Abstract
Purpose
To verify whether pelvic incidence (PI) would change in adult spinal deformity (ASD) patients who underwent long instrumentation using S2-alar-iliac (S2AI) screws and to identify factors associated with the change in PI.
Methods
We retrospectively reviewed all patients who underwent spinal surgery using S2AI screws between November 2014 and January 2017 at our institution. Patients aged 20 years or above with available radiographs were included. According to the change in PI, patients were divided into two groups, group C: PI variance reached 5 or more degrees postoperatively and group NC: PI changed less than 5°.
Results
A total of 47 patients (3 males, 44 females; mean age, 52.47 ± 15.80 years) were included in this study. PI significantly decreased from 51.25° ± 14.80° to 40.43° ± 14.23° in group C (n = 26), with a mean change in 11.52° ± 6.17° (P < 0.05), but changed from 47.00° ± 13.18° to 46.57° ± 13.71° in group NC without statistical significance. Intergroup analysis showed that change in PI, preoperative PI–LL, preoperative LL, preoperative SVA, and postoperative PT were significantly different between both groups. Correlation analysis showed that the change in PI and preoperative LL and PI were significantly associated. The formula provided by the regression analysis was ΔPI = − 3.108 − 0.11PreLL + 0.211PrePI.
Conclusions
Our study showed that PI decreased in 55% of ASD patients after spinal surgery using S2AI screws. Greater preoperative PI–LL mismatch and PI, as well as lumbar kyphosis, were associated with postoperative change in PI.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The human pelvis, which articulates with the spine and inferior extremity, is tremendously important in the development of verticality. It is crucial to define the pelvic geometry in order to investigate the interaction between the spine and inferior extremity. Pelvic incidence (PI), which was defined by Duval-Beaupère et al. [1], enables the correlation between pelvic form and function and is traditionally considered a morphological value that remain constant after maturity. The interaction between the pelvis and spine plays an important role in regulating spinal sagittal alignment [2,3,4]. As a constant value, PI is said to be the only signature of the initial situation that can reveal the original anatomy of the spinopelvic complex [5]. Because of this unique characteristic, PI is used to evaluate sagittal alignment based on formulas such as PI minus lumbar lordosis (LL) [6, 7].
However, there is a new point of focus on spinopelvic parameters. A randomized prospective study funded by the Scoliosis Research Society showed that PI varies in a high percentage of healthy subjects [8]. A cross-sectional study performed by Cecchinato et al. [9] reported that PI decreased during the early postoperative in adult spinal deformity (ASD) patients who underwent long fusion to the sacrum with pelvic fixation. Bao et al. [10] reported that lumbosacral stress and age may contribute to increased PI and that spinal malalignment may be associated with the discrepancy in change in PI. All these studies that reported the change in PI implied a similar hypothesis: the laxity of the sacroiliac joint leads to a relative sacral motion with respect to the pelvis, and motion at the sacroiliac joint may affect the PI value [11,12,13].
In only few studies that have reported the change in PI after surgery, the change in PI was relatively small, the pelvic fixation technique utilized in patients was not homogeneous, which may bias the results, and factors associated with the change in PI have not been well investigated. The trajectory of S2-alar-iliac (S2AI) screw placement starts from the sacrum, with the screws placed across the sacroiliac joint and into the ilium. This study aimed to investigate whether PI would change postoperatively in ASD patients who underwent S2AI screw placement and to identify possible factors associated with the change in PI.
Materials and methods
Subjects
This retrospective case series study was approved by the institutional review board of our hospital. Informed consent was obtained from all patient included in this study. ASD patients who underwent long fusion using S2AI screws between November 2014 and January 2017 were retrospectively reviewed to investigate whether the laxity of the sacroiliac joint affected the PI value. Patients (1) aged 20 years or above at the year of surgery who underwent (2) bilateral placement of S2AI screws and (3) long arthrodesis involving five or more levels and who had (4) available standing posteroanterior and lateral radiographs obtained preoperatively and postoperatively were included in this study [14]. Patients with prior history of spinal or pelvic surgery and nonambulatory patients were excluded from the study.
Radiographic evaluation
Standing posteroanterior and lateral radiographs of the spine were preoperatively and postoperatively evaluated. The prevalence of sacroiliac joint degeneration was evaluated on the posteroanterior radiograph according to a previous study [15]. All parameters were measured by two senior spinal surgeons, and mean values were used for analysis. After 6 months, the same two surgeons re-measured the preoperative and postoperative PI independently and were blinded to patient details. The following radiographic parameters were measured using a validated software (Surgimap, Nemaris, Inc., New York, NY) [16]:
-
1.
