tissue response caused by PEEK rods, and was therefore unable to be graded. No biomechanical study could be assigned an evidence level.
Clinical studies using PEEK rods
Eight clinical studies were included in this systematic review. Seven were case series or retrospective cohort studies. Most discussed the use of PEEK rods in lumbar fusion surgeries. However, Wang et al. [43] and Huang et al. [19] presented case series discussing the use of PEEK rods in a non-fusion technique. Wang assessed 67 patients diagnosed with lumbar degenerative diseases (disc/stenosis/spondylosis) that resulted in some form of instability associated with neurogenic or radicular pain or chronic back pain. These patients underwent a laminectomy or discectomy with pedicle screw fixation using a K-rod system without a fusion. The K-rod system is a flexible rod system composed of titanium alloy cables and a PEEK shell. The mechanical properties of this system will be discussed later in this article. Huang’s patient series included 38 cases. The main indications for surgery were lumbar spinal stenosis, spinal instability with or without disc herniation, and chronic lower back pain. Both studies used patient self-reporting parameters, including the visual analog scale (VAS), the Oswestry Disability Index (ODI), and the Japanese Orthopaedic Association (JOA) score. Radiographic measurements such as the intervertebral disc space (IVS), the segmental lordosis angle (SLA), and the disc height index (DHI) were calculated. The spine range of motion (ROM) was also evaluated. Wang found that the VAS and ODI were both significantly improved after surgery. There were also no obvious changes in the IVS or SLA at the 2-year follow-up. Huang found a significant improvement in the JOA and ODI. The DHI was slightly increased from 0.3 to 0.32 immediately after surgery, although it declined to 0.27 at the final follow-up. The lumbar spine ROM decreased from 8.8° preoperatively to 2.1° 3 months postoperatively, stabilizing to 1.8° at the final follow-up. There was one case of screw loosening without clinical symptoms. As this was a non-fusion surgery, no fusion rates could be estimated.
Most authors reported using PEEK rods for lumbar fusions. In a retrospective cohort study, Colangeli et al. [10] discussed the results of 12 patients who received PEEK rod instrumentation compared with another 12 patients who received the NFlex system (N spine Inc., San Diego, CA). The authors reported a significant improvement in the VAS, ODI, and Euro Qol-5D results in both fusion groups. The PEEK rods had no complications or hardware failures and had superior outcomes compared with the NFlex system. All patients in the PEEK rod group had a fusion at the 6-month follow-up.
In another case series reported by Ormond et al. [35], 42 consecutive patients underwent an instrumented fusion using PEEK rods for degenerative lumbar spinal disease for a chief complaint of axial back pain. The fusion rate in this case series was 89.3 % (25 out of 28). Eight out of 42 patients had a reoperation. The indications for the reoperations were 5 ASDs, 2 cage mitigations, and 1 screw fracture. The follow-up period was 31.4 months (range 3–62 months). The authors observed that the reoperation rate was high in this small case series and ASD was the most common indication for a reoperation. The authors therefore concluded that PEEK rods were less beneficial in lumbar fusions than traditional titanium rods.
Qi et al. [37] compared the outcomes of 20 patients who received PEEK rods with 21 patients who received traditional titanium rods. The fusion rates were 100 % in both groups at the 1-year follow-up. There were no statistically significant clinical outcome differences between the two groups, which was scored with JOA and the VAS, or radiographically, which was assessed by comparing the segmental lordosis angles and disc height measurements between the two groups.
Two authors focused on complications specifically. Athanasakopoulos et al. [3] performed a case series study that showed a significant improvement in the ODI and VAS scores after surgeries. The fusion rate was 96 % at the 1-year follow-up. One patient had a screw breakage at the head-screw interface but remained pain free. No reoperation was needed and fusion was achieved at the 2-year follow-up. De Lure et al. [11] reported the results of a 30-patient cohort study in which 22 patients underwent an anterior interbody fusion (AIF) and eight only received posterolateral autologous grafting. At the 1-year follow-up, all of the AIF patients and seven out of the eight autologous grafting patients had a successful fusion. With respect to complications, revision surgery was required for one dural tear, one superficial wound dehiscence, one deep infection, and one cranial screw mobilization.
