Abstract
Purpose
To compare intermediate screws (IS) with kyphoplasty (KP) in posterior short-segment fixation (PSSF) for patients with single-level thoracolumbar burst fractures.
Methods
Between 2010 and 2016, 1465 patients were retrospectively reviewed; 48 patients were enrolled with a minimal follow-up of 2 years. Perioperative and functional outcomes were compared. The regional Cobb angle (CA) was included in radiographic analysis. Implant failures or CA correction loss over 10° were regarded as surgical failures. Multiple linear regression was performed to investigate the risk factors of kyphosis recurrence.
Results
Fluoroscopic time (23.7 ± 3.6 vs. 79.3 ± 12.1 s, p < 0.001), operative time (109.6 ± 13.1 vs. 123.8 ± 19.0 min, p = 0.006) and blood loss (104.6 ± 34.9 vs. 129.1 ± 21.7 ml, p = 0.005) were all lower in the IS group. The KP group had lower Visual Analogue Scale scores (3.3 ± 0.9 vs. 2.7 ± 0.8, p = 0.028) and greater anterior body height (ABH) (30.3 ± 9.0 vs. 36.3 ± 11.0%, p = 0.044) after surgery, and less correction loss (5.6 ± 2.7 vs. 0.4 ± 1.2%, p < 0.001). Both groups had a CA correction loss of 4° with a 10% failure rate. The A3 Magerl subclassification, smaller preoperative ABH and smaller postoperative CA had positive correlations with CA correction loss.
Conclusion
PSSF with KP provides better back pain relief, greater ABH reduction and less correction loss, while IS has the advantages of less operative time, fluoroscopic time and blood loss. Magerl subclassification of burst fracture is a potential predictor for recurrent kyphosis. Reducing fractured vertebral body height rather than segmental curvature may be more important in PSSF.
Study design
Retrospective, non-randomized controlled study.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
First proposed in 2005, the thoracolumbar injury classification and severity score system (TLICS) distinguishes a patient in need of surgery by a score greater than 4 [1]. McCormack et al. [2] put forward a load sharing classification (LSC) system designed to help guide the surgical strategy for spinal fractures. However, it is still unclear when additional reinforcement should be used for posterior short-segment fixation (PSSF). PSSF is the most commonly used surgical procedure for single-level thoracolumbar burst fractures (STBF) [3,4,5] and traditionally involves inserting pedicle screws above and below the fractured vertebrae only. Although this procedure is proven to save segmental motion and be as effective as long-segment pedicle screws fixation [6, 7], poor outcomes such as kyphosis recurrence, vertebral bone nonunion, and implant failure are commonly reported [4, 5, 8,9,10,11], especially for Magerl Type A3 fractures (Fig. 1) [4, 12]. Several biomechanical studies have revealed that insufficient support for the anterior column may be responsible for these unsatisfactory outcomes [13,14,15]. Moreover, the cavity that appears in the fractured vertebral body after distraction of the adjacent vertebra slows the healing of bone tissue, which accelerates correction loss [16]. Since the concept of using intermediate screws (IS) was proposed by Dick et al. [17], augmenting screws to the injured vertebrae has become a common method, even for severe vertebral burst fractures. Recently, a number of studies have reported the efficacy of kyphoplasty (KP) for vertebral fractures with vertebral wall deficiency, demonstrating kyphoplasty was also applicable for vertebral burst fractures [18,19,20]. However, the optimal procedure for fractured vertebra remains controversial, especially for people over the age of 50 years as this population often exhibits a lower bone mass and an increased risk of osteoporosis. The objective of this study is to compare outcomes of these two different procedures as PSSF reinforcement for patients with STBF.
