Abstract
Purpose
Intractable upper limb and neck pain has traditionally been a challenging pain condition to treat, with conventional spinal cord stimulation (SCS) often inducing positional variation in paraesthesia and/or inadequate coverage of axial neck pain. The purpose of this Australian multi-centre prospective, clinical trial was to assess the safety and effectiveness of paraesthesia-independent 10 kHz SCS for the treatment of upper limb and neck pain.
Methods
Subjects with chronic, intractable neck and/or upper limb pain of ≥ 5 cm (on a 0–10-cm visual analogue scale) were enrolled (ACTRN12614000153617) following human research ethics committee approval. Subjects were implanted with two epidural leads spanning C2–C6 vertebral bodies. Subjects with successful trial stimulation were implanted with a Senza® system (Nevro Corp., Redwood City, CA, USA) and included in the safety and effectiveness evaluation at 3 months post-implant (primary endpoint assessment, PEA) and followed to 12 months.
Results
Overall, 31/38 (82.6%) subjects reported a successful 10 kHz SCS trial and proceeded to a permanent implant. Twenty-three of 30 subjects (76.7%) met the PEA. Subjects reported a reduction in neck pain and upper limb pain from baseline at the PEA (8.1 ± 0.2 cm vs. 2.9 ± 0.5 cm, 7.3 ± 0.3 cm vs. 2.5 ± 0.5 cm, respectively, p ≤ 0.0001). Disability, as measured by pain disability index score, decreased from 42.6 ± 2.6 at baseline to 22.7 ± 3.2 at PEA. Results were maintained 12 months post-implant. No neurological deficits, nor reports of paraesthesia, were observed.
Conclusions
Stable, long-term results demonstrated that 10 kHz SCS is a promising therapy option for intractable chronic upper limb and neck pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Neck pain is ranked as the fourth leading cause of years lost to disability behind back pain, depression and arthralgias [1, 2]. Globally, it is estimated to occur in excess of 30% of the population, with nearly 50% of individuals continuing to experience ongoing pain [1]. There are different manifestations of pain arising from the cervical region, including axial neck pain and upper limb radicular pain [3]. Whilst most cases of axial neck pain resolve within weeks with conservative management, studies have suggested around 10% to 34% of patients have persistent chronic pain [3].
When conservative management is ineffective and neck pain is accompanied by spinal instability, neurological compromise or deformity, surgical intervention may be indicated [3]. There have been few studies that have evaluated surgical procedures for neck pain and even fewer that have evaluated outcomes longer than 2 years post-surgery [1]. Beyond surgery, no other proven treatment options currently exist, and for some, surgery is not expected to alleviate the underlying cause of pain [1].
In patients with persistent or recurrent pain, spinal cord stimulation (SCS) may be a viable treatment option [4]. Whilst SCS has been employed and evaluated extensively for chronic axial and radicular back pain, the practicality of the technique in the cervical region has been limited, with a small number of studies highlight promising effects on both pain relief, disability and patient satisfaction following the use of traditional SCS in patients with cervical origin pain [2, 4,5,6,7,8,9]. Despite this, the propensity for electrode dislodgement and variability in the distribution of cervical pain compared with back and lower limb pain has limited its widespread use [10]. Further, traditional SCS, a stimulation that produces a tingling sensation known as paraesthesia in an attempt to mask the painful sensation, has limitations in the cervical region with the paraesthesia itself being an unpleasant sensation for some patients [11]. In addition, creating the ideal paraesthesia coverage can be challenging and even more difficult in the highly mobile cervical region, as paraesthesia intensity can increase or decrease with body movement [12].
However, a newer modality of SCS has an established body of long-term evidence in back and leg pain. High-frequency SCS at 10,000 Hz (10 kHz SCS) applies a unique waveform, providing pain relief superior to traditional SCS without any paraesthesia and demonstrated improvements in quality of life and functionality, maintained up to 2 years post-implant [13,14,15]. This is of particular interest in pain originating from the cervical region as positional variation may not be an issue with 10 kHz SCS.