A retrieval analysis was performed by Kurtz et al. [26], who assessed 12 patients that required revision surgeries for previously instrumented PEEK rods because of intractable pain. The mechanisms for this pain were varied, including ASD (four cases), pseudoarthrosis (three cases), screw loosening (one case), epidural seroma (one case), hardware-related muscular paravertebral pain (one case), residual osteophytes (one case), motor vehicle trauma (one case), and screw impingement and nerve root encroachment (one case). No cases of PEEK rod fracture or pedicle screw failure were included. The most commonly observed finding between all cases was a plastic deformation at the screw-rod interface. Burnishing and scratching were minor (Fig. 3). Degeneration, inflammation, calcification, PEEK debris, and metal wear could be seen in the periprosthetic tissue (Fig. 4).
Examples of surface damage in retrieved PEEK rods. Plastic deformation of the convex (a) and concave (b) surfaces of a patient underwent revision surgery. Impressions from the pedicle screw and set screw (c). And titanium end cap discoloration (d). Note that rods in c and d are different from rods in a and b. Image courtesy of Steven M. Kurtz et al. Adapted from [26], with permission from Springer
Histologic (a) and polarized (b) images of PEEK rod tissues (×400 magnification) from a patient who underwent revision surgery. The black arrows indicate the encapsulated PEEK wear debris and associated inflammation. The white arrows indicate PEEK wear particles. Image courtesy of Steven M. Kurtz et al. Adapted from [26], with permission from Springer
Biomechanical studies
Fifteen articles regarding in vitro biomechanical tests were included in this review. Eight were finite element studies (F-E) while others used models or cadaveric specimens. As a result of differences in model properties, test methods, and other influencing factors, the test results of these biomechanical studies cannot be measured across studies. Several biomechanical tests had questionable clinical applications. Many results across studies were also conflicting. We therefore only listed the parameters deemed most important to in vivo performance.
The ROM of the lumbar spine was reported in 10 studies [1, 5, 7, 14, 15, 20, 30, 36, 39, 40]. All included articles concluded that the use of PEEK rods could significantly decrease the ROM of the fused level. Whether or not this was significantly different when other fusion materials were used remains controversial. When the spine ROM was subdivided into single-plane motion measurements, the results were also controversial. Abode-Iyamah et al. [1] reported that PEEK and titanium rods can significantly reduce the lumbar spine ROM in flexion and extension but not in axial rotation or lateral bending compared with controls. Shih et al. [40] showed that the ROM at the implant level increased in the following order based on technique group: rigid, semi-rigid, dynamic intact, and disc degeneration. Gornet et al. [15] found that the lumbar spine ROMs of fusions with PEEK rods were greater than that permitted by titanium rods in every motion direction. As for adjacent ROM compensation, Galbusera et al. [14] reported similar changes in value between titanium rods, stainless steel rods, Osta Pek, and PEEK rods. However, PEEK rods permitted half the axial rotation allowed by its counterparts. A smaller difference in ROM was observed in pedicle flexible devices (FlexPLUS, DSS). Shih et al. found that the lumbar spine ROM increased in the following order: dynamic, semi-rigid, and rigid [40].
