Abstract
Purpose
The purpose of the present study was to validate a new spinal sagittal classification.
Methods
We retrospectively included 105 consecutive AIS patients who underwent posterior spinal fusion. Preoperative long-standing EOS radiographs were available on all patients. Patients were classified according to the four suggested sagittal patterns: type 1, 2a, 2b or 3. Several predetermined sagittal parameters were compared between the groups.
Results
The mean preoperative Cobb angle was 64° ± 12°, and 73% of the patients were female. Of 105 patients, 51 were type 1, 14 were type 2a, one was type 2b and 39 were type 3. The distribution of the four sagittal patterns was significantly different compared with the original publication (p < 0.05). However, the two study populations were comparable in terms of Lenke and Roussouly types (p = 0.49 and 0.47, respectively). In our study population, the sagittal groups differed significantly in terms of thoracic kyphosis, length of thoracic and lumbar curves, lumbar lordosis, thoracic slope, C7 slope, pelvic incidence and sacral slope (p < 0.05).
Conclusion
The distribution of the four sagittal patterns varies between AIS cohorts. Type 2b was rare, which limits the clinical applicability. Contrary to the original publication, we found that the spinopelvic parameters lumbar lordosis, pelvic incidence and sacral slope were significantly different between the Abelin-Genevois types. Hence, the corrective surgical strategy may need to incorporate these spinopelvic parameters to achieve a balanced spine requiring a minimum of energy expenditure.
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material.

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Adolescent idiopathic scoliosis (AIS) is a three-dimensional deformity of the spine. Surgical treatment of AIS requires attention to both the coronal and sagittal deformity. Recently, focus has been on maintaining or restoring sagittal alignment after surgical treatment of adult spinal deformity, due to evidence suggesting that malalignment is correlated with dysfunction and decreased quality of life [1, 2]. Furthermore, sagittal imbalance has also been associated with a high complication rate—and increases the risk of lumbar pathology after long spinal fusions [3, 4]. Less is known about the consequences of sagittal malalignment in AIS. Overall, this highlights the need for accurate preoperative sagittal evaluation for direct comparison of research findings and postoperative complications. The Lenke classification [5] is used for preoperative planning of AIS curve types, but the coronal component is primarily used in the surgical strategy, whereas the sagittal variables are not typically used in preoperative planning. Abelin-Genevois et al. [6] have recently suggested a new classification system describing four sagittal profiles to guide the surgical strategy and to serve as a complementary tool to the Lenke classification. Before this classification system can be generally applied, it needs to be validated in different patient populations. Therefore, we aimed to validate this new classification system in an independent cohort.
Materials and methods
This study included a consecutive series of AIS patients surgically treated in a single pediatric spine unit from January 1, 2015, to December 31, 2017. We included patients undergoing surgical treatment with posterior fusion only and excluded patients without preoperative and postoperative long-standing EOS radiographs. Study approval was obtained from the institutional review board.
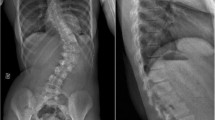
Patients were categorized using the recently published sagittal classification for AIS [6] (Fig. 1):
-
Type 1: normal sagittal shape. Defined as T10–L2 > − 10° (negative values indicate lordosis) and T4–T12 ≥ 20°.
-
Type 2a: hypokyphotic thoracic spine with cervical kyphosis (preserving three alternating sagittal curves). Defined by T4–T12 < 20° and T10–L2 between − 10° and 10°.
-
Type 2b: thoracic hypokyphosis and thoracolumbar kyphosis, sagittal shape including four alternating sagittal curves. Defined by T4–T12 < 20° and T10–L2 > 10°.
-
Type 3: only two alternating sagittal curves: a proximal cervicothoracic kyphosis and a long thoracolumbar lordosis. Defined by T10–L2 ≤ − 10° (Fig. 2).
The classification algorithm was received from the corresponding author to the original article.
As only one patient was type 2b, we merged groups 2a and 2b in the comparative analysis between groups, to improve the statistical power of the study.
Radiographic assessment
Radiographic assessment was performed with EOS imaging® system (EOS Imaging, France), and supine bending films were included for Lenke classification. The EOS imaging system takes simultaneous frontal and lateral radiographs of the whole spine in standing position and with arms flexed in 45°. Radiographs were uploaded to an online imaging software KEOPS® (S.M.A.I.O, Lyon, France) where all measurements were performed by the primary author.