In upper limb and neck pain, the application of 10 kHz SCS has been previously examined in 36 cases from a retrospective Australian study of intractable pain conditions [12]. In patients with neck pain with or without arm/shoulder pain who underwent permanent implantation (n = 11), significant pain reductions were reported at 6 months [12]. Further evidence for patient satisfaction following the application of 10 kHz SCS in the cervical region has been reported in a small subgroup of patients. Three-quarters (75%) reported satisfaction after permanent implantation of the 10 kHz SCS system in the cervical region [13].
High-quality prospective studies that stratify patients based on their cervical axial and radicular components are needed to improve our understanding of the application of 10 kHz SCS in cervical axial and radicular pain [4]. Therefore, the aim of this study was to assess the safety and effectiveness of 10 kHz SCS in a cohort of subjects with chronic, intractable pain of the upper limb and/or neck.
Methods
This study was a prospective, multi-centre study assessing the safety and effectiveness to 10 kHz SCS therapy without stimulation-related neurological deficit in adult subjects with chronic, intractable pain of the upper limb and/or neck.
Patients
Subjects meeting the inclusion and exclusion criteria were eligible for inclusion in this study (Table 1). Study sites submitted redacted medical records and flexion–extension images of the cervical spine to two independent medical monitors to confirm enrolment eligibility.
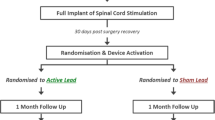
The protocol was listed on the Australian New Zealand Clinical Trial Registry (ACTRN12614000153617) and received Human Research Ethics Committee (HREC) approval from Bellberry Limited (Application Number: 2013-10-560). Subjects were recruited from three centres in Australia and consented prior to any study procedures. A flow chart of study design and enrolment is presented in Fig. 1.
Procedure
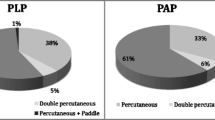
Thirty-eight subjects completed a trial stimulation phase with 10 kHz SCS (Senza System, Nevro Corp., Redwood City, CA, USA) of up to 14 days with an external stimulator to determine their short-term response. Under fluoroscopy and sterile conditions, two octapolar leads were placed in a staggered fashion into the epidural space at the anatomical midline of the cervical spine spanning C2 to C6 vertebral levels to deliver 10 kHz SCS (Fig. 2). Sites were permitted to use their standard clinical practice for performing the trial procedures, including either staged trials [8] or temporary trials [9], as previously described. Subjects who experienced at least 40% reduction in their neck and/or upper limb pain during the trial compared to baseline were eligible for permanent device implantation. For permanent implantation, leads were placed as detailed above and connected to a subcutaneously placed implantable pulse generator (IPG). The leads, anchored to the supraspinous ligaments, were tunnelled to the IPG site in the axillary, flank or buttock region for connection and tested to ensure electrical integrity before closure. SCS was delivered at 10 kHz frequency, 30 μs pulse width, and amplitudes adjusted to maximise individual subject’s pain relief.
Follow-up
Subjects were assessed at baseline and at 1, 3, 6, 9 and 12 months after permanent implantation. At each visit, subjects were assessed for change in pain according to the 10-cm VAS, disability using Pain Disability Index (PDI) [16] and pain experience using Short-Form McGill Pain Questionnaire (SFMPQ2) [17]. Effects on quality of life were assessed using the Short Form-12 (SF-12) questionnaire [18], Clinician Global Impression of Change (CGIC) and Patient Global Impression of Change (PGIC) instruments [19]. Effect on depression was measured by Beck Depression Inventory (BDI) [20] and sleep disturbance by Pittsburgh Sleep Quality Index (PSQI) [21]. Change from baseline in opioid medication usage and adverse events were also recorded at every visit.
Per protocol population (PPP)
The intent-to-treat (ITT) population was defined as all subjects who received a permanent device implant. PPP was defined as subjects who had a successful SCS trial, received an IPG implant, had their device activated and had 3-month primary endpoint assessment post-permanent implant. The primary endpoint of the proportion of responders (defined as subjects with ≥ 50% pain relief from baseline) without a stimulation-related neurological deficit was assessed at 3 months in PPP and at follow-up visits.
Statistical analyses
Descriptive analysis of continuous variables included mean and standard error (SEM), or median as appropriate. Categorical variables were reported as counts and percentages where possible. All data were analysed as-observed and outcomes reported through descriptive statistics. Two-tailed paired t test was used to compare the means, and a p value < 0.05 was considered as significant.