Intradisc pressure (IDP) or disc stress is thought to be connected with postoperative ASD. This relationship was reported in seven studies [1, 7, 9, 15, 21, 30, 40]. When applied to posterior pedicle screws and PEEK rod fixation, the IDP from instrumented segments was comparable to that of intact models and was greater than that of titanium rod constructs [9]. The IDP at the implant level increased in the following order: rigid, semi-rigid, and dynamic instrumentation. In contrast, the IDP at adjacent levels increased in the reverse order [40]. The IDP of the cranial adjacent level was increased in both the PEEK and titanium rod groups, with a greater increase in the titanium group [1] during extension, axial rotation, and lateral bending but flexion [9, 15]. The IDP changes at the cranial adjacent level in the PEEK group were significantly less than those in the titanium group, but were slightly greater than those in the titanium group at caudal adjacent levels [21]. One report suggested that the stress increment in the upper disc was larger than that of the lower disc, and the stress values of PEEK fusions were lower than those of titanium fusions regardless of the fusion type and the direction of motion [7]. A report [30] comparing PEEK rods to another dynamic system (Dynesys) indicated that the stress from the cranial adjacent disc was 1.29 and 1.02 times that of an intact model in the PEEK rod and Dynesys groups, respectively.
Load sharing was evaluated in three studies [2, 15, 39]. Sengupta et al. [39] concluded that anterior load sharing decreased in the following order: posterior dynamic stabilizers, PEEK rods, and titanium rods. Gornet et al. [15] found that in all loading scenarios PEEK rods carried at least 6 % less load than titanium rods. Ahn et al. [2] showed that PEEK rods absorbed compressive forces the least and had more anterior column forces than nitinol or titanium alloy rods.
Other mechanical parameters, such as facet joint contact force, the strain at the screw-bone interface, construct strength, and load fatigue, were reported in several papers [41] and listed in Table 2.
Discussion
Traditional lumbar spinal fusion surgeries aim to eliminate physiologic movement and provide absolute stabilization for the instrumented segments. Lumbar fusion with rigid rod fixation is the “gold standard” surgery for posterior lumbar instability, resulting in a high fusion rate and good clinical outcomes. However, several significant complications of spinal fusions, including ASD, non-union, hardware failure, and chronic pain, have been reported [12, 28]. The non-union and ASD rates are the most concerning of these complications.
Among the eight clinical studies included in our review, five studies used PEEK rods for fusions. The interbody fusion rate varied from 89.3 % [35] to 100 % [3, 10, 11, 37]. One author used two fusion technologies: an anterior interbody cage and posterolateral autologous grafting. The fusion rate was 100 % (22/22) for the anterior interbody cage and 87.5 % (7/8) for the posterolateral autologous grafting groups [11]. The studies that reported fusion rates below 100 % were all case series without control groups. No comparison of the time until fusion was performed between the different groups. Most studies included patients with single-level pathology. Based on these facts, the data regarding the fusion rate of PEEK rods is inconclusive.
The etiology of ASD is still uncertain. Some believe that it has a connection with the supraphysiologic stress applied to adjacent segments, causing accelerating disc and facet joint degeneration. Conversely, others suggest that ASD is nothing but a natural process of our lumbar spine that has little connection with surgeries [27]. Physical loading conditions and muscle tones are traditionally suspected of causing accelerated disc degeneration. However, the Twin Spine Study challenged this view [4], finding that a discordance in the occupational and leisure-time physical loading conditions throughout adulthood between twins has little effect on disc degeneration. It is therefore difficult to conclude which factor plays a major part in disc disease [45]. In our systematic review, we mainly focus on the clinical and radiographic ASD observed after spinal surgery. Lumbar surgeries have been associated with the development of ASD. Many studies have attempted to find a correlation between ASD and various kinds of spinal surgeries. Redcliff et al. [38] performed a review and found that the rate of ASD after decompression and stabilization surgeries is approximately 2–3 %. Factors that are consistently associated with ASD include a laminectomy adjacent to a fusion site and sagittal imbalance. Motion-sparing technology findings were too inconsistent to [22, 47] create a positive correlation between any measured factor and ASD [17, 24]. In a recent systematic review, Wang et al. [44] pooled cohort and randomized controlled studies to measure the relative risk of ASD in spinal fusion patients compared with patients who received a total disc replacement. The authors concluded that there is a higher risk of ASD following a fusion than a total disc replacement. However, data regarding other types of motion-preserving devices, such as dynamic fusion devices, is lacking.