Frontal radiographs and bending films: Measurements included major curve (Cobb’s angle) and Lenke type [5].
Lateral radiographs: Measurements included the following: global cervical spine angle (C1–C7), upper cervical angle (C1–C2), lower cervical angle (C2–C7), C7 slope: formed by the tangent to the inferior endplate of C7 and the horizontal reference line and fixed thoracic kyphosis (TK) (T4–T12), global TK, length of global TK. Lumbar parameters included fixed lumbar lordosis (LL) (L1–S1), global LL and length of global LL.
All patients were categorized according to Roussouly [7].
Global LL and global TK were measured in relation to the position of the inflexion point and found at the limit where one curve transitioned into another [8].
Furthermore, we also included the following spinopelvic parameters: pelvic incidence (PI), sacral slope (SS) and pelvic tilt (PT).
If the patient presented with an odd number of vertebrae, the vertebrae labeling suggested by the Spinal Deformity Study Group was used [9].
Statistical analysis
Patients were categorized based on the sagittal profile into the four groups defined by Abelin-Genevois et al. [6]. We compared our population to the original using Fisher’s exact test and Chi-squared test as appropriate. Continuous data were assessed for normal distribution using histograms and reported as mean ± standard deviation and analyzed using ANOVA. Post hoc analysis was done with Tukey’s honestly significant difference test. Non-normally distributed data were reported with median and interquartile range (IQR), and groups were compared using Kruskal–Wallis test and post hoc pairwise Wilcoxon rank-sum test. Furthermore, correlation between specific spinopelvic parameters including PI, PT and SS and the earlier described kyphotic and lordotic parameters was assessed using Spearman correlation analysis. A p value < 0.05 was considered statistically significant. All statistical analyses were performed using R, version 3.4.1 (R Core Team, 2015, Vienna, Austria).
Results
During the study period, 122 patients were identified as eligible for inclusion. We excluded 7 patients due to instrumentation with magnetically controlled growing rods and 10 patients due to anterior only surgery. Of 105 patients, 51 patients were type 1, 14 patients were type 2a, 1 patient was type 2b and 39 patients were type 3. The four sagittal groups did not differ significantly in age and mean preoperative major curve size (Table 1). The mean preoperative major curve angle was 64 ± 12°, and 73% of the patients were females. Twenty percent of patients were Risser grade 5, 46% were grade 4, 11% were grade 3, 6% grade 2, 4% grade 1 and 13% grade 0. Comparing this study population to the original one, we saw a clear difference in distribution of the four sagittal types (p < 0.01) (Fig. 2). There was no statistically significant difference between the original cohort and our cohort in terms of Lenke types or Roussouly types (p = 0.48 and p = 0.47, respectively) (Table 1) (Fig. 2).
Comparison of sagittal parameters across the three sagittal groups
The distribution of the sagittal and spinopelvic parameters across the three groups (type 1, type 2 and type 3) is presented in Table 3. Type 1 had a mean global TK 36° ± 17 with 10 ± 2 vertebrae in the TK and 6 (IQR 5-7) vertebrae in the LL and a global LL 61° ± 11. The C7 slope was positive and the thoracolumbar junction straight (Fig. 3). In type 2, we found a mean global TK 17° ± 7 and global LL 51° ± 12. Global C angle was 16° ± 11 (Figs. 4 and 5). Type 3 had a mean global TK 30.5° (± 10.7) and mean thoracic vertebrae 8 (± 2.4). Global LL was 66.1° (± 14.2) with median lumbar vertebrae 8 (IQR 7-10) (Fig. 6).
Regarding the thoracic parameters, the three sagittal groups differed significantly in terms of global TK (p < .001), fixed TK (p < .001) and length of thoracic curve (p = .007). We found statistically significant difference between groups 1 and 2 and groups 1 and 3 in terms of fixed TK (Table 2). All the groups differed significantly from each other regarding global TK. The mean number of thoracic vertebrae was significantly different between groups 1 and 3.
We found significant differences between the groups in terms of global LL (p < 0.001), fixed LL (p < .001), T10–L2 angle (p < .001) and length of lumbar curves (p < 0.001) (Table 2). The post hoc test further indicated a significantly different relationship between groups 1 and 2, and 2 and 3 in terms of global LL. Only groups 1 and 2 were significantly different in terms of fixed LL. The length of lumbar curve was significantly different between groups 1 and 3 and between groups 2 and 3.
