Abstract
Study design
Retrospective cohort study.
Objective
Assess the outcomes of final fusion in early onset scoliosis patients treated with TDGR, particularly with acceptable coronal and sagittal alignment at the end of their growing age.
Summary of background data
Early onset scoliosis (EOS) poses challenges due to the need for managing spinal deformities while accommodating trunk growth. The dual growing rod (TDGR) technique, a traditional approach, aims to address these concerns by periodic lengthening until spinal growth ceases. Recent shifts propose observation without immediate implant removal after achieving spinal alignment, raising questions about the necessity of final fusion surgery.
Methods
This retrospective study included 22 EOS patients treated with TDGR who underwent final fusion surgery. Clinical and radiological data were analyzed, including pre- and post-surgery measurements, complications, surgical approaches, and screw density.
Results
Patients (average initial surgery age: 6.9 years) exhibited significant reductions in main curve angle (preoperative: 65.8°, pre-fusion: 49.1°, post-fusion: 36.3°) and thoracic kyphosis (preoperative: 47°, pre-fusion: 46.6°, post-fusion: 38.7°). Complications included one surgical site infection and four transient intraoperative neuro-monitoring Impairment. High screw density correlated with lower total correction.
Conclusion
Final fusion surgery post-TDGR treatment shows promise in correcting EOS-associated deformities. Surgeons and parents should be aware of the procedure’s complexity and potential complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Early onset scoliosis (EOS) is characterized by scoliosis onset before the age of 10 years [1]. While spinal fusion garnered interest in the past, recent research has illuminated its adverse effects on cosmetic appearance and pulmonary function in patients younger than 7 years old [2,3,4,5,6]. Addressing EOS remains challenging as corrective measures must accommodate ongoing trunk growth [7]. Non-fusion techniques aim to support trunk growth while halting or improving spinal deformities in the coronal and sagittal planes [8]. The traditional dual growing rod (DTGR) method, pioneered by Akbarnia et al., establishes a foundation using screws, hooks, or a combination of both at proximal and distal points for fixation. Rods are interconnected with a connector, and periodic lengthening, typically every 6 months, continues until spinal growth or thoracic development plateaus or no further distraction is achievable. Subsequently, patients undergo final fusion surgery involving growing rod removal, necessary deformity correction, and posterior fusion with instrumentation [9,10,11,12]. Recent studies highlight a potential paradigm shift in EOS treatment. Patients treated with growing rods, achieving proper spinal alignment, acceptable trunk height, and without device-related complications, may now be considered for observation without immediate implant removal and final fusion [7]. This potential shift holds promise for patients and healthcare systems. Given the limited research in this area, our study aims to assess the outcomes of final fusion in early onset scoliosis patients treated with TDGR, particularly with acceptable coronal and sagittal alignment at the end of their growing age.
Material and methods
This retrospective cohort study commenced following the approval of our institute’s Ethics Committee. The study encompassed all patients diagnosed with early onset scoliosis, who received treatment with TDGR and subsequently underwent final fusion surgery. Inclusion criteria comprised individuals aged below 10 at diagnosis, absence of prior spine surgery, initial treatment involving TDGR, and subsequent final fusion surgery upon skeletal maturity with at least 2-year follow-up. Exclusion criteria involved the application of growth friendly devices other than TDGR, unavailability of pre- or post-operative radiographs, limited access to patients’ clinical records, or failure to meet any of the inclusion criteria. Ultimately, 22 eligible patients meeting these criteria were included in the study.
Data retrieved from patient records encompassed pre- and post-surgery age, scoliosis type (Congenital, idiopathic, neuromuscular, and syndromic), surgical complications (attributed to growing rods pre-fusion and to final fusion post-fusion), frequency of rod lengthening procedures, and the surgical approach (posterior or combined anterior–posterior) for final fusion. Any complication related to final fusion surgery was extracted and recorded. Neurological complications were defined as a decrease or absence of motor evoked potential (MEP) during intraoperative neuro-monitoring or intraoperative Stagnara wake-up test. Radiological parameters, including primary curvature magnitude, cervical lordosis, and thoracic kyphosis, were measured via the Cobb’s method on radiographs. These measurements were conducted at three intervals: pre-initial surgery, pre-final fusion (after the last rod lengthening session), and post-final fusion. The difference in the main curvature before the growing rod surgery and after final fusion was considered the total correction, while the difference before and after final fusion was deemed the final correction. Screw density (SD) served as an assessment parameter for screw insertion difficulty, calculated as the number of screws placed per fusion levels. SD values less than 70% indicated low density.
Descriptive statistics employed mean, standard deviation, median, mode, and frequency. Correlation, t-tests, and Chi-square tests were utilized for data analysis, with significance set at P < 0.05.