The development of ASD in patients with semi-rigid fusion technology has been under-evaluated. From the studies included in this systematic review, only one article addressed this problem. Ormond et al. [35] investigated 42 consecutive patients fused with PEEK rods. Five patients (11.9 %) underwent a reoperation because of ASD. While the authors did not specify the standard for diagnosing ASD, the study was designed as a small case series with a short follow-up period and no control group, thus making the results less conclusive. It is a paradox that ASD should be the most concerning complication of spinal fusions and also the least evaluated.
The source of lower back pain has not yet been fully discussed. Recent studies show that instead of the abnormal motion of spine segments, an abnormal load pattern is responsible for degenerative low back pain [32]. Eliminating intradisc stress would do little to help alleviate the pain. This may be why the clinical efficacy of rigid fusions reaches a plateau phase decades after surgery [6]. So what would happen if we alter the load-sharing pattern of the degenerative spine and control abnormal motion while decreasing the supraphysiologic pressure on the structures of the spine? This is the goal of dynamic fusion [33].
There are three studies that performed non-fusion surgeries using PEEK rods [19, 29, 43]. Two were performed by the same senior author at the same institution [29, 43]. One was excluded because of a lack of a specific indication for surgery [29]. Although early results showed a significant improvement in the self-assessment parameters (VAS, ODI, JOA), a conclusion on the efficacy of PEEK rod use without a fusion cannot be made because of the small overall sample size, the lack of a control group in all studies, and bias related to the self-assessment parameters. There was one case of screw loosening without clinical symptoms [19]. Worries about construct failure need further verification with a longer clinical follow-up. The FDA only approved PEEK rods to be used as fusion adjuncts [25].
Many authors have tried to develop new materials suitable for dynamic lumbar fusions. This field has not been well studied both theoretically and clinically. There are contradicting definitions of what a dynamic fusion is. Semi-rigid fusions can be referred to as flexible fusions, dynamic fusions, or soft stabilization [8, 23, 33]. There are other devices that fall into this category, such as the Graf ligament (SEM Co., Mountrouge), the Isobar TTL (Scient’x Alphatec Spine, Bretonneux), the DYNESYS (Zimmer Spine, Minneapolis), and many others [6]. However, some authors have pointed out that the performance of PEEK rods was different than other dynamic fusion devices. Others assert that a semi-rigid fusion cannot be equal to dynamic fusions [14]. Based on the different rigidities provided by the hardware, we agree with a classification that subdivides posterior pedicle-screw-based lumbar fusion technologies into rigid, semi-rigid, and dynamic fusion devices.
Highsmith et al. [18] published the first formal clinical application and study of PEEK rods. In his paper, three cases of PEEK rods used for different indications were presented. One was the de novo treatment of spinal instability, the second was revision surgery for ASD, and the third was the use of a hybrid PEEK rod/titanium screw construct to create a tension band. This paper was not included in the review because of its study design (case report).
Theoretically, PEEK rods have several pros and cons. The advantages of PEEK rods compared with traditional titanium rods are the following: (1) A less-rigid profile makes the modulus of PEEK rods closer to that of cortical bone and thus provides more load sharing with the anterior column and better fusion rates according to Wolff’s law [13]; (2) more physiologic motion is permitted because of PEEK’s increased elasticity, potentially reducing the likelihood of ASD; (3) reduced rod-screw interface stress, a simple structure, and a lower possibility of hardware failure; (4) reduced rod-bone interface shear forces, which is suitable for osteoporotic vertebrae; (5) a radiolucent character, minimizing radiographic artifacts and allowing for the more reliable detection of a fusion mass (An example is shown in Fig. 5); (6) PEEK is easy to mix with other materials, such as carbon fiber or titanium alloy fiber, to adjust the rigidity and elasticity of rods for individual treatment; and (7) less stress is applied to the constructs, which reduces the chances of hardware failure compared with dynamic fixation devices. Disadvantages include the following: (1) The very radiolucent character of PEEK rods can make the early detection of rod breakage difficult, although no single PEEK rod break was reported in this systematic review; (2) most authors recommend only indicating PEEK rods for semi-rigid fusion in mild degenerative lumbar disease because of the lack of data on the use of PEEK rods in other clinical scenarios, such as vertebral fractures, unilateral fusions, or simple fixations without a fusion; and (3) greater implant expense [18, 20, 31].