Results
Baseline characteristics
Baseline demographics and clinical characteristics of the subjects enrolled in the study are shown in Table 2. The mean age at the time of enrolment was 53.0 ± 2.3 years, 41.9% were female, the mean time since diagnosis was 10.1 ± 1.3 years, and 35.5% of enrolled subjects had previously undergone surgery of the cervical spine. Subjects with a history of spinal instability and/or progressive neurological deficits were evaluated and treated if indicated as part of their standard of care, prior to enrolling in this study. Subjects cleared for SCS continuing to experience neck and/or upper limb pain were enrolled in the study.
Trial success rates
Trial success was defined as pain relief of ≥ 40% compared to baseline as measured by VAS scores. Majority of the subjects (81.5%) had a successful trial. In subjects with VAS with ≥ 5 cm, 80.0% (28/35) and 94.7% (18/19) with neck pain and upper limb pain, respectively, were trial stimulation responders.
Safety and adverse events
The mean length of study participation for the permanently implanted subjects was 54.5 weeks (range: 40.0–76.6 weeks). Subjects were assessed for possible neurological deficits and other safety events compared with their baseline state. Overall, no stimulation-related neurological deficits were reported, with neurological assessments reporting “No Change” or “Improvement” in neurological function at PEA. Study-related adverse events (AEs) were reported in 12 (30.8%) subjects, categorised as mild or moderate, with all events resolved prior to study exit at 12 months (Table 3). One study-related serious adverse event was reported in 1 (2.6%) subject, a medical device site infection, which resolved with treatment. There were no stimulation-related, unanticipated or device-related serious adverse events recorded for the study.
Pain relief
The baseline average score for neck pain was 8.1 ± 0.2 cm and for upper limb pain was 7.3 ± 0.3 cm, which were reduced to 2.9 ± 0.5 cm (p ≤ 0.0001) and 2.5 ± 0.5 cm (p ≤ 0.0001), respectively, at 3 months and maintained to 12 months (Fig. 3). Average reduction in neck and upper limb pain was 65.2% and 66.0%, respectively, at 3 months. The improvement was sustained at 6 months (64.3% and 66.3%, respectively) and improved further at 12-month endpoint assessment (74.2% and 61.8%, respectively).
Responder and remitter rates
Responders were subjects who had ≥ 50% pain relief. At 3 months, 64.3% of subjects with neck pain (18/28) had ≥ 50% pain relief, which increased to 85.2% (23/27) by 12 months. In subjects with upper limb pain, 77.8% at 3 months (14/18) and 76.5% (13/17) at 12 months reported ≥ 50% pain relief (Fig. 3).
Subjects with VAS scores ≤ 3.0 cm were defined as remitters [22]. At 3 months, 57.1% of subjects with neck pain (16/28) had pain remission, which increased to 71.4% of subjects (20/27) by 12 months. In subjects with upper limb pain, 66.6% at 3 months (12/18) and 64.7% (11/17) at 12 months were categorised as remitters.
Subjects also reported reduced SFMPQ2 scores over time in all sub-scales (Fig. 4) and had a mean total score decrease from baseline varying between 2.3 and 2.5 through month 12 (Table 4).
Functional improvement
Effect of 10 kHz SCS treatment on improvement in function was assessed using the PDI. The mean functional disability improved from 42.6 ± 2.6 at baseline to 22.7 ± 3.2 at 3 months, indicating a lesser level of disability by 19.9 ± 3.1 points, twice the minimal clinically important difference (MCID) of 8.5 to 9.5 points [23]. Subjects showed durability of PDI improvement over time, reporting a sustained PDI of 21.2 ± 3.4 at 12 months (Fig. 5).
Quality of life and medication use
Effect of 10 kHz SCS treatment on quality of life was assessed using multiple questionnaires including SF-12 quality of life, BDI, PSQI and GAF. Table 4 shows subjects reported significant improvements in all quality-of-life assessments at 3 months and sustained improvements through 12 months post-implantation.
At 3, 6 and 12 months, 41.7% of patients (10/24), 45.8% (11/24) and 58.3% (14/24) were able to decrease or eliminate concomitant opioid medications, respectively.