Results
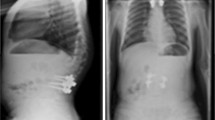
A total of 22 patients diagnosed with early onset scoliosis (EOS), including seven idiopathic, 10 congenital, four syndromic, and one neuromuscular curve type, underwent final fusion surgery subsequent to growing rod treatment at our referral spine surgery center between 2000 and 2020. The average age at the initial surgery was 6.9 years (range 4–9), while the mean age at the time of final fusion stood at 12.6 years. Preoperative, pre-final fusion, and post-final fusion measurements of the main curve angle were 65.8 ± 17.6, 49.1 ± 21.6, and 36.3 ± 22.2 degrees, respectively. These findings indicate a significant reduction in curve magnitude following both growing rod treatment and final fusion (Fig. 1). Similarly, thoracic kyphosis angle correction was observed after final fusion, whereas cervical lordosis angle did not show substantial improvement (Table 1). Among operated patients, 7 (31.8%) patients were idiopathic EOS, 10 (45.5%) were congenital EOS, 4 (18.2%) were syndromic, and 1 (4.5%) was neuromuscular EOS.
Radiographs illustrating the clinical course of one case. A, B: AP and lateral preoperative radiographs of an 8-year-old boy with idiopathic early onset scoliosis with about 50 degrees Cobbs angle. C, D: The same patient at the age of 11 and after 7 rod lengthening sessions; main curve 30 degrees. E, F: After final fusion; main curve about 5 degrees
On average, patients underwent 7.5 rod lengthening sessions. All final fusion procedures were performed through the posterior approach, and correction was achieved by using screws and multi-Ponte osteotomies. Complications associated with the growing rod included rod breakage (36.4%), hook dislodgment (36.4%), and proximal junctional kyphosis (PJK) (31.8%). Following final fusion, 1 patient (4.5%) experienced a surgical site infection necessitating hospitalization and reoperation involving irrigation and debridement. Four experienced transient intraoperative neuro-monitoring impairment (Table 2).
Evaluating the patients before the final fusion, the study revealed that the mean preoperative main curve magnitude was significantly lower in the group experiencing PJK (P = 0.04). Additionally, in this group, the mean pre-fusion main curve magnitude was also notably lower (P = 0.02). At final fusion, 6 (27.3%) patients had high-density screws while 16 (72.7%) were in group of low-density screws. Within this low-density group, the total correction was found to be lower (P = 0.02), although no significant relationship was observed with the final correction (Table 3).
Discussion
The management of early onset scoliosis (EOS) presents a persistent challenge due to the dual necessity of controlling chest growth while addressing both coronal and sagittal deformities [7]. Presently, the prevailing approach for EOS involves utilizing growing rods and staged distraction, typically conducted at intervals of 6 months until skeletal maturity is achieved, followed by the definitive fusion surgery [11, 13, 14].
This study sought to assess the outcomes of the final fusion surgery, specifically focusing on the correction of coronal and sagittal plane deformities, alongside an evaluation of associated surgical complications. Notably, the primary curve magnitude decreased from 65.8° (preoperative) to 49.1° (pre-fusion), ultimately reaching 36.3 degrees post-fusion. Concurrently, mean thoracic kyphosis exhibited a reduction from 47° (preoperative) to 46.6° (pre-fusion), culminating in 38.7° post-fusion. These findings underscore the effectiveness of final fusion in rectifying scoliosis and thoracic kyphosis.
In a study by Cahill et al., comprising nine EOS patients treated with growing rods followed by final fusion, comparable results were observed, with the mean scoliosis curve decreasing from 72.6° pre-surgery to 24.4° post-fusion. Notably, Cahill et al. reported an 89% incidence of autofusion during final fusion surgery, necessitating multiple osteotomies for correction [15]. Our study accounts the necessity of performing Ponte osteotomy in all cases in order to release autofusion in non-instrumented area of the spine.
Furthermore, Du et al. identified the number of spinal levels involved with the growing rod and the duration of treatment as independent risk factors for reoperation post-final fusion in a study involving 167 patients [16]. In contrast, our study, with a smaller cohort (n = 22), did not find a similar association. Moreover, the rate of surgical site infections (SSI) in our study was 4.5%, with no reported wound complications, akin to Du et al.’s findings. Similarly, Clement et al.’s study involving 26 patients showcased a reduction in main curve magnitude and thoracic kyphosis following final fusion surgery, aligning with our results pre-fusion. However, discrepancies emerged post-fusion in thoracic kyphosis measurements [17].
Nevertheless, limitations such as the retrospective nature of the study, a small sample size, and the absence of a control group emphasize the necessity for future prospective research. Larger cohorts with a control group, including patients not undergoing final fusion surgery, are essential to improve the accuracy of future investigations.
Our study highlights the potential for corrective outcomes through the intricate final fusion surgery in addressing EOS-related deformities treated with TDGR during the patients’ final growth stage. Surgeons and parents of patients should be cognizant of the surgery’s complexity and potential complications.