However, after analyzing the biomechanical properties of these devices, we note several differences between PEEK rods and other dynamic stabilization devices. PEEK rods are more like rigid titanium rods in some aspects, although they maintain some of the merits of dynamic devices. The stiffness of PEEK rods is greater than that of other dynamic devices, such as NFlex and DYNESYS. Many studies demonstrate similar ROMs between PEEK and titanium rod fusions [14, 20]. However, the load-sharing pattern of PEEK rods is distinct from titanium rods. In a biomechanical study comparing titanium, PEEK, and the TRANSITION dynamic stabilization device (Globus Medical, Audubon, PA), Sengupta et al. demonstrated that the anterior loading of titanium, PEEK, and TRANSITION was 55 %, 59 % and 75 %, respectively [39]. This indicated that the load-sharing proportion of PEEK rods is significantly different than that of TRANSITION devices and is similar to titanium rods. The decreased ROM and increased anterior load sharing could theoretically promote a fusion and alleviate lower back pain.
Two alternative types of PEEK rods are mentioned in biomechanical studies: carbon fiber-reinforced PEEK (CFRP) [5] and titanium alloy cable with PEEK-coated rods (K-ROD) [30]. The stiffness of CFRP is higher than that of pure PEEK and lower than that of titanium (Table 2), which may therefore increase the risk of intraoperative fracture when securing the rods with pedicle screws. K-ROD has a titanium alloy cable rod with a diameter of 3 mm and a PEEK spacer with a diameter of 4 mm. There is no data that directly compares K-ROD with PEEK. According to a finite element study performed by Lin et al. [30], the K-ROD system still appears to fall into the category of semi-rigid fusion devices. However, only one cohort study from Taiwan used K-ROD as a semi-rigid fixation without fusion [43]. No clinical studies have been performed on CFRP.
Following the examination of the clinical studies included in this systematic review, we observed several limitations: (1) Most authors did not report on the occurrence of ASD, which is an important variable concerned with semi-rigid fusion. For those who did report, the follow-up period was not long enough (maximum 36 months) to make valid conclusions. (2) The sample sizes of the included studies are small and many do not have control groups. This questions whether the study was adequately powered to fully assess all the intended outcomes. (3) Patient demographic data was heterogeneous and may lead to conflicting results. In some studies, good outcomes were reported and a 100 % fusion rate was achieved by the 1-year follow-up. However, in other studies, there was a high reoperation rate that led the authors to recommend against PEEK rods. These contradictory reports can potentially be ascribed to differences between patient groups. (4) Different surgery methods exist, such as pedicle-screw-based anterior interbody fusions, posterolateral fusions, pedicle screw fixation without fusion, and revision surgery. The parameters evaluating the use of PEEK in these cases may vary.
Conclusions
In conclusion, PEEK rod systems can be used for semi-rigid fusion for the treatment of degenerative disc disease and mild lumbar spondylolisthesis. Theoretically, PEEK rod systems can improve anterior column load sharing, reduce stress shielding, and promote fusion. Through its improved load sharing and decreased adjacent structure pressure compared with rigid titanium rod systems, PEEK rod systems reduce the symptoms of lower back pain. Clinical data on the use of PEEK rods is scarce. Several low-quality cohort studies showed contradictory results. We were therefore unable to find strong evidence even on early clinical outcomes after spinal fusions with PEEK rods. Larger sample sizes with a better study composition are required to fully validate PEEK rods as a viable fusion adjunct.