PI the angle subtended by a perpendicular line from the upper endplate of S1 and a line connecting the center of the femoral head to the center of the upper endplate of S1.
-
2.
Pelvic tilt (PT) the angle between the line connecting the midpoint of the sacral plate to the femoral head axis and the vertical axis.
-
3.
Sacral slope (SS) the angle between the superior plate of S1 and a horizontal line.
-
4.
Sagittal vertical axis (SVA) the distance from the C7 plumb line to the perpendicular line drawn from the superior posterior endplate of the S1 vertebral body.
-
5.
LL the angle between the lower endplate of T12 and the upper endplate of S1.
-
6.
PI–LL postoperative PI minus postoperative LL.
Changes in PI, SVA, and LL were then calculated by subtracting the preoperative values from the postoperative values. According to the change in PI, ASD patients were divided into three groups: group A (a decrease in PI of > 5°), group B (a change in PI between − 5° and 5°), and group C (an increase in PI of > 5°). As no patient had an increase in PI of > 5° postoperatively, we then divided the patients into two subgroups: changed group (group C) in whom the decrease in PI was ≥ 5° postoperatively and non-changed group (group NC) in whom the change in PI was < 5°. The cutoff value was determined as 5° because deviation may occur owing to varied posture during imaging and measurement [17].
Statistical analysis
Statistical analysis was performed using SPSS version 17.0 (SPSS Inc., Chicago, IL). All values were expressed as mean ± standard deviation. Paired Student’s t tests were performed to assess the perioperative changes in radiographic parameters between the two groups. Independent-samples t test was used for intergroup comparison of continuous variables and analysis of the differences between groups C and NC. Correlation tests were performed to analyze the correlation between each radiographic parameter and the change in PI, thus serving as preliminary screening tools to select the possible candidates (P < 0.05) for regression analysis. Linear regression model was subsequently used to analyze the covariate effects of possible indicators of the change in PI. Inter-observer and intra-observer reliability were assessed using intra-class correlation (ICC) coefficients. The following thresholds represent the quality of ICC > 0.90, excellent; 0.71–0.90, good; 0.51–0.70, fair; 0.25–0.49, low, and < 0.25, poor [18]. All reported P values were two-sided, and P < 0.05 was considered statistically significant.
Results
In this study, 47 ASD patients [3 males, 44 females; mean age, 52.47 ± 15.80 years (range 20–73 years)] were ultimately included and divided into two subgroups according to the postoperative change in PI. Of these patients, 26 were included in group C, whereas the remaining 21 were included in group NC.
Radiographic analysis
As shown in Table 1 and Figs. 1 and 2, PI significantly decreased from 51.25° ± 14.80° preoperatively to 40.43° ± 14.23° postoperatively in group C, with a mean change in 11.52° ± 6.17° (P < 0.05). In contrast, PI was 47.00° ± 13.18° preoperatively and 46.57° ± 13.71° postoperatively in group NC. The difference between preoperative and postoperative PI values was 0.43° ± 3.00° without statistical significance (P = 0.521). In group C, PT, SS, LL, and SVA significantly changed postoperatively (P < 0.05). However, in group NC, only PT, SS, and LL significantly changed postoperatively (P < 0.05), with SVA decreasing from 38.07 mm ± 32.86 mm preoperatively to 28.55 ± 21.26 mm postoperatively without statistical significance (P = 0.312).