References
McMaster MJ, Macnicol MF (1979) The management of progressive infantile idiopathic scoliosis. J Bone Jt Surg Br 61(1):36–42. https://doi.org/10.1302/0301-620X.61B1.422633. (PMID: 422633)
Patterson JF, Webb JK, Burwell RG (1990) The operative treatment of progressive early onset scoliosis. A preliminary report. Spine 15(8):809–815 (PMID: 2237631)
Winter RB, Moe JH (1982) The results of spinal arthrodesis for congenital spinal deformity in patients younger than five years old. J Bone Jt Surg Am 64(3):419–432 (PMID: 7061559)
Goldberg CJ, Gillic I, Connaughton O et al (2003) Respiratory function and cosmesis at maturity in infantile-onset scoliosis. Spine 28(20):2397–2406. https://doi.org/10.1097/01.BRS.0000085367.24266.CA. (PMID: 14560091)
Karol LA, Johnston C, Mladenov K et al (2008) Pulmonary function following early thoracic fusion in non-neuromuscular scoliosis. J Bone Jt Surg Am 90(6):1272–1281. https://doi.org/10.2106/JBJS.G.00184. (PMID: 18519321)
Vitale MG, Matsumoto H, Bye MR et al (2008) A retrospective cohort study of pulmonary function, radiographic measures, and quality of life in children with congenital scoliosis: an evaluation of patient outcomes after early spinal fusion. Spine 33(11):1242–1249. https://doi.org/10.1097/BRS.0b013e3181714536. (PMID: 18469699)
Jain A, Sponseller PD, Flynn JM et al (2016) Avoidance of “final” surgical fusion after growing-rod treatment for early-onset scoliosis. J Bone Jt Surg Am 98(13):1073–1078. https://doi.org/10.2106/JBJS.15.01241. (PMID: 27385680)
Poe-Kochert C, Shannon C, Pawelek JB et al (2016) Final fusion after growing-rod treatment for early onset scoliosis: is it really final? J Bone Jt Surg Am 98(22):1913–1917. https://doi.org/10.2106/JBJS.15.01334. (PMID: 27852908)
Akbarnia BA (2007) Management themes in early onset scoliosis. J Bone Jt Surg Am 89(Suppl 1):42–54. https://doi.org/10.2106/JBJS.F.01256. (PMID: 17272422)
Akbarnia BA, Marks DS, Boachie-Adjei O et al (2005) Dual growing rod technique for the treatment of progressive early-onset scoliosis: a multicenter study. Spine 30(17 Suppl):S46–S57. https://doi.org/10.1097/01.brs.0000175190.08134.73. (PMID: 16138066)
Bess S, Akbarnia BA, Thompson GH et al (2010) Complications of growing-rod treatment for early-onset scoliosis: analysis of one hundred and forty patients. J Bone Jt Surg Am 92(15):2533–2543. https://doi.org/10.2106/JBJS.I.01471. (Epub 2010 Oct 1 PMID: 20889912)
Chehrassan M, Nikouei F, Shakeri M et al (2024) Factors related to proximal junctional kyphosis and device failure in patients with early-onset scoliosis treated with a traditional dual growing rod: a single institution study. Asian Spine J 18(2):236–243
Menapace B, Jain V, Sturm P (2024) Autofusion in early-onset scoliosis growing constructs: occurrence, risk factors, and impacts. Spine Deform. https://doi.org/10.1007/s43390-024-00853-8
Ahuja K, Ifthekar S, Mittal S et al (2023) Is final fusion necessary for growing-rod graduates: a systematic review and meta-analysis. Glob Spine J 13(1):209–218
Cahill PJ, Marvil S, Cuddihy L et al (2010) Autofusion in the immature spine treated with growing rods. Spine 35(22):E1199–E1203. https://doi.org/10.1097/BRS.0b013e3181e21b50. (PMID: 20683383)
Du JY, Poe-Kochert C, Thompson GH et al (2020) Risk factors for reoperation following final fusion after the treatment of early-onset scoliosis with traditional growing rods. J Bone Jt Surg Am 102(19):1672–1678. https://doi.org/10.2106/JBJS.20.00312. (PMID: 33027120)
Clement RC, Yaszay B, McClung A et al (2020) Growth-preserving instrumentation in early-onset scoliosis patients with multi-level congenital anomalies. Spine Deform 8(5):1117–1130. https://doi.org/10.1007/s43390-020-00124-2. (PMID: 32451975)
Funding
There is no funding source.
Author information
Authors and Affiliations
Contributions
Mohammadreza Chehrassan made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work; Mohammadreza Shakeri drafted the work or revised it critically for important intellectual content; Farshad Nikouei drafted the work or revised it critically for important intellectual content; Mahdi Yaqubnejad made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work; Ebrahim Ameri Mahabadi approved the version to be published; Hasan Ghandhari Agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chehrassan, M., Shakeri, M., Nikouei, F. et al. Achievements and complications related to final fusion surgery in early onset scoliosis at the end of “traditional dual growing rod mission”. Musculoskelet Surg 108, 333–337 (2024). https://doi.org/10.1007/s12306-024-00829-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-024-00829-x