References
Abode-Iyamah K, Kim SB, Grosland N, Kumar R, Belirgen M, Lim TH, Torner J, Hitchon PW (2014) Spinal motion and intradiscal pressure measurements before and after lumbar spine instrumentation with titanium or PEEK rods. J Clin Neurosci 21:651–655
Ahn YH, Chen WM, Lee KY, Park KW, Lee SJ (2008) Comparison of the load-sharing characteristics between pedicle-based dynamic and rigid rod devices. Biomed Mater 3
Athanasakopoulos M, Mavrogenis AF, Triantafyllopoulos G, Koufos S, Pneumaticos SG (2013) Posterior spinal fusion using pedicle screws. Orthopedics 36:e951–e957
Battie MC, Videman T, Kaprio J, Gibbons LE, Gill K, Manninen H, Saarela J, Peltonen L (2009) The Twin Spine Study: contributions to a changing view of disc degeneration. Spine J : Off J North Am Spine Soc 9:47–59. doi:10.1016/j.spinee.2008.11.011
Bruner HJ, Guan Y, Yoganandan N, Pintar FA, Maiman DJ, Slivka MA (2010) Biomechanics of polyaryletherketone rod composites and titanium rods for posterior lumbosacral instrumentation: presented at the 2010 Joint Spine Section Meeting—Laboratory Investigation. J Neurosurg Spine 13:766–772
Chamoli U, Diwan AD, Tsafnat N (2014) Pedicle screw-based posterior dynamic stabilizers for degenerative spine: in vitro biomechanical testing and clinical outcomes. J Biomed Mater Res A 102:3324–3340. doi:10.1002/jbm.a.34986
Chang TK, Huang CH, Liu YC, Chen WC, McClean CJ, Lai YS, Cheng CK (2013) Biomechanical evaluation and comparison of polyetheretherketone rod system to traditional titanium rod fixation on adjacent levels. Formosan J Musculoskelet Disord 4:42–47
Chou D, Lau D, Skelly A, Ecker E (2011) Dynamic stabilization versus fusion for treatment of degenerative spine conditions. Evidence-Based Spine-Care J 2:33–42. doi:10.1055/s-0030-1267111
Chou WK, Chien A, Wang JL (2014) Biomechanical analysis between PEEK and titanium screw-rods spinal construct subjected to fatigue loading. J Spinal Disord Tech
Colangeli S, Barbanti Brodano G, Gasbarrini A, Bandiera S, Mesfin A, Griffoni C, Boriani S (2015) Polyetheretherketone (PEEK) rods: short-term results in lumbar spine degenerative disease. J Neurosurg Sci 59:91–96
De Iure F, Bosco G, Cappuccio M, Paderni S, Amendola L (2012) Posterior lumbar fusion by peek rods in degenerative spine: preliminary report on 30 cases. Eur Spine J 21:S50–S54
Fritzell P, Hagg O, Nordwall A (2003) Complications in lumbar fusion surgery for chronic low back pain: comparison of three surgical techniques used in a prospective randomized study. A report from the Swedish Lumbar Spine Study Group. Eur Spine J : Off Publ Eur Spine Soc Eur Spinal Deformity Soc Eur Section Cervical Spine Res Soc 12:178–189. doi:10.1007/s00586-002-0493-8
Frost HM (1994) Wolff’s Law and bone’s structural adaptations to mechanical usage: an overview for clinicians. Angle Orthod 64:175–188. doi:10.1043/0003-3219(1994)064<0175:WLABSA>2.0.CO;2
Galbusera F, Bellini CM, Anasetti F, Ciavarro C, Lovi A, Brayda-Bruno M (2011) Rigid and flexible spinal stabilization devices: a biomechanical comparison. Med Eng Phys 33:490–496
Gornet MF, Chan FW, Coleman JC, Murrell B, Nockels RP, Taylor BA, Lanman TH, Ochoa JA (2011) Biomechanical assessment of a PEEK rod system for semi-rigid fixation of lumbar fusion constructs. J Biomech Eng 133