The C7 slope was significantly different between the three groups (p = 0.04). The main reason for the difference was found in the post hoc test between groups 1 and 2. We found no difference between the groups in terms of cervical lordosis (p = 0.28) or upper and lower cervical angle (p = .69 and p = .18, respectively).
Finally, the spinopelvic parameters were distributed statistically significant different from the original study in terms of SS (p = .004) and PI (p = .003). The main explanation for the difference between the groups was found in groups 1 and 3 in the post hoc analysis (Table 2).
Correlation analysis
Correlation analysis showed good correlation between the spinopelvic parameters and the lumbar parameters. Thus, PI was related to global LL and fixed LL and was inversely correlated with the T10–L2 angle. SS also showed significantly positive correlation with global LL, fixed LL and inverse correlation with T10–L2. Thus, the greater the SS, the smaller the T10–L2 angle. The regional thoracic parameters were positively correlated with the lumbar parameters. Specifically, there was a modest correlation between fixed TK and T10–L2. Finally, C7 slope showed significant correlation with both lumbar and thoracic parameters (Table 3).
Discussion
In this study, we found a significantly different distribution in sagittal curve types compared to the original publication by Abelin-Genevois et al. Since only one patient was a type 2b, this study could only identify three clinically meaningful sagittal types.
Type 1, sagittal profile, was found in 49% of the patients. Still 27% of the type 1 patients were hyperkyphotic (T4–T12 > 40°) compared to the normal population. This is in line with previous studies showing that although AIS patients are traditionally believed to have a relative hypokyphosis there is substantial variation of the TK at the preoperative stage [10]. The current classification system does not actually distinguish between normal and hyperkyphosis, which we believe is a limitation of the classification.
Type 2a, hypokyphotic sagittal profile, was found in only 13% patients compared with 39% in the original publication. Type 2a is classified by a normal thoracolumbar junction and hypokyphosis. Nonetheless, 18% of type 3 patients had a global hypokyphosis, which could be the reason for the discrepancy between the numbers in types 2 and 3 compared to the original population. Type 3 is only characterized by the thoracolumbar junction and not by any kyphotic measurements. A recent study by Abelin-Genevois et al. [11] found poor correlation between the 2D and 3D measures of T10–L2. The uncertainty of T10–L2 measurement in the 2D projection could be the reason for our difficulties distinguishing type 2 from type 3. We believe this highlights the algorithm’s need for revision since the measurement of the thoracolumbar junction is the most pivotal parameter in the classification algorithm. Finally, we saw that type 2 patients had a reduced C7 slope compared to the normal type 1, indicating that the hypokyphotic/straight spine continues in the cervical region.
Type 3 is characterized by cervicothoracic kyphosis and a lordotic thoracolumbar junction. In comparison with the normal type 1 patients, we saw that type 3 patients had significantly longer lordosis (no. of vertebrae) even though the magnitude of the global LL was not significantly different. These findings are in accordance with the original paper. However, we found no significant difference in cervical parameters when comparing group 3 to either group 1 or 2, contrary to the original publication.
Studies show that postoperative changes in the cervical profile vary according to the preoperative sagittal profile of TK and therefore support the inclusion of the cervical parameters in the preoperative planning [12,13,14]. For this reason, Abelin-Genevois et al. designed this classification system to address and include the cervical spine in the preoperative planning. Nevertheless, we could not differentiate the cervical parameters between the three Abelin-Genevois types. We did, however, find a reduced C7 slope in the hypokyphotic type 2, supporting the idea that each region of the spine is interdependent of each other. Little consensus exists in terms of cervical parameters and its association with health-related quality of life in patients with AIS [12, 15, 16]. Still, many studies report high incidence of cervical kyphosis in thoracic AIS, some up to 67% preoperatively [12, 17, 18]. In our population, only 6 patients had a global cervical kyphosis (cervical angle above 0°). To our knowledge, there is no strong evidence showing that changes in cervical parameters following AIS surgery translate into decreased quality of life. Considering our data, we do not find support for including cervical parameters in the preoperative evaluation.
A balanced spine is obtained when the spine and pelvis are aligned so that energy expenditure is minimized [19]. Roussouly et al. described how changes in the spinopelvic profile occur after surgical correction in AIS. They found altered pelvic alignment with pelvic retroversion resulted in increased PT and therefore a slightly decreased SS [13]. These data support the importance of evaluating the spinopelvic parameters before surgery. Compared to the original study, the most substantial finding in our data is the difference in the spinopelvic parameters between the Abelin-Genevois types. Mac-Thiong et al. [20] evaluated the spinopelvic parameters in normal children and adolescents and found mean values of PI, PT and SS comparable to our results. In the present study, the spinopelvic parameters, PI and SS, were found to be significantly different between type 1 and type 3. Furthermore, PI was significantly correlated with global lordosis, fixed LL and the thoracolumbar junction. Studies on spinopelvic balance in the normal pediatric population and in AIS patients have shown strong correlation between PI and the orientation of the sacrum (SS) and the pelvis (PT) [20, 21]. Furthermore, they also found that SS correlates with the shape of the lordosis (LL) [20]. This is in accordance with our results and supports the possible difference between Abelin-Genevois types 1 and 3. Type 3 is characterized by a longer and larger lordosis and therefore also a larger PI and SS. The strong relationship between PI and lumbar sagittal alignment in both normal and AIS spines emphasizes the importance of considering both pelvic anatomy and position relative to the sagittal alignment. We found poor correlation between SS and PT. Theoretically, these two parameters should be inversely correlated. The difference between the two cohorts in terms of pelvic parameters as well as the poor correlation between SS and PT could be attributed to pelvic parameters depending on age and race [8, 22, 23]. This is further supported by the relatively large proportion (23%) of our patients with a Risser grade below or equal to 3. Thus, comparing populations with different bone ages with respect to pelvic parameters could be ambiguous.
The current study has some limitations. Absolute values are difficult to compare between studies considering interobserver variation. Both the original study and this study have small populations, which could lead to a potential type 2 error. Furthermore, we used a conservative post hoc analysis, and by decreasing our type 1 error, we may have increased the risk of type 2 error. This could potentially explain some of the incongruence between the original study and our results. Lastly, it is criticized that 2D lateral view results from the projection of the 3D deformity.
We suggest further validation in different and larger demographic settings. In addition, our results show that the current algorithm only provides segmental sagittal classification of the spine and not, as intended, a global classification into the four suggested sagittal types. In conclusion, we encourage further studies evaluating postoperative alignment in the four Abelin-Genevois types and support a classification system with applicable sagittal parameters to assess the sagittal alignment as a tool to compare research findings and provide surgical guidelines in AIS. The published classification does not fully explain how to classify the patients. This is probably due to an oversimplification of the classification algorithm, which is why we suggest further revision before general application.
Conclusion
The distribution of the four sagittal patterns varies between AIS cohorts. Type 2b was rare, which limits the clinical applicability. Contrary to the original publication, we found that global LL, PI and SS were significantly different between some of the Abelin-Genevois types. Hence, the corrective surgical strategy may need to incorporate spinopelvic parameters to achieve a balanced spine. Finally, this study did not provide supporting evidence to include the cervical parameters in the preoperative evaluation of AIS patients.
Change history
28 January 2020
Unfortunately, the names of the members of the Texas Children’s Hospital Spine Study Group have not been mentioned in the published article.
References
Glassman SD, Berven S, Bridwell K et al (2005) Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976) 30:682–688
Faundez A, Hoffmeyer P, Aunoble S et al (2014) Evidence showing the relationship between sagittal balance and clinical outcomes in surgical treatment of degenerative spinal diseases: a literature review. Int Orthop 39:87–95. https://doi.org/10.1007/s00264-014-2516-6
Bhagat S, Vozar V, Lutchman L et al (2013) Morbidity and mortality in adult spinal deformity surgery: Norwich Spinal Unit experience. Eur Spine J 22:42–46. https://doi.org/10.1007/s00586-012-2627-y
de Jonge T, Dubousset JF, Illés T (2002) Sagittal plane correction in idiopathic scoliosis. Spine (Phila Pa 1976) 27:754–760
Lenke LG, Betz RR, Harms J et al (2001) Adolescent idiopathic scoliosis. J Bone Jt Surg Am 83:1169–1181. https://doi.org/10.2106/00004623-200108000-00006
Abelin-Genevois K, Sassi D, Verdun S, Roussouly P (2018) Sagittal classification in adolescent idiopathic scoliosis: original description and therapeutic implications. Eur Spine J. https://doi.org/10.1007/s00586-018-5613-1
Roussouly P, Gollogly S, Berthonnaud E, Dimnet J (2005) Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976) 30:346–353
Roussouly P, Nnadi C (2010) Sagittal plane deformity: an overview of interpretation and management. Eur Spine J 19:1824–1836. https://doi.org/10.1007/s00586-010-1476-9
O’Brien MFO, Kuklo TR (2004) Radiographic measurement manual Editors in Chief
Ohrt-Nissen S, Hallager DW, Karbo T et al (2017) Radiographic and functional outcome in adolescent idiopathic scoliosis operated with hook/hybrid versus all-pedicle screw instrumentation—a retrospective study in 149 patients. Spine Deform 5:401–408. https://doi.org/10.1016/j.jspd.2017.05.002
Post M, Verdun S, Roussouly P, Abelin-Genevois K (2018) New sagittal classification of AIS: validation by 3D characterization. Eur Spine J. https://doi.org/10.1007/s00586-018-5819-2
Lee CS, Lee D-H, Hwang CJ et al (2017) Cervical sagittal alignment in patients with adolescent idiopathic scoliosis: is it corrected by surgery? J Neurosurg Pediatr 21:292–301. https://doi.org/10.3171/2017.8.peds17357
Roussouly P, Labelle H, Rouissi J, Bodin A (2013) Pre- and post-operative sagittal balance in idiopathic scoliosis: a comparison over the ages of two cohorts of 132 adolescents and 52 adults. Eur Spine J. https://doi.org/10.1007/s00586-012-2571-x
Pepke W, Almansour H, Lafage R et al (2019) Cervical spine alignment following surgery for adolescent idiopathic scoliosis (AIS): a pre-to-post analysis of 81 patients. BMC Surg 19:1–12. https://doi.org/10.1186/s12893-019-0471-2
Grob D, Frauenfelder H, Mannion AF (2007) The association between cervical spine curvature and neck pain. Eur Spine J 16:669–678. https://doi.org/10.1007/s00586-006-0254-1
Jeon WK, Kang SS, Youn MS et al (2016) Relationship between cervical sagittal alignment and health-related quality of life in adolescent idiopathic scoliosis. Eur Spine J 25:3114–3119. https://doi.org/10.1007/s00586-016-4488-2
Ilharreborde B, Vidal C, Skalli W, Mazda K (2013) Sagittal alignment of the cervical spine in adolescent idiopathic scoliosis treated by posteromedial translation. Eur Spine J 22:330–337. https://doi.org/10.1007/s00586-012-2493-7
Canavese F, Turcot K, De Rosa V et al (2011) Cervical spine sagittal alignment variations following posterior spinal fusion and instrumentation for adolescent idiopathic scoliosis. Eur Spine J 20:1141–1148. https://doi.org/10.1007/s00586-011-1837-z
La Maida GA, Zottarelli L, Mineo GV, Misaggi B (2013) Sagittal balance in adolescent idiopathic scoliosis: radiographic study of spino-pelvic compensation after surgery. Eur Spine J 22(Suppl 6):S859–S867. https://doi.org/10.1007/s00586-013-3018-8
Mac-Thiong JM, Labelle H, Berthonnaud E et al (2007) Sagittal spinopelvic balance in normal children and adolescents. Eur Spine J 16:227–234. https://doi.org/10.1007/s00586-005-0013-8
Pasha S, Aubin C-E, Sangole AP et al (2014) Three-dimensional spinopelvic relative alignment in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 39:564–570. https://doi.org/10.1097/BRS.0000000000000193
Betz RR, Labelle H, Mac-Thiong J-M et al (2004) Sagittal alignment of the spine and pelvis during growth. Spine (Phila Pa 1976) 29:1642–1647. https://doi.org/10.1097/01.brs.0000132312.78469.7b
Lonner BS, Auerbach JD, Sponseller P et al (2010) Variations in pelvic and other sagittal spinal parameters as a function of race in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 35:374–377. https://doi.org/10.1097/BRS.0b013e3181bb4f96
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
B. Dahl and M. Gehrchen have received institutional grants from K2M and Medtronic. J. Heydemann is a comitee member of POSNA, AACPDM and SRS and shareholder in Merck, Sanofi Avanti and Orthopediatrics, unrelated to this work. L. Deveza is a shareholder in Lento Medical Inc. and has received research funding from OREF (Orthopedic Research an Education Fund), unrelated to this work. C. Dragsted, S. Ohrt-Nissen, M. Jain, D. Liu and S. Fruergaard have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fruergaard, S., Jain, M.J., Deveza, L. et al. Evaluation of a new sagittal classification system in adolescent idiopathic scoliosis. Eur Spine J 29, 744–753 (2020). https://doi.org/10.1007/s00586-019-06241-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-06241-5