Materials and methods
Patient
We conducted a retrospective review of 1465 patients with thoracolumbar fractures in our institute between January 2010 and February 2016. The study was carried out with the approval of our institution’s ethics committee. Forty-eight patients met the selection criteria and were given a thoracolumbar injury classification and severity score (TLICS) before surgery [1]. The inclusion criteria were as follows: (1) trauma-induced single-level thoracolumbar (T11-L3) A3 burst fracture according to Magerl classification [21]; (2) subjects received posterior short-segment pedicle fixation with Universal Spine System (USS) from Synthes® including the superior and inferior segment, with either two additional screws or kyphoplasty at the injured vertebrae; (3) over 50 years of age; (4) the follow-up duration was no less than 2 years and all the information of interest was available. Subjects were excluded if: (1) there were previous fractures or surgical interventions at the vertebra above, below, or at the fractured level; (2) the patient had combined surgery; for example, both pedicle screws and kyphoplasty at the influenced levels; (3) pathological fractures; (4) the patient underwent implant removal in the follow-up period; (5) the bone mineral density (BMD) was less than − 2.5. Patients with additional intermediate screws formed the IS group, while patients with kyphoplasty formed the KP group. The detailed screening flowchart is presented in Supplement 1.
The BMDs were evaluated using the dual-energy X-ray absorptiometry (DEXA) (Discovery Wi, Hologic, America). Patients were labeled with A3.1, A3.2 and A3.3 based on Magerl burst fracture subclassification (Fig. 2). All patients received a load sharing classification (LSC) score based on the amount of vertebral body damaged, spread of fracture fragments and degree of kyphosis deformity observed on computed tomography (CT) and plain films [2].
Surgical procedures
After administrating general anesthesia, all patients were placed in the prone position after general anesthesia with their pelvis and manubrium supported by pads. Neurological monitoring and biplane fluoroscopy were applied for all patients. A standard open posterior midline approach was performed, centering the fractured vertebra, and systematically revealing the posterior vertebral structure. The USS spine system was applied, and four schanz screws were inserted into the cephalad and caudal vertebra at the fractured level. These procedures were essential for both groups.
For the IS group, two additional polyaxial screws measuring 5–10 mm shorter than the ones above them were inserted into the fractured vertebrae through the pedicles. Following the insertion of bent rods, sequential distraction and restoration of lordosis was performed between the ipsilateral adjacent screws to reduce kyphosis. When the vertebral height was sufficiently restored, the bent rods were substituted with straight rods and the free nuts were tightened finally.
For the KP group, manual distraction and restoration of lordosis was performed directly between the bilateral screws of the adjacent vertebra above and below the fractured vertebrae. In the second surgical phase, a procedure for balloon kyphoplasty was followed using the steps described by Lieberman et al. [22]. Polymethylmethacrylate (PMMA) cement (KyphX; Kyphon Inc) was injected following the bilateral balloon expansion to further correct the kyphosis of the fractured body. Under continuous fluoroscopy guidance, each balloon was inserted into the vertebral anterior column and inflated to over 150 psi. After withdrawing the balloons, an average of 5–7 cc of viscous PMMA was injected carefully to prevent the cement from leaking. The incremental temperature cement delivery and graded infusion techniques were used in our institute to minimize the leakage rate [23].
Posterolateral fusions with an autogenous or allograft bone were applied to all patients. Convex fracture fragments in the canal were reduced or removed, and additional vertebral laminectomy was performed for patients with inextricable compression. Patients were strictly confined to the supine position for the first 24 h. Drains were placed immediately after surgery and removed after 2 days. Implants were not removed in the follow-up period. The intraoperative fluoroscopic time, estimated blood loss, operative time and hospital stay after surgery were all recorded.
Clinical assessment
The neurological function of patients was evaluated preoperatively and at the final follow-up according to the guidelines set by The American Spinal Injury Association (ASIA) [24]. The Visual Analogue scale (VAS) was used to evaluate back pain before and after surgery [25].
Radiographic evaluation
The anteroposterior and lateral radiographs on standing position were routinely performed before and after surgery and at follow-up. CT scans were routinely performed before surgery. The regional Cobb angel (CA) was measured as the angle between the superior endplate of the vertebrae above and the inferior endplate of the vertebrae below the fractured level [25]. The anterior vertebral body height (ABH) was defined as the percentage of the anterior height of the fractured vertebrae with respect to the mean value of the anterior vertebral height of the vertebra above and below the injured level; an analogous definition was used for the posterior vertebral body height (PBH). The CA, ABH and PBH were measured on a lateral radiograph. The spinal canal encroachment (SCE) was obtained before surgery and calculated on CT scan as described by Panagiotis et al. [26]. The correction loss refers to the increased kyphosis angle or decreased vertebral body height at the final follow-up as compared to the condition immediately after the operation. If a CA correction loss more than 10° was found, or if an internal fixation failure was observed, the surgery was regarded as a failure [27].