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schunemann HJ (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336:924–926. doi:10.1136/bmj.39489.470347.AD
Heo DH, Cho YJ, Cho SM, Choi HC, Kang SH (2012) Adjacent segment degeneration after lumbar dynamic stabilization using pedicle screws and a nitinol spring rod system with 2-year minimum follow-up. J Spinal Disord Tech 25:409–414. doi:10.1097/BSD.0b013e318231665d
Highsmith JM, Tumialan LM, Rodts GE, Jr. (2007) Flexible rods and the case for dynamic stabilization. Neurosurg Focus 22
Huang W, Chang Z, Song R, Zhou K, Yu X (2016) Non-fusion procedure using PEEK rod systems for lumbar degenerative diseases: clinical experience with a 2-year follow-up. BMC Musculoskelet Disord 17:53. doi:10.1186/s12891-016-0913-2
Jahng TA, Kim YE, Moon KY (2013) Comparison of the biomechanical effect of pedicle-based dynamic stabilization: a study using finite element analysis. Spine J 13:85–94
Jin YJ, Kim YE, Seo JH, Choi HW, Jahng TA (2013) Effects of rod stiffness and fusion mass on the adjacent segments after floating mono-segmental fusion: a study using finite element analysis. Eur Spine J 22:1066–1077
Kanayama M, Togawa D, Hashimoto T, Shigenobu K, Oha F (2009) Motion-preserving surgery can prevent early breakdown of adjacent segments: comparison of posterior dynamic stabilization with spinal fusion. J Spinal Disord Tech 22:463–467. doi:10.1097/BSD.0b013e3181934512
Kelly MP, Mok JM, Berven S (2010) Dynamic constructs for spinal fusion: an evidence-based review. Orthop Clin North Am 41:203–215. doi:10.1016/j.ocl.2009.12.004
Kumar A, Beastall J, Hughes J, Karadimas EJ, Nicol M, Smith F, Wardlaw D (2008) Disc changes in the bridged and adjacent segments after Dynesys dynamic stabilization system after two years. Spine 33:2909–2914. doi:10.1097/BRS.0b013e31818bdca7
Kurtz SM (2011) PEEK biomaterials handbook. Applications of polyaryletheretherketone in spinal implants. William Andrew
Kurtz SM, Lanman TH, Higgs G, MacDonald DW, Berven SH, Isaza JE, Phillips E, Steinbeck MJ (2013) Retrieval analysis of PEEK rods for posterior fusion and motion preservation. Eur Spine J 22:2752–2759
Lee MJ, Dettori JR, Standaert CJ, Ely CG, Chapman JR (2012) Indication for spinal fusion and the risk of adjacent segment pathology: does reason for fusion affect risk? A systematic review. Spine 37:S40–51. doi:10.1097/BRS.0b013e31826ca9b1
Lehmann TR, Spratt KF, Tozzi JE, Weinstein JN, Reinarz SJ, El-Khoury GY, Colby H (1987) Long-term follow-up of lower lumbar fusion patients. Spine 12:97–104
Liao Z, Chen W, Wang Z-H, Wei H-W (2015) Clinical study of a new transpedicular nonfusion posterior dynamic stabilization system for treating herniated lumbar intervertebral disks. Neurosurg Q 25:4
Lin HM, Pan YN, Liu CL, Huang LY, Huang CH, Chen CS (2013) Biomechanical comparison of the K-ROD and Dynesys dynamic spinal fixator systems—a finite element analysis. Bio-med Mater Eng 23:495–505. doi:10.3233/BME-130766
Mavrogenis AF, Vottis C, Triantafyllopoulos G, Papagelopoulos PJ, Pneumaticos SG (2014) PEEK rod systems for the spine. Eur J Orthop Surg Traumatol 24:S111–S116
Mulholland RC, Sengupta DK (2002) Rationale, principles and experimental evaluation of the concept of soft stabilization. Eur Spine J : Off Publ Eur Spine Soc Eur Spinal Deformity Soc Eur Section Cervical Spine Res Soc 11(Suppl 2):S198–205. doi:10.1007/s00586-002-0422-x