Patient and clinician impression of change and satisfaction
At 3 months, subjects reporting PGIC as ‘a great deal better’, ‘better’ and ‘moderately better’ were 61.3%, which increased at 12-month endpoint assessment to 82.8% (Table 5). Similarly, clinicians reporting GIC as ‘a great deal better’, ‘better’ and ‘moderately better’ were 83.8% at 3 months, which increased to 89.7% at 12-month endpoint assessment.
Patient satisfaction was positively rated in 67.7% and 75.9% of subjects at the 3- and 12-month endpoints, respectively (Fig. 5).
Discussion
This prospective trial of 10 kHz SCS in Australian subjects with chronic, intractable neck and upper limb pain confirms the safety and efficacy of this therapy in the cervical region. Importantly, despite historical complications such as electrode migration and incomplete paraesthesia with traditional SCS, this study confirms that the safety of 10 kHz SCS in the cervical region is similar to the profile reported previously in the thoracic region. In the current study, neurological assessment revealed no stimulation or electrode placement-related neurological deficits. Similar rates of serious and non-serious study-related AEs were reported in the current study as compared with previous reports of 10 kHz SCS and traditional SCS, suggesting that the former does not induce any new complications [14, 24].
Significant pain relief was achieved with 10 kHz SCS for both neck and upper limb pain. Subjects reported significant improvements in pain scores at the end of the stimulation trial, maintained through to 12 months. Pain reduction translated into improved functional and quality of life scores, assessed across numerous assessments and at all time points. Given the subjects in this study have suffered from chronic pain for 10 years on an average, and other interventions had failed to relieve their pain, their baseline PDI was moderately high (42.6 out of 70). The application of 10 kHz SCS enabled clinically meaningful pain relief to an extent where they reported improved daily function out to 12 months. Given neck and upper limb pain is considered to be disabling to the extent at which work and everyday activities may be affected, 10 kHz SCS has the potential to reduce the disability-related impact of cervical-related pain. Here, a majority of subjects were satisfied with the outcome of therapy and more than half were able to decrease or cease opioid medications. In the light of the current opioid crisis, the latter signifies an important step towards successful non-opioid management of chronic pain.
The current study implies better pain relief reported in previous traditional SCS studies, where the average pain reduction for cervical spine conditions ranged from 22.8 to 66.8%, though the origin of pain was not always noted across all studies [4]. Also notable, the amount of pain relief with 10 kHz SCS was achieved without paraesthesia. Whilst a few previous traditional SCS studies also investigated impact on quality of life, no study was as thorough in demonstrating the improvement with SCS as the current study.
There is now consistent evidence for 10 kHz SCS across diverse chronic, intractable pain conditions [8, 13,14,15, 22, 25]. Regardless of the anatomical lead placement, significant reductions in pain are observed and sustained over the longer term.
It is important to note that this study is early data on cervical 10 kHz SCS. Previous studies in cervical SCS in particular often failed to distinguish between pain aetiologies. Alike the evolution of surgical interventions for cervical axial pain and SCS itself, improvements in technique and patient selection from this study is expected to help yield improved outcomes in future studies.
Main limitations of the study include lack of a control group and randomisation of subjects. The possible selection bias by the investigators which could have resulted from lack of randomisation was minimised by involvement of independent medical monitors and high level of diligence in the selection of subjects meeting the inclusion and exclusion criteria. Lack of control group in the study was addressed by estimating the effect size from efficacy of 10 kHz SCS, documented in previously completed randomised controlled trial and in large real-world retrospective review [14, 25]. Further investigations may address the impact of prior surgeries, comorbidities and concurrent healthcare utilisation, which were not built into the study design of this current study.
Conclusion
This Australian neck and upper limb study demonstrates the utility of 10 kHz SCS to cervical axial pain conditions. Over the 12-month follow-up, 10 kHz SCS in the cervical region was well tolerated, with a similar safety profile to lumbar electrode placement. A majority of subjects reported significant upper limb and neck pain relief that conferred improvements in function and quality of life. Both patients and clinicians were satisfied with treatment at the 12-month visit. Overall, the study highlights that 10 kHz SCS is a legitimate paraesthesia-independent treatment option for patients with chronic, intractable cervical axial pain.