Statistical analysis
SPSS 19.0 (IBM, Armonk, NY, USA) was used to perform data processing. The final data were presented in percentages for categorical variables and mean with ± standard deviation for continuous variables, with probability values of less than 0.05 indicating a statistically significant difference. For numerical data, the Student’s t test was used for data with a normal distribution; otherwise, the Mann–Whitney U test was used. Pearson’s Chi-square test and the Fisher exact test were used for categorical data, while. Ranked data were analyzed using the Mann–Whitney U test. Multiple linear regression was used to find correlations between various results.
Results
Demographics
The demographic data of both groups are shown in Table 1. The IS group was composed of 14 males and 13 females between the ages of 51–71 (mean age 60 years), while the KP group consisted of 12 males and 9 females between the age of 50–78 (mean age 62 years) (Fig. 3). The mean follow-up duration was 28 months for both groups. There were no significant differences between the two groups for age, gender, cause and level for injury, and the time interval between injury and surgery. The mean BMD of L1–L5 was lower in the KP group than in the IS group (− 1.7 ± 0.4 vs. − 1.9 ± 0.4); however, this difference was not statistically significant (p = 0.262). The distribution of the LSC scores among patients were as follows: in the IS group, there were one 4-points, two 5-points, eleven 6-points, nine 7-points, three 8-points and one 9-points; in the KP group, there were three 5-points, eight 6-points, seven 7-points, two eight-points and one 9-points. With respect to Magerl subclassification, six patients were A3.1, thirteen were A3.2 and eight were A3.3 in the IS group; in the KP group, five patients were A3.1, ten were A3.2 and six were A3.3. There were no significant differences in LSC score or distribution of Magerl subclassification between the two groups.
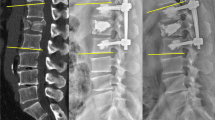
a–c Male, 54 years, L1 fracture, IS group. Lateral radiograph before operation (a) and immediately after operation (b) showed a CA reduction from 17° to 11° and an increase in ABH from 76 to 97%. The Cobb angle (CA) and anterior body height (ABH) were well maintained 2 years later (c). d–f Female, 59 years, L1 fracture, KP group. Preoperative radiograph (d) showed the fractured vertebrae collapsed with an ABH of 28% and CA of 17°, the operation resulted in changes to 89% and 1°, respectively, with no cement leakage (e). After 2 years, the reduction was generally maintained with minor correction loss (f)
Perioperative parameters
The summary of perioperative results is presented in Table 2. Fluoroscopic time, blood loss and operative time were all less in the IS group (23.7 ± 3.6 vs. 79.3 ± 12.1 s, p < 0.001; 104.6 ± 34.9 vs. 129.1 ± 21.7 ml, p = 0.005; 109.6 ± 13.1 vs. 123.8 ± 19.0 min, p = 0.006, respectively). The KP group had an insignificantly shorter length of stay after surgery compared to the IS group (8.1 ± 1.3 vs. 7.7 ± 1.3 days, p = 0.315). Thirteen patients in the IS group and eight patients in the KP group received a laminectomy, with no significant difference in proportion (48.1 vs. 38.1%, p = 0.343).
Functional results
According to the ASIA grading system, 2, 5 and 20 patients in the IS group were classified as grade C, D and E on admission, respectively. At the final follow-up, all patients were classified as Grade E except for one patient, who was ranked as Grade D. For the KP group, 1, 5 and 15 patients were classified as grade C, D and E on admission, respectively. Similarly, all patients were Grade E at the final follow-up, except for one patient who was given a Grade D. No significant difference was found in the ASIA scale distribution between the two groups, neither preoperatively nor after surgery.