Nockels RP (2005) Dynamic stabilization in the surgical management of painful lumbar spinal disorders. Spine 30:S68–72
Norvell DC, Dettori JR, Skelly AC, Riew KD, Chapman JR, Anderson PA (2012) Methodology for the systematic reviews on an adjacent segment pathology. Spine 37:S10–17. doi:10.1097/BRS.0b013e31826cd9c8
Ormond DR, Albert Jr L, Das K (2012) Polyetheretherketone (PEEK) rods in lumbar spine degenerative disease: a case series. J Spinal Disord Tech
Ponnappan RK, Serhan H, Zarda B, Patel R, Albert T, Vaccaro AR (2009) Biomechanical evaluation and comparison of polyetheretherketone rod system to traditional titanium rod fixation. Spine J 9:263–267
Qi L, Li M, Zhang S, Xue J, Si H (2013) Comparative effectiveness of PEEK rods versus titanium alloy rods in lumbar fusion: a preliminary report. Acta Neurochir 155:1187–1193
Radcliff KE, Kepler CK, Jakoi A, Sidhu GS, Rihn J, Vaccaro AR, Albert TJ, Hilibrand AS (2013) Adjacent segment disease in the lumbar spine following different treatment interventions. Spine J : Off J North Am Spine Soc 13:1339–1349. doi:10.1016/j.spinee.2013.03.020
Sengupta DK, Bucklen B, McAfee PC, Nichols J, Angara R, Khalil S (2013) The comprehensive biomechanics and load-sharing of semirigid PEEK and semirigid posterior dynamic stabilization systems. Adv Orthop 745610:4
Shih K-S, Hsu C-C, Zhou S-Y, Hou S-M (2015) Biomechanical investigation of pedicle screw-based posterior stabilization systems for the treatment of lumbar degenerative disc disease using finite element analyses. Biomed Eng - Appl Basis Commun 27
Turner JL, Paller DJ, Murrell CB (2010) The mechanical effect of commercially pure titanium and polyetheretherketone rods on spinal implants at the operative and adjacent levels. Spine 35:E1076–E1082
Vieweg; U, Grochulla F (2012) Manual of spine surgery. Posterior lumbar interbody fusion with an interbody fusion spacer or cage. Springer
Wang CJ, Graf H, Wei HW (2014) Clinical outcomes of the dynamic lumbar pedicle screw-rod stabilization: 2-year follow-up results. Neurosurg Q
Wang JC, Arnold PM, Hermsmeyer JT, Norvell DC (2012) Do lumbar motion preserving devices reduce the risk of adjacent segment pathology compared with fusion surgery? A systematic review. Spine 37:S133–143. doi:10.1097/BRS.0b013e31826cadf2
Williams FM, Sambrook PN (2011) Neck and back pain and intervertebral disc degeneration: role of occupational factors. Best Pract Res Clin Rheumatol 25:69–79. doi:10.1016/j.berh.2011.01.007
Wright JG, Swiontkowski MF, Heckman JD (2003) Introducing levels of evidence to the journal. J Bone Joint Surg Am 85-A:1–3
Yang M, Li C, Chen Z, Bai Y, Li M (2014) Short term outcome of posterior dynamic stabilization system in degenerative lumbar diseases. Indian J Orthop 48:574–581. doi:10.4103/0019-5413.144222
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
None of the authors received financial support for this study.
Additional information
Strength of recommendation
Low (due to the majority of clinical studies being level III or below)
Rights and permissions
About this article
Cite this article
Li, C., Liu, L., Shi, JY. et al. Clinical and biomechanical researches of polyetheretherketone (PEEK) rods for semi-rigid lumbar fusion: a systematic review. Neurosurg Rev 41, 375–389 (2018). https://doi.org/10.1007/s10143-016-0763-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-016-0763-2