References
Cohen SP (2015) Epidemiology, diagnosis, and treatment of neck pain. Mayo Clin Proc 90(2):284–299. https://doi.org/10.1016/j.mayocp.2014.09.008
Vallejo R, Kramer J, Benyamin R (2007) Neuromodulation of the cervical spinal cord in the treatment of chronic intractable neck and upper extremity pain: a case series and review of the literature. Pain Phys 10(2):305–311
Clarke MJ, Schiefer TK, Pichelmann MA, Krauss WE (2011) Axial neck pain: a surgeon’s perspective. Therapy 8(6):763–770
Provenzano DA, Amirdelfan K, Kapural L, Sitzman BT (2017) Evidence gaps in the use of spinal cord stimulation for treating chronic spine conditions. Spine 42(Suppl 14):S80–S92. https://doi.org/10.1097/brs.0000000000002184
Deer TR, Mekhail N, Provenzano D, Pope J, Krames E, Leong M, Levy RM, Abejon D, Buchser E, Burton A, Buvanendran A, Candido K, Caraway D, Cousins M, DeJongste M, Diwan S, Eldabe S, Gatzinsky K, Foreman RD, Hayek S, Kim P, Kinfe T, Kloth D, Kumar K, Rizvi S, Lad SP, Liem L, Linderoth B, Mackey S, McDowell G, McRoberts P, Poree L, Prager J, Raso L, Rauck R, Russo M, Simpson B, Slavin K, Staats P, Stanton-Hicks M, Verrills P, Wellington J, Williams K, North R, Neuromodulation Appropriateness Consensus C (2014) The appropriate use of neurostimulation of the spinal cord and peripheral nervous system for the treatment of chronic pain and ischemic diseases: the Neuromodulation Appropriateness Consensus Committee. Neuromodulation 17(6):515–550. https://doi.org/10.1111/ner.12208discussion 550
Haider N, Ligham D, Quave B, Harum KE, Garcia EA, Gilmore CA, Miller N, Moore GA, Bains A, Lechleiter K, Jain R (2018) Spinal cord stimulation (SCS) trial outcomes after conversion to a multiple waveform SCS system. Neuromodulation 21(5):504–507. https://doi.org/10.1111/ner.12783
Hunter CW, Carlson J, Yang A, Deer T (2018) Spinal cord stimulation for the treatment of failed neck surgery syndrome: outcome of a prospective case series. Neuromodulation 21(5):495–503. https://doi.org/10.1111/ner.12769
Salmon J (2019) High-frequency spinal cord stimulation at 10 kHz for widespread pain: a retrospective survey of outcomes from combined cervical and thoracic electrode placements. Postgrad Med 131(3):230–238. https://doi.org/10.1080/00325481.2019.1587564
Amirdelfan K, Vallejo R, Benyamin R, Yu C, Yang T, Bundschu R, Yearwood TL, Sitzman BT, Gliner B, Subbaroyan J, Rotte A, Caraway D (2019) High-frequency spinal cord stimulation at 10 kHz for the treatment of combined neck and arm pain: results from a prospective multicenter study. Neurosurgery. https://doi.org/10.1093/neuros/nyz495
Simpson BA, Bassett G, Davies K, Herbert C, Pierri M (2003) Cervical spinal cord stimulation for pain: a report on 41 patients. Neuromodulation 6(1):20–26. https://doi.org/10.1046/j.1525-1403.2003.03003.x
Jang HD, Kim MS, Chang CH, Kim SW, Kim OL, Kim SH (2008) Analysis of failed spinal cord stimulation trials in the treatment of intractable chronic pain. J Korean Neurosurg Soc 43(2):85–89. https://doi.org/10.3340/jkns.2008.43.2.85
Russo M, Van Buyten JP (2015) 10-kHz high-frequency SCS therapy: a clinical summary. Pain Med 16(5):934–942. https://doi.org/10.1111/pme.12617
Al-Kaisy A, Palmisani S, Smith T, Harris S, Pang D (2015) The use of 10-kilohertz spinal cord stimulation in a cohort of patients with chronic neuropathic limb pain refractory to medical management. Neuromodulation 18(1):18–23. https://doi.org/10.1111/ner.12237discussion 23
Kapural L, Yu C, Doust MW, Gliner BE, Vallejo R, Sitzman BT, Amirdelfan K, Morgan DM, Brown LL, Yearwood TL, Bundschu R, Burton AW, Yang T, Benyamin R, Burgher AH (2015) Novel 10-kHz high-frequency therapy (HF10 therapy) is superior to traditional low-frequency spinal cord stimulation for the treatment of chronic back and leg pain: the SENZA-RCT randomized controlled trial. Anesthesiology 123(4):851–860. https://doi.org/10.1097/ALN.0000000000000774
Amirdelfan K, Yu C, Doust MW, Gliner BE, Morgan DM, Kapural L, Vallejo R, Sitzman BT, Yearwood TL, Bundschu R, Yang T, Benyamin R, Burgher AH, Brooks ES, Powell AA, Subbaroyan J (2018) Long-term quality of life improvement for chronic intractable back and leg pain patients using spinal cord stimulation: 12-month results from the SENZA-RCT. Qual Life Res 27(8):2035–2044. https://doi.org/10.1007/s11136-018-1890-8
Tait RC, Chibnall JT, Krause S (1990) The pain disability index: psychometric properties. Pain 40(2):171–182
Dworkin RH, Turk DC, Revicki DA, Harding G, Coyne KS, Peirce-Sandner S, Bhagwat D, Everton D, Burke LB, Cowan P, Farrar JT, Hertz S, Max MB, Rappaport BA, Melzack R (2009) Development and initial validation of an expanded and revised version of the Short-form McGill Pain Questionnaire (SF-MPQ-2). Pain 144(1–2):35–42. https://doi.org/10.1016/j.pain.2009.02.007
Jenkinson C, Layte R, Jenkinson D, Lawrence K, Petersen S, Paice C, Stradling J (1997) A shorter form health survey: can the SF-12 replicate results from the SF-36 in longitudinal studies? J Public Health Med 19(2):179–186
Fischer D, Stewart AL, Bloch DA, Lorig K, Laurent D, Holman H (1999) Capturing the patient’s view of change as a clinical outcome measure. JAMA 282(12):1157–1162
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J (1961) An inventory for measuring depression. Arch Gen Psychiatry 4:561–571
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213
Amirdelfan K, Gliner BE, Kapural L, Sitzman BT, Vallejo R, Yu C, Caraway D, Rotte A, Province-Azalde R, Krames E (2019) A proposed definition of remission from chronic pain, based on retrospective evaluation of 24-month outcomes with spinal cord stimulation. Postgrad Med 131(4):278–286. https://doi.org/10.1080/00325481.2019.1592401
Soer R, Reneman MF, Vroomen PC, Stegeman P, Coppes MH (2012) Responsiveness and minimal clinically important change of the Pain Disability Index in patients with chronic back pain. Spine 37(8):711–715. https://doi.org/10.1097/brs.0b013e31822c8a7a
Eldabe S, Buchser E, Duarte RV (2016) Complications of spinal cord stimulation and peripheral nerve stimulation techniques: a review of the literature. Pain Med 17(2):325–336. https://doi.org/10.1093/pm/pnv025
Stauss T, El Majdoub F, Sayed D, Surges G, Rosenberg WS, Kapural L, Bundschu R, Lalkhen A, Patel N, Gliner B, Subbaroyan J, Rotte A, Edgar DR, Bettag M, Maarouf M (2019) A multicenter real-world review of 10 kHz SCS outcomes for treatment of chronic trunk and/or limb pain. Ann Clin Transl Neurol 6(3):496–507. https://doi.org/10.1002/acn3.720
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The study was sponsored by Nevro Corp. Drs Verrills, Russo and Salmon are consultants to Nevro Corp. Mr Gliner, Barnard and Caraway are employees of Nevro Corp.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Verrills, P., Salmon, J., Russo, M. et al. 10 kHz spinal cord stimulation for chronic upper limb and neck pain: Australian experience. Eur Spine J 29, 2786–2794 (2020). https://doi.org/10.1007/s00586-020-06480-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06480-x