Compared with the preoperative score, the VAS decreased from 7.5 ± 1.1 to 3.3 ± 0.9 immediately after surgery. For the KP group, the corresponding VAS was 7.5 ± 1.5 and 2.7 ± 0.8. Significant improvements in the VAS were observed in both groups (p < 0.05). Moreover, the postoperative VAS was lower in the KP group than in the IS group (3.3 ± 0.9 vs. 2.7 ± 0.8, p = 0.028).
Radiographic outcomes
A summary of the radiographic outcomes is presented in Table 3. The preoperative SCE was 34.4 ± 11.7% in the IS group and 35.1 ± 11.8% in the KP group, showing no significant difference (p = 0.823). For the IS group, the preoperative CA of 23.6° ± 6.9° was corrected to 5.7° ± 2.9° after surgery; at the final follow-up, the CA was 9.6° ± 3.8° with a significant correction loss of 3.8° ± 2.9° (p < 0.001). For the KP group, the CA was 21.4° ± 5.9° before surgery, 5.2° ± 2.3° immediately after surgery and 9.4° ± 3.4° at the final follow-up; a significant correction loss of 4.1° ± 3.2° was observed (p < 0.001). There was no significant difference in CA at different stages between two groups (p > 0.05), nor any significant CA correction loss difference (p = 0.713). The surgery corrected ABH from 53.0 ± 12.2 to 83.3 ± 5.1% in the IS group, and 58.2 ± 12.2 to 90.1 ± 5.3% in the KP group. No significant difference was observed between the ABH of the two groups before surgery (p > 0.813), but this changed after surgery (p < 0.001) as the KP group showed significantly greater ABH correction from the surgery (30.3 ± 9.0 vs. 36.3 ± 11.0%, p = 0.044). At the final follow-up, the ABH of the IS group showed a significant correction loss of 5.6 ± 2.7% (83.3 ± 5.1 vs. 77.7 ± 5.8%, p < 0.001), but remained at 89.7 ± 5.6% in the KP group. There was a significant difference of ABH correction loss between the two groups (5.6 ± 2.7 vs. 0.4 ± 1.2%, p < 0.001). The PBH was similar between two groups at each stage. No correction loss was found in either group.
The failure rate was 11.1% (3/27) in the IS group and 9.5% (2/21) in the KP group; no statistically significant difference was found (p > 0.858). Patients who met the surgical failure criteria all experienced a correction loss of the CA of more than 10° during the follow-up; beyond that, no failure of the posterior instrumentation happened, and no revision surgery was performed. Cement leakage was not found in any patients of the KP group (Table 4).
Analysis for risk factors of correction loss of CA and ABH
Multiple linear regression (MLR) was performed to identify the risk factors of correction loss of CA and ABH. Variables group, age, gender, BMD, Magerl subclassification for A3 burst fracture (A3.1, A3.2, A3.3), LSC (divided into less than or equal to 7 and greater than 7), laminectomy, preoperative CA, postoperative CA, preoperative ABH, postoperative ABH, preoperative PBH and postoperative PBH were all included in the analysis. The MLR showed that Magerl subclassification (standardized coefficient = 0.658, p < 0.001), postoperative CA (standardized coefficient = −0.308, p = 0.005) and preoperative ABH (standardized coefficient = −0.215, p = 0.046) were significant factors for CA correction loss, meaning that a more serious subclassification of A3 (A3.3 > A3.2 > A3.1), smaller postoperative CA and smaller preoperative ABH all contribute to greater CA correction loss. As for ABH correction loss, the variables group was the only significant factor (standardized coefficient = −0.768, p < 0.001), consisting with Student’s t test for ABH. Other factors such as BMD, LSC and laminectomy did not significantly affect the correction loss of CA nor ABH.
Discussion
This study comprehensively compared the functional and radiographic outcomes of PSSF with IS and KP. The results showed that PSSF with KP was associated with less back pain immediately after surgery, and provided a greater ABH reduction with less correction loss. However, KP required a greater operative time, more intraoperative fluoroscopic time and caused more blood loss. Similar rates of kyphosis recurrence were observed in both groups. Risk factors for CA correction loss included having a smaller preoperative ABH, a more severe burst fracture, and having achieved a better reduction of CA by surgery.
Neurological improvement after both procedures was satisfactory in this study. Back pain appeared lighter after PSSF, especially for patients with KP, underlining the dramatic pain reduction effect of PMMA bone cement in treating painful vertebral fractures [28].
In our study, the CA was similar between groups immediately after surgery and at the final follow-up. It is important, however, to note that the ABH was significantly lower in the IS group, both postoperatively and at the final follow-up; ABH was reduced by 5.6% in the IS group but was better maintained in the KP group. This indicates that KP was better able to reduce the body height of the fractured vertebrae to its intact condition. After a follow-up at least 2 years, kyphosis recurrence was observed in both groups with a CA correction loss nearly 4°. Despite correcting the regional kyphotic deformity through distraction, the collapsed endplate of the intermediate vertebrae did not always regress thereupon for lack of attachment of ligament and fiber ring. The inflated balloon in Kyphoplasty was able to prop up the collapsed superior endplate, whereas the additional intermediate screws could not. The subsequent PMMA cement provided stronger vertebral internal support for maintaining restoration of the spine.
Patients with recurrent kyphosis after PSSF are more likely to suffer moderate to severe pain that seriously affect their quality of life [29], so avoiding this issue is an important objective of PSSF surgery. However, a review of 5748 patients by Verlann et al. [30] concluded that none of the techniques whether anterior, posterior or a combination of the two were able to maintain the corrected kyphosis angle. Porter et al. [31] concluded that there was a significant tendency for patients with poor bone mass to develop progressive kyphosis. Pellisé et al. [32] found that loss of correction was affected by the amount of bony comminution of the fracture, which is indicated by the LSC score. Yoganondon et al. [33] claimed that the posterior ligamentous complex is damaged after laminectomy, causing the deterioration of spinal stability and physiological curvature. In our study, however, BMD, LSC and laminectomy were not observed to be risk factors for CA correction loss; instead, we found that that the greatest predictor of CA correction loss was the type of Magerl subclassification. We infer that more severe burst fractures are accompanied with greater destruction of the anterior column and adjacent intervertebral disks, which are two critical factors of recurrent kyphosis [15, 34]. A significant negative correlation was found between preoperative ABH and CA correction loss, which is consistent with Wang et al. [29]. Interestingly, we also found that better surgical reduction of CA contributed to greater CA correction loss, suggesting that segmental angular reduction may not necessarily produce better long-term radiographic results. Wang et al. [29] advised surgeons to focus on reducing the fractured vertebral body height rather than the segmental curvature, a finding which concurs with the results of our study.
As for perioperative parameters, the IS group was shown to have lower operative time, intraoperative fluoroscopic time and blood loss. PSSF without KP involves less surgical trauma and radiation exposure compared to IS, which benefits older patients with decreased surgical tolerance.
The major limitation of this study was the relatively small sample size, due to the strict selection criteria required to control hybrid migration. Further studies with perspectiveness and randomization are needed to verify the results of our study.
Conclusion
Both intermediate screws and kyphoplasty are good enhancements in PSSF; KP provides better back pain relief and reduction of ABH with less correction loss, whereas IS involves less operative time, fluoroscopic time and blood loss. Magerl subclassification of burst fracture is a potential predictor for recurrent kyphosis, which is common after PSSF with both IS and KP surgery. Surgeons should focus on reducing the fractured vertebral body height rather than the segmental curvature in PSSF to reduce kyphosis.
References
Vaccaro AR, Lehman RA Jr, Hurlbert RJ, Anderson PA, Harris M, Hedlund R, Harrop J, Dvorak M, Wood K, Fehlings MG, Fisher C, Zeiller SC, Anderson DG, Bono CM, Stock GH, Brown AK, Kuklo T, Oner FC (2005) A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine 30:2325–2333
McCormack T, Karaikovic E, Gaines R (1994) The load sharing classification of spine fractures. Spine 19:1741–1744
Gelb D, Ludwig S, Karp JE, Chung EH, Werner C, Kim T, Poelstra K (2010) Successful treatment of thoracolumbar fractures with short-segment pedicle instrumentation. J Spinal Disord Tech 23:293–301. https://doi.org/10.1097/BSD.0b013e3181af20b6
McLain R, Sparling E, Benson D (1993) Early failure of short-segment pedicle instrumentation for thoracolumbar fractures. A preliminary report. J Bone Joint Surg Am 75:162–167
McLain RF, Burkus JK, Benson DR (2001) Segmental instrumentation for thoracic and thoracolumbar fractures: prospective analysis of construct survival and five-year follow-up. Spine J 1:310–323
Tezeren G, Kuru I (2005) Posterior fixation of thoracolumbar burst fracture: short-segment pedicle fixation versus long-segment instrumentation. J Spinal Disord Tech 18:485–488
Fuentes S, Blondel B, Metellus P, Gaudart J, Adetchessi T, Dufour H (2010) Percutaneous kyphoplasty and pedicle screw fixation for the management of thoraco-lumbar burst fractures. Eur Spine J 19:1281–1287. https://doi.org/10.1007/s00586-010-1444-4
Sasso RC, Renkens K, Hanson D, Reilly T, McGuire RA Jr, Best NM (2006) Unstable thoracolumbar burst fractures: anterior-only versus short-segment posterior fixation. J Spinal Disord Tech 19:242–248. https://doi.org/10.1097/01.bsd.0000211298.59884.24
Guven O, Kocaoglu B, Bezer M, Aydin N, Nalbantoglu U (2009) The use of screw at the fracture level in the treatment of thoracolumbar burst fractures. J Spinal Disord Tech 22:417–421. https://doi.org/10.1097/BSD.0b013e3181870385
Alanay A, Acaroglu E, Yazici M, Yazici M, Oznur A, Oznur A, Surat A, Surat A (2001) Short-segment pedicle instrumentation of thoracolumbar burst fractures: does transpedicular intracorporeal grafting prevent early failure? Spine 26:213–217
Lakshmanan P, Jones A, Mehta J, Ahuja S, Davies PR, Howes JP (2009) Recurrence of kyphosis and its functional implications after surgical stabilization of dorsolumbar unstable burst fractures. Spine J 9:1003–1009. https://doi.org/10.1016/j.spinee.2009.08.457
Altay M, Ozkurt B, Aktekin CN, Ozturk AM, Dogan Ö, Tabak AY (2007) Treatment of unstable thoracolumbar junction burst fractures with short- or long-segment posterior fixation in magerl type a fractures. Eur Spine J 16:1145–1155. https://doi.org/10.1007/s00586-007-0310-5
Anekstein Y, Brosh T, Mirovsky Y (2007) Intermediate screws in short segment pedicular fixation for thoracic and lumbar fractures: a biomechanical study. J Spinal Disord Tech 20:72–77. https://doi.org/10.1097/01.bsd.0000211240.98963.f6
Baaj AA, Reyes PM, Yaqoobi AS, Uribe JS, Vale FL, Theodore N, Sonntag VK, Crawford NR (2011) Biomechanical advantage of the index-level pedicle screw in unstable thoracolumbar junction fractures. J Neurosurg Spine 14:192–197. https://doi.org/10.3171/2010.10.SPINE10222
Norton RP, Milne EL, Kaimrajh DN, Eismont FJ, Latta LL, Williams SK (2014) Biomechanical analysis of four- versus six-screw constructs for short-segment pedicle screw and rod instrumentation of unstable thoracolumbar fractures. Spine J 14:1734–1739. https://doi.org/10.1016/j.spinee.2014.01.035
Knop C, Fabian HF, Bastian L, Blauth M (2001) Late results of thoracolumbar fractures after posterior instrumentation and transpedicular bone grafting. Spine 26:88–99
Dick JC, Fau Jones Mp, Zdeblick -, Zdeblick TA, Kunz DN, Kunz D, Horton WC, Horton WC (1994) A biomechanical comparison evaluating the use of intermediate screws and cross-linkage in lumbar pedicle fixation. J Spinal Disord Tech 7:402–407