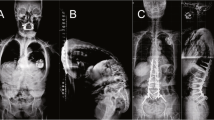
a, c Preoperative radiographs of patient who underwent long instrumentation using S2AI screws in group C (preoperative parameters: LL, − 9°; PI, 56°; PT, 41°; SS, 15°). b, d Postoperative radiographs (postoperative parameters: LL, 24°; PI, 40°; PT, 22°; SS, 18°). PI decreased from 56° preoperatively to 40° postoperatively. e, f The enlarged pictures of c and d
a, c Preoperative radiographs of patient who underwent long instrumentation using S2AI screws in group NC (preoperative parameters: LL, 21°; PI, 46°; PT, 26°; SS, 20°). b, d Postoperative radiographs (postoperative parameters: LL, 41°; PI, 44°; PT, 20°; SS, 24°). PI was 46° preoperatively and 44° postoperatively. e, f The enlarged pictures of c and d
Intergroup analysis showed that aside from the change in PI, preoperative PI–LL (54.12° ± 24.22° vs. 28.53° ± 26.48°, P = 0.001), preoperative LL (− 2.87° ± 23.45° vs. 18.47° ± 29.19°, P = 0.08), preoperative SVA (81.68 ± 94.60 vs. 38.07 ± 32.86 mm, P = 0.36), and postoperative PT (15.10° ± 9.85° vs. 21.52° ± 8.08°, P = 0.02) were significantly different between the two groups. Preoperative PT (32.10° ± 11.22° vs. 29.36° ± 8.82°, P = 0.366), preoperative SS (18.46° ± 15.36° vs. 17.60° ± 14.33°, P = 0.844), and postoperative SS (25.63° ± 9.14° vs. 25.05° ± 12.71°, P = 0.855) were similar between the two groups. Preoperative PI–LL and preoperative SVA were greater and preoperative LL was smaller in group C than in group NC (Table 1). Patients in group C had a significantly higher prevalence of sacroiliac joint degeneration than patients in group NC, with sacroiliac joint degeneration showing on the posteroanterior radiograph in 61.5% of patients in group C and 28.6% of patients in group NC (P = 0.024, Table 2). Inter- and intra-observer reliability analyses revealed excellent agreement (ICC > 0.9) for preoperative and postoperative PI (Table 3).
Correlation and regression analyses
Correlation and regression analyses were performed to determine potential factors associated with the decrease in PI. As shown in Table 4, the correlation analysis showed that preoperative PI–LL (r = 0.465, P = 0.01), preoperative LL (r = − 0.316, P = 0.03), and preoperative PI (r = 0.297, P = 0.043) were significantly associated with postoperative change in PI in ASD patients. Moreover, the regression analysis showed that preoperative LL and preoperative PI were associated factors, with an R2 of 0.250. The formula provided by the regression analysis was ΔPI = − 3.108 – 0.11 preoperative LL + 0.211 preoperative PI, indicating that ASD patients with greater PI and lumbar kyphosis preoperatively are more likely to have a greater postoperative decrease in PI (Table 5).
Discussion
PI is a morphological parameter that reflects the relation between the sacrum and both iliac wings. Although some studies reported that PI changes with skeletal growth [19], it is often considered a constant value after maturity [20]. However, several studies have questioned this characteristic of PI, claiming that PI may change under certain circumstances. Place et al. [8] supposed that PI changed when the pelvic position varied in healthy asymptomatic individuals probably because of potential functional motion at the sacroiliac joint. Bao et al. [10] speculated that PI increases with years owing to motion at the sacroiliac joint caused by lumbosacral stress. In addition, several studies showed that the increase in PI was attributed to the potential motion at the sacroiliac joint.
The change in PI has been observed in patients who underwent pelvic fixation in previous studies [9, 21]. However, the pelvic fixation technique used in these studies was not homogeneous. And the change in PI was relatively small which cannot exclude the measurement deviation; whether the laxity of the sacroiliac joint could affect PI remains unknown. Pelvic fixation using the S2AI screws through sacroiliac joint penetration and immobilization is currently widely used and is associated with fewer complications than traditional iliac screw fixation [22]. The results of the present study showed that PI dramatically changed after S2AI screw fixation in 55% (26/47) of ASD patients and decreased by 11.52° ± 6.17° in group C. Our results were consistent with those of previous studies. Cecchinato et al. [9] reported that PI decreased by 3.9° in patients in whom iliac screws were used. As PI value may also be influenced by whether the selection of the distal fusion is the sacrum or iliac, a decrease in PI may be due to the placement of iliac screws that has altered the morphology of the pelvis. Further, Ishida et al. [21] showed that PI decreased by 6° in patients in whom S2AI screws were utilized, claiming that there is a possible decrease in PI.
Our results showed that PI decreased more when ASD patients had lumbar kyphosis or had a greater PI preoperatively. This finding supports the previous hypothesis that sagittal spinopelvic malalignment may contribute to the change in PI [11]. Correlation and multivariate regression analyses showed that preoperative PI–LL mismatch was more significant in group C, indicating that sagittal malalignment may play an important role in the change in PI. In group NC, the PI changed by only 0.43° ± 3.00° without statistical significance. This observation may be explained by the fact that patients in group NC had a relatively smaller preoperative PI–LL mismatch and greater preoperative LL than those in group C. Previous studies reported that spinal malalignment may lead to an increased PI in patients with severe sagittal malalignment [10]. Moreover, pelvic retroversion generates a reaction force on the sacroiliac joint in patients with sagittal malalignment, destabilizing the joint, particularly in the presence of combined degeneration. Herein, the laxity of the sacroiliac joint serves as basis of the change in PI. Moreover, when applying the S2AI screws, it will change and reconstruct the sacroiliac joint, which may also affect the value of PI. Briefly, PI postoperatively decreases probably because PI has already preoperatively increased during degeneration [10].
Our study implies that the decrease in PI may be attributed to the laxity of the sacroiliac joint at least in part because of sagittal malalignment. During the surgery, the S2AI screws were placed through the sacroiliac joint, reconstructing the morphology of pelvis. As a consequence, we observed the dramatic decrease in PI. The discrepancy in postoperative change in PI reported by other studies indicates that the potential mechanism may be related to multiple factors. Ishida et al. [21] compared the spinopelvic parameters between ASD patients who underwent S2AI screw fixation and iliac screw fixation and showed that PI remained unchanged in the iliac screw fixation group. However, they also claimed that there is a possible reduction of PI in the S2AI screw fixation group. PI remained unchanged in the iliac screw fixation group probably because these patients had residual motion at the sacroiliac joint. In our study, PI decreased in 55% of patients, with a mean change in PI of 11.52° ± 6.17° in group C. The dramatic decrease in PI in our study may be attributed to the fact that the major pathology in our patients was degenerative scoliosis and patients in group C had severe sagittal malalignment and that we divided ASD patients into two subgroups based on the postoperative change in PI. In contrast, in the study of Ishida et al., 84.8% of patients in the S2AI screw fixation group had a history of prior lumbosacral surgery, and their preoperative PI–LL mismatch was smaller than those patients in group C in our study.
Restoring sagittal balance in ASD patients is crucial to achieving a satisfying clinical outcome. The formula PI–LL = ± 10° is widely applied to help predict the optimal LL for patients. Although this formula provides good clinical assessment in the representative majority of ASD patients, it seems be limited in the elderly or the young patients [23]. Lafage et al. provided an age-adjusted spinopelvic alignment values that correlated with satisfactory patient-reported outcomes [24]. In some ASD patients, LL was overcorrected past the thresholds dictated by the age-adjusted formula. Moreover, overcorrection appeared to be greater in cases where PI value decreased postoperatively. This suggests that in patients with lumbar kyphosis and large PI, clinicians should be aware of possible postoperative PI reduction, and that PI–LL value may be different from the predicted value.
To the best of our knowledge, our study first observed significant PI decrease postoperatively in 55% ASD patients who utilized S2AI screws. The dramatic change in PI in our study may be due to the categorization of homogenous patients into two subgroups. Our results remind us to reconsider the role of PI in developing surgical plans and evaluating clinical outcome. Our study has several limitations. Firstly, the relatively small study cohort may lead to biased results. Secondly, the anatomical change at the sacroiliac joint needs to be confirmed through computed tomography, which was not available to all patients owing to ethnical concerns. Thirdly, this study is limited by its retrospective nature. The majority of the patients enrolled in this study were female and relatively young, with a wide range of ages. Future longitudinal studies are required to further investigate the change in PI.
Conclusion
In conclusion, our study showed that PI dramatically decreased in 55% of ASD patients after spinal surgery using S2AI screws. Greater preoperative PI–LL mismatch and PI, as well as lumbar kyphosis, were associated with postoperative change in PI.
References
Duval-Beaupere G, Schmidt C, Cosson P (1992) A Barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng 20:451–462
Legaye J, Duval-Beaupere G, Hecquet J, Marty C (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7:99–103
Berjano P, Langella F, Ismael MF, Damilano M, Scopetta S, Lamartina C (2014) Successful correction of sagittal imbalance can be calculated on the basis of pelvic incidence and age. Eur Spine J 23(Suppl 6):587–596. https://doi.org/10.1007/s00586-014-3556-8
Schlosser TP, Janssen MM, Vrtovec T, Pernus F, Oner FC, Viergever MA, Vincken KL, Castelein RM (2014) Evolution of the ischio-iliac lordosis during natural growth and its relation with the pelvic incidence. Eur Spine J 23:1433–1441. https://doi.org/10.1007/s00586-014-3358-z
Roussouly P, Pinheiro-Franco JL (2011) Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. Eur Spine J 20:609–618. https://doi.org/10.1007/s00586-011-1928-x
Schwab FJ, