Abstract
Design
Retrospective cohort.
Purpose
The aim of this study is to evaluate the effectiveness of percutaneous short fixation (PSFx) plus kyphoplasty (BP) for thoracolumbar fractures.
Methods
Thirty-six consecutive selected patients, aged 59 ± 17 years, with fresh single thoracolumbar A2, A3, and B2 AO-type fracture, received PSFx plus BP. The primary outcomes pain, and vertebral body deformity; and the secondary outcomes screw malposition, facet violation, PMMA leakage, adjacent segment degeneration (ASD) and loss of correction were evaluated. The f/up was 31 ± 7 months.
Results
Pain and kyphosis decreased and vertebral body heights increased significantly postoperation. PMMA leakage occurred in five cases; 6 (4 %) screws were grades III malpositioned in relation to pedicle; facet violation occurred in 8 (5.5 %) facets; loss of kyphosis correction was 3.68°; ASD occurred in two cases; interfacet fusion in ten (28 %) patients; Three patients were reoperated for different reasons.
Conclusions
PSFx plus BP for thoracolumbar fractures reduces significantly spinal deformity and pain with few complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The treatment of the thoracolumbar injuries remains until nowadays debatable for the lack of a reproducible classification system, predicting the treatment outcome and the natural history of an injury pattern.
Although there is a consensus for surgical treatment of thoracolumbar injuries in patients with neurologic deterioration, unstable fractures, and polytrauma, a universally accepted algorithm to decide the appropriate surgical technique remains lacking [1, 2].
Traditional open instrumented fusion for unstable thoracolumbar injuries is performed via a posterior pedicle screw construct spanning at least two vertebrae cephalad and two vertebrae caudal the injury. As an alternative to long instrumentation, short-segment pedicle screw fixation was introduced in the 80s, however, it frequently associated with a high failure rate for different reasons (osteoporosis, insufficient support of anterior column, insufficient fixation segments) [3].
In the last decade, percutaneous minimally invasive (MIS) pedicle screw fixation has been used initially for degenerative lumbar spine disorders, and later for trauma and metastatic spine disease. Indirect reduction of a fracture is usually sufficiently achieved via the prone positioning of the patient on the surgical table and distraction with pedicle instrumentation. However, although the vertebral walls give the radiological impression of a good reduction with the pedicle screw construct, the middle part of the endplate cannot be reduced [4]. The adjacent nucleus pulposus may later herniate through the fractured endplate resulting in anterior vertebral column insufficiency, progressive collapse and finally failure [3]. The introduction of percutaneous kyphoplasty (BK) and PMMA in the fractured vertebral body was an advent in transpedicular fractured endplate reduction and augmentation that theoretically should prevent failure of posterior short pedicle screw fixation due to progressive vertebral body collapse and reoperation [5, 6]. Such an augmentation seems to have a beneficial effect to the discs adjacent to an A3/AO-type fracture, managed with pedicle screw fixation plus endplate restoration, since no significant degeneration occurs 12–18 months post-injury [5].
Traditional open pedicle screw insertion includes a posterior traumatic midline approach resulting in blood loss, pain and slow recovery because of the extensive paravertebral muscles stripping [6]. Contemporary minimally invasive approaches through key-hole skin incisions and longitudinal muscle-splitting is increasingly used by spine surgeons to reduce trauma, back pain and blood loss [7–9].
Several recent studies have raised concern that minimally invasive techniques may have a higher incidence of inaccurate pedicle screw fixation and potential for neurologic lesion, [10] and higher rate of violation by pedicle screw thread of unfused facet joint than open approaches [11]. Continued motion at the violated facet joint and/or rods could theoretically lead to accelerated facet degeneration, and subsequently to early adjacent segment degeneration [11].
Despite the plethora of peer reviewed papers regarding minimally invasive surgery for thoracolumbar fractures, each reporting only few parameters to our knowledge; there are no studies reporting on most of the established parameters associated with MIS. This study reports on the alterations of primary (posttraumatic vertebral body deformity and pain intensity) and secondary (PMMA leakage, screw misplacement, facet violation, loss of correction, reoperation rate) outcome measures associated with percutaneous hybrid reduction and short-segment fixation plus BP with PMMA for severely compressed A2, A3 and B2 AO/Margel type, fresh thoracolumbar single traumatic fractures.
Methods
We retrospectively reviewed 36 prospectively selected consecutive patients aged >18 years, who underwent percutaneous instrumented thoracolumbar instrumentation (MIS) with cannulated multiaxial pedicle screws plus balloon kyphoplasty (BK) with PMMA for fresh single thoracolumbar vertebral fractures. The operations were performed between January 2012 and October 2013 by one senior spine surgeon in one institution. The selection/inclusion criteria were patients with fresh, single-level severely compressed A2 (>20 % loss of anterior vertebral height loss), A3, and B2 AO-type fractures and patients operated either with traditional open surgery or combined with anterior surgery; the exclusion criteria were: previous surgery in the area of interest, neurologic impairment (ASIA A to D) related to trauma, and multilevel injuries. There were 17 men and 16 women, aged (average ± SD) of 59 ± 17 years (range 18–86 years), with a BMI (average ± SD) of 28 ± 4.5, with 19 A3, 12A2 and 5B2 AO-type fractures, who underwent percutaneous BK at the fracture level and pedicle screw fixation at the immediately above and below the fractured vertebrae. Institutional review board approval was obtained for this study.
Functional outcome measures
Visual Analogue scale (VAS, 0–10 scale) was the single functional outcome measure used for the evaluation of patients.
Radiological outcome measures
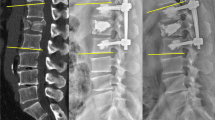
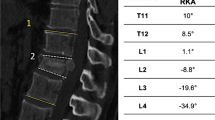
On digital roentgenograms, several roentgenographic parameters were measured: segmental vertebral kyphosis (angle formed from the lines drawn on the upper endplate of the cranial adjacent vertebrae and the lower endplate of caudal adjacent intact vertebra); anterior vertebral body height ratio (AVBHr) (vertebral body height of the fractured vertebra divided by the average of vertebral body height of the adjacent intact vertebrae); middle vertebral body height ratio (MVBHr) and posterior vertebral body height ratio (PVBHr). Preoperative and postoperative CT-scan in 0.6 mm slices were taken in all patients to evaluate spinal canal encroachment, pedicle screw position within the vertebral pedicle (grades I = medial marginal intracanal position, II = medial partial intracanal position, III = intracanal malposition) and facet joint violation (grades I–III) as well as early adjacent segment degeneration (ASD) were recorded. On axial CT-scan views: anteroposterior spinal canal encroachment [length of spinal canal occupied by the retropulsed vertebral bone divided by the average of anteroposterior spinal canal diameter of the two adjacent intact vertebrae × 100] (SCE) were measured preoperatively, and postoperatively (Fig. 2).
a Preoperative (admission) sagittal spinal CT-scan image in a female 36-year-old patient showing severe comminution (A3/AO-type) of the L 1 vertebral body associated with spinal canal encroachment and segmental kyphosis. b Postoperative sagittal standing roentgenogram of the patient in a showing excellent correction of segmental kyphosis. Extravertebral PMMA leakage is evident without neurological impairment or complaints
a Preoperative axial CT image of the patient in Fig. 1a showing severe vertebral body comminution (LSC score = 8). b Postoperative CT-scan image of the patient in Fig. 1a 1 year postoperatively showing an excellent spinal canal remodelling at the fracture level. The presence of PMMA did not interfere vertebral body bone remodelling
The accuracy of each pedicle screw placement in relation to midaxis of the pedicle was objectively evaluated on axial CT scans slice using Youkilis et al. classification [12] that divides the pedicle violations into three grades: grade I, screws within the pedicular cortical margin; grade II, screws that extended <2 mm beyond the pedicular cortex; and grade III, screws that extended ≥2 mm beyond the pedicular cortex.
For evaluation of facet violation on axial CT-scan slices, the Jones-Quaidoo SM et al. classification (grade I–III) was used; pedicle screws were graded as intraarticular if screw threads were clearly interposed between the superior facet of the injured vertebra and inferior articular processes of the facet joint in question (not injured adjacent vertebra), or if the screw actually first entered the inferior articular process, traversed the joint, and then entered the superior articular process and pedicle [13]. If a screw entered the superior articular process lateral to the joint and remained extraarticular throughout its course, it was graded as extraarticular. The load sharing classification (LSC) score was used to preoperatively evaluate the degree of injured vertebra comminution [14]. Digital roentgenograms and CT scans were evaluated by an unbiased orthopaedic spine surgeon and a senior orthopaedic radiologist who did not participated in surgeries.
Preoperative to postoperative oblique plain roentgenograms and CT scans of the spine were used to evaluate preoperatively to postoperatively the degree of adjacent segment degeneration.
Surgical technique
Under general endotracheal anaesthesia all patients were operated in prone position on Acromed frame. Continuous neuromonitoring and biplane fluoroscopy control were intraoperatively applied in all patients. The spontaneous reposition of the posttraumatic segmental kyphosis after lying on the Acromed frame was controlled on a lateral view taken with image intensifier. The pedicle screw instrumentation construct included one intact adjacent vertebra immediately above and one intact adjacent vertebra below the fractured vertebra. The fractured vertebra is augmented with PK and PMMA bone cement. A targeting cannulated needle for each pedicle of the instrumented adjacent vertebrae is used for initial insertion into the stab wound to locate the pedicle. K-wires of 2 mm are then passed through the needle, and all additional instruments and screws are taken from the K-wire. Multiaxial fully cannulated pedicle screws (5.5–6.5 mm) were placed with extender sleeves in down into the pedicles of the non-fractured vertebrae above and below the fractured vertebra, and subsequently all 4 K-wires were removed. After insertion of all four screws, the fractured vertebra augmentation was performed. Selecting the appropriate rod length with rod callipers and appropriate contouring of the rod, it was inserted through the stab wound for end screw extender sleeve (end vertebra) and the position was controlled with image intensifier. Reduction of the rod into the screw tulip is finally done using reducer. The closure top is tightened in all screws. Local anestheticum was injected into the superficial fascia. All patients received a custom made brace for 6 weeks.
Statistical analysis
Statistical analysis was performed using the MS Office Microsoft Excel software package. All data were presented as average ± SD. Paired t test was used to compare data derived from study subjects who have been measured at two time points.
Pearson correlation coefficient was used to compare different parametric parameters. Differences were considered significant at p < 0.05. Although all images (roentgenograms and CT scans) were digital which means low interobserver variability, the evaluation of interobserver agreement was considered as necessary to increase the scientific value of this study; this is because radiological measurements of vertebral body deformation before and following surgery was one of the two primary outcome measures in this study. This was performed using the kappa statistic or kappa coefficient. Two orthopaedic surgeons separately evaluated the same CT scans views from 15 randomly selected spines for displaced versus non-displaced screws and BMI only. The measured kappa values between the two observers were compared and kappas between 0.61 and 0.80 were considered as “substantial agreement”. Since in judging screw position in the sagittal images was found fair (κ value = 0.39) by Schizas et al. [10] the consensus interpretation was used in reporting screw placement in only the axial images [10].
Results
Operation duration averaged 68 ± 21 min, (range 40–100 min).
The fluoroscopy time per surgery was 3 ± 1 s, range 1.25–5.8 s. The cumulative irradiation dose per surgery was 6.5 ± 5 mGy, range 1.13–19 mGy.
The hospital stay averaged 2 days. No transfusion was made in any patient.
The patients were followed for an average of 31 ± 7 months (range 24–44 months) postoperation.
Functional outcomes
VAS significantly decreased from 7.86 ± 0.68 on admission to 1.65 ± 2.1 (p < 0.001) 3 months postoperatively, while no further changes (1.8 ± 1.65) were shown at the final evaluation.
Radiological outcomes
There was substantial interobserver agreement in judging pedicle screw position in all reconstructed CT images and roentgenograms (κ = 0.78–0.66) for axial pedicle screw position and facet violation plus fusion, respectively.
Preoperative LSC score averaged 6 ± 1 (range 5–8).