Zou J, Mei X, Gan M, Wang G, Lu J, Yang H (2010) Is kyphoplasty reliable for osteoporotic vertebral compression fracture with vertebral wall deficiency? Injury 41:360–364
Kruger A, Zettl R, Ziring E, Mann D, Schnabel M, Ruchholtz S (2010) Kyphoplasty for the treatment of incomplete osteoporotic burst fractures. Eur Spine J 19:893–900. https://doi.org/10.1007/s00586-010-1281-5
Gan M, Zou J, Zhu X, Wang G, Yang H (2014) Balloon kyphoplasty for osteoporotic spinal fractures with middle column compromise. Injury 45:1539–1544. https://doi.org/10.1016/j.injury.2014.06.018
Magerl F, Aebi M, Gertzbein SD, Gertzbein SD, Harms J, Nazarian S (1994) A comprehensive classification of thoracic and lumbar injuries. Eur Spine J 3:184–201
Lieberman IH, Dudeney S, Reinhardt MK, Bell G (2001) Initial outcome and efficacy of “kyphoplasty” in the treatment of painful osteoporotic vertebral compression fractures. Spine 26:1631–1638
Yang H, Liu H, Wang S, Wu K, Meng B, Liu T (2016) Review of percutaneous kyphoplasty in China. Spine 41(Suppl 19):B52–B58. https://doi.org/10.1097/BRS.0000000000001804
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, Johansen M, Jones L, Krassioukov A, Mulcahey M (2011) International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med 34:535–546
Crichton N (2001) Visual analogue scale (VAS). J Clin Nurs 10:706
Korovessis P, Mpountogianni E, Syrimpeis V (2017) Percutaneous pedicle screw fixation plus kyphoplasty for thoracolumbar fractures A2, A3 and B2. Eur Spine J 26:1492–1498
Liao JC, Fan KF, Keorochana G, Chen WJ, Chen LH (2010) Transpedicular grafting after short-segment pedicle instrumentation for thoracolumbar burst fracture: calcium sulfate cement versus autogenous iliac bone graft. Spine 35:1482–1488. https://doi.org/10.1097/BRS.0b013e3181c176f8
Lovi A, Teli M, Ortolina A, Costa F, Fornari M, Brayda-Bruno M (2009) Vertebroplasty and kyphoplasty: complementary techniques for the treatment of painful osteoporotic vertebral compression fractures. A prospective non-randomised study on 154 patients. Eur Spine J 1(18 Suppl):95–101. https://doi.org/10.1007/s00586-009-0986-9
Wang XY, Dai LY, Xu HZ, Chi YL (2008) Kyphosis recurrence after posterior short-segment fixation in thoracolumbar burst fractures. J Neurosurg Spine 8:246–254. https://doi.org/10.3171/SPI/2008/8/3/246
Verlaan JJ, Diekerhof CH, Buskens E, van der Tweel I, Verbout AJ, Dhert WJ, Oner FC (2004) Surgical treatment of traumatic fractures of the thoracic and lumbar spine: a systematic review of the literature on techniques, complications, and outcome. Spine 29:803–814
Porter RW, Johnson K, McCutchan JD (1990) Wrist fracture, heel bone density and thoracic kyphosis: a case control study. Bone 11:211–214
Pellisé F, Barastegui D, Hernandez-Fernandez A, Barrera-Ochoa S, Bagó J, Issa-Benítez D, Cáceres E, Villanueva C (2015) Viability and long-term survival of short-segment posterior fixation in thoracolumbar burst fractures. Spine J 15:1796–1803. https://doi.org/10.1016/j.spinee.2014.03.012
Yoganandan N, Maiman DJ, Pintar FA, Bennett GJ, Larson SJ (1993) Biomechanical effects of laminectomy on thoracic spine stability. Neurosurgery 32:604–610
Hertlein H, Hartl W, Dienemann H, Schürmann M, Lob G (1995) Thoracoscopic repair of thoracic spine trauma. Eur Spine J 4:302–307
Acknowledgements
We would like to acknowledge the invaluable contribution of the patients. Thanks to all patients involved in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, J., Liu, H., Liu, H. et al. Intermediate screws or kyphoplasty: Which method of posterior short-segment fixation is better for treating single-level thoracolumbar burst fractures?. Eur Spine J 28, 502–510 (2019). https://doi.org/10.1007/s00586-018-5822-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-018-5822-7