The changes of the radiological, CT-scan and functional parameters are demonstrated in the Table 1.
There was a nonsignificant average loss of kyphosis correction of 3.3° (p = 0.57) between the 3 months postoperatively and final kyphosis value (Table 1).
Complications
15 (10 %) screws in 13 patients were considered in axial CT images as malpositioned in relation to the longitudinal axis of the pedicle: six (4 %) screws in 5 pts. were considered as Grades II and six (4 %) screws in 5 pts. as grades III. Pedicle violation most commonly occurred in T 11 = 6; L 4 = 3; L 1 = 2 and L 2 = 1 vertebra. No correlation was found between number of malpositioned screws and BMI (r = 0.01). Two patients (2 grades III malpositioned screws) reported postoperatively discomfort in the ipsilateral lower extremity without evident neurologic deficit.
Intraarticular adjacent segment facet violation by the pedicle screws was disclosed in axial CT images in eight (5.5 %) facet joints, five patients. Facet joint violation most often occurred in T 11 = 6; L 1 = 2; L 4 = 3 and L 2 = 1 vertebra.
Asymptomatic PMMA leakage without sequela was recorded in axial CT images in 5 (14 %) fractured vertebral bodies, extracanal in 4 (11 %) and intracanal in one (3 %). PMMA leakage most commonly recorded in A3 AO-type (4 cases), and B2 AO-type (1 case) fractures with an average LSC score 6 (range 5–7). Intracanal PMMA leakage occurred in a 77-year-old female patient with an T12 A3 AO-type fracture and LSC = 7 without neurologic complications.
Adjacent joint degeneration at the violated by screw facet was shown in 2 (5.5 %) patients, respectively, 1 year postoperation.
Spontaneous interfacet fusion within the instrumentation area at the 1 year f/up occurred in 10/36 (28 %) patients.
Reoperations
Three patients (8 %) included in this study were reoperated for different reasons: one patient for symptomatic medial screw malposition; one patient for superficial infection; and one patient because of young age. In particular, the parents of a 18-year-old patient with a L 1 fracture have requested removal of the hardware 6 months postoperation because of his child’s young age and possible adverse effects by the implants onto the spine growth.
Discussion
Both primary and secondary outcome measures were fulfilled by the main findings in this clinical study. In particular, the primary outcome measures in this cohort: vertebral body heights and segmental kyphosis were significantly restored postoperatively by the hybrid fixation, and preoperative pain decreased, all significantly. Regarding the secondary outcome measures: asymptomatic PMMA leakage was radiologically shown in five (14 %) cases with only one (3 %) intracanal leakage that occurred solely in A3 and B2 fractures with significant comminution; accidental adjacent facet violation by the screws was shown in five patients in eight (5.5 %) facets; pedicle screw misplacement grades III occurred in six patients; the reoperation rate for different reasons (screw malposition, young age and infection) was 8 % (three patients). No radiological loss of correction was shown at the latest follow-up. Furthermore, although no bone graft was used, radiological spontaneous interfacet fusion rate was shown in 28 % cases.
Percutaneous spinal fixation is regarded by most surgeons as an advent in operative treatment of spinal fractures since it is associated with less surgical time, less blood loss and blood transfusion, lower potential for infection and pain compared with open traditional approaches [5, 6, 8, 9]. In this series, the operative time averaged 68 min, within the reported range from 22 to 85 min [7, 15].
Deep infection that requires instrumentation removal was reported in 1.5 % of the percutaneous surgical cases [7, 15, 16], significantly lower than the 3–10 % rate associated with open procedures [17]. In the present series, there was no deep infection.
However, some disadvantages of percutaneous surgery, e.g., pedicle screw malposition and potential for neural tissue damage have been reported. Although the reported pedicle violation by the screws ranged a lot (1.6–23 %) [10, 11, 18] the cases required revision for neurological complications ranged from 0 to 9 per study [19, 20]. In our cohort, only 6 (4 %) screws showed significant pedicle walls violations (grades III), whereas in only one patient pedicle screw removal for associated complaints was percutaneously made. The pedicle screw malposition rate in contrast to previous studies [10] was not correlated with the patient’s BMI index.
The need for addition of posterolateral fusion in spine fractures is debated. Some authors who removed instrumentation in not-fused spines observed asymptomatic mid-term loss of kyphosis correction [21]. Some loss, although insignificant, of segmental kyphosis was observed in our series that, however, should have been occurred at the disc levels. It is impressive that although no bone graft was used in our patients, spontaneous fusion occurred in about one third of the cases. If this spontaneous interfacet fusion is the result of immobilization or of facet violation or both cannot be elucidated from the findings of this study.
Loss of correction in instrumented thoracolumbar injuries is related to fracture type (A2–B2 AO-type) and the degree of vertebral body comminution. To avoid loss of correction it is recommended either anterior spine reconstruction [14, 15, 17], or short-segment pedicle screws plus vertebral body augmentation when LSC score >7 [9]. The reported loss of correction in short-segment fixation in such fractures averaged 4◦ that is comparable to that reported for open posterior approaches for this type of fractures [8, 9, 18, 19, 22–24]. The 3.3° loss of segmental kyphosis correction in our series was insignificant and within the previously reported.
An important consideration in all instrumented pedicle screw cases is preventing the development of adjacent level disease (ASD) by limiting injury to the adjacent level facets. A previous clinical study reported 24–100 % facet joint violation rates in open [25], while other studies reported 11–50 % violation rates for percutaneous procedures [11, 26]. In the present series, facet violation occurred, much lower than that reported, in eight (5.5 %) facet joints in five patients in all cases asymptomatic.
The study has several relevant limitations: first, the sample size of the series was small (no power analysis was made); second, it was not comparative; third, it was one surgeon’s series experience, and hence, it had a rather limited follow-up in terms of assessing an implant-based (pedicle screws plus BK) therapy.
Conclusively, this clinical study showed that percutaneous short-segment posterior fixation plus vertebrae augmentation for the treatment of acute traumatic thoracolumbar Type A2, A3, and B2 fractures is safe and efficient in medium-term follow-up with several of no clinical importance complications.
References
Rajasekaran S, Vaccaro AR, Kanna RM, Schroeder GD, Oner FC, Vialle L, Chapman J, Dvorak M, Fehlings M, Shetty AP, Schnake K, Maheshwaran A, Kandziora F (2016) The value of CT and MRI in the classification and surgical decision-making among spine surgeons in thoracolumbar spinal injuries. Eur Spine J. doi:10.1007/s00586-016-4623-0
Barcelos AC, Joaquim AF, Botelho RV (2016) Reliability of the evaluation of posterior ligamentous complex injury in thoracolumbar spine trauma with the use of computed tomography scan. Eur Spine J 25:1135–1143. doi:10.1007/s00586-016-4377-8 (Epub 2016 Jan 25)
McLain RF, Sparling E, Benson DR (1993) Early failure of short-segment pedicle instrumentation for thoracolumbar fractures. A preliminary report. J Bone Joint Surg Am 75:162–167
Esses SI, Botsford DJ, Wright T, Bednar D, Bailey S (1991) Operative treatment of spinal fractures with the AO internal fixator. Spine (Phila Pa 1976) 16:S146–S150
Mahar A, Kim C, Wedemeyer M, Mitsunaga L, Odell T, Johnson B, Garfin S (2007) Short-segment fixation of lumbar burst fractures using pedicle fixation at the level of the fracture. Spine (Phila Pa 1976) 32:1503–1507
Gu Y, Zhang F, Jiang X, Jia L, McGuire R (2013) Minimally invasive pedicle screw fixation combined with percutaneous vertebroplasty in the surgical treatment of thoracolumbar osteoporosis fracture. J Neurosurg Spine 18:634–640
Merom L, Raz N, Hamud C, Weisz I, Hanani A (2009) Minimally invasive burst fracture fixation in the thoracolumbar region. Orthopedics 32:273–278
Korovessis P, Vardakastanis K, Repantis T et al (2014) Transpedicular vertebral body augmentation reinforced with pedicle screw fixation in fresh traumatic A2 and A3 lumbar fractures: comparison between two devices and two bone cements. Eur J Orthop Surg Traumatol (France) 24(Suppl 1):S183–S191
Jia Q, Hu L, Yu Y et al (2015) Balloon vertebroplasty combined with short-segment pedicle screw instrumentation for treatment of thoracolumbar burst fractures. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi (China) 29(6):741–745
Schizas C, Michel J, Kosmopoulos V, Theumann N (2007) Computer tomography assessment of pedicle screw insertion in percutaneous posterior transpedicular stabilization. Eur Spine J 16:613–617
Knox JB, Dai JM 3rd, Orchowski JR (2011) Superior segment facet joint violation and cortical violation after minimally invasive pedicle screw placement. Spine J 11(3):213–217
Youkilis AS, Quint DJ, McGillicuddy JE, Papado-poulos SM (2001) Stereotactic navigation for placement of pedicle screws in the thoracic spine. Neurosurgery 48:771–778
Jones-Quaidoo SM, Djurasovic M, Owens RK 2nd, Carreon LY (2013) Superior articulating facet violation: percutaneous versus open techniques. J Neurosurg Spine 18(6):593–597
McCormack T, Karaikovic E, Gaines RW (1994) The load sharing classification of spine fractures. Spine (Phila Pa 1976) 19:1741–1744
Ni WF, Huang YX, Chi YL, Xu HZ, Lin Y, Wang XY et al (2010) Percutaneous pedicle screw fixation for neurologic intact thoracolumbar burst fractures. J Spinal Disord Tech 23:530–537
Palmisani M, Gasbarrini A, Brodano GB, De Iure F, Cappuccio M, Boriani L et al (2009) Minimally invasive percutaneous fixation in the treatment of thoracic and lumbar spine fractures. Eur Spine J 18:71–74
Rechtine GR, Bono PL, Cahill D et al (2001) Postoperative wound infection after instrumentation of thoracic and lumbar fractures. J Orthop Trauma 15:566–569
Knight RQ (2009) Minimally invasive spine surgery. Curr Orthop Pract 20:227–231
Korovessis P, Hadjipavlou A, Repantis T (2008) Minimal invasive short posterior instrumentation plus balloon kyphoplasty with calcium phosphate for burst and severe compression lumbar fractures. Spine 33:658–667
Khoo LT, Palmer S, Laich DT, Fessler RG (2002) Minimally invasive percutaneous posterior lumbar interbody fusion (see comment). Neurosurgery 51:S166–S171
Yang H, Shi JH, Ebraheim M, Liu X, Konrad J, Husain I (2011) Outcome of thoracolumbar burst fractures treated with indirect reduction and fixation without fusion. Eur Spine J 20:380–386
Afzal S, Akbar S, Dhar SA (2008) Short segment pedicle screw instrumentation and augmentation vertebroplasty in lumbar burst fractures: an experience. Eur Spine J 17:336–341
Verlaan JJ, van Helden WH, Oner FC et al (2002) Balloon vertebroplasty with calcium phosphate cement augmentation for direct restoration of traumatic thoracolumbar vertebral fractures. Spine 27:543–548
Verlaan JJ, Dhert WAJ, Verbout AJ, Oner C (2005) Balloon vertebroplasty in combination with pedicle screw instrumentation: a novel technique to treat thoracic and lumbar burst fractures. Spine 30(3):73–79
Chen Z, Zhao J, Xu H, Liu A, Yuan J, Wang C (2008) Technical factors related to the incidence of adjacent superior segment facet joint violation after transpedicular instrumentation in the lumbar spine. Eur Spine J 17(11):1476–1480
Zeng ZL, Jia L, Xu W, Yu Y, Hu X, Jia YW, Wang JJ et al (2015) Analysis of risk factors for adjacent superior vertebral pedicle-induced facet joint violation during the minimally invasive surgery transforaminal lumbar interbody fusion: a retrospective study. Eur J Med Res 20:80
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Korovessis, P., Mpountogianni, E. & Syrimpeis, V. Percutaneous pedicle screw fixation plus kyphoplasty for thoracolumbar fractures A2, A3 and B2. Eur Spine J 26, 1492–1498 (2017). https://doi.org/10.1007/s00586-016-4743-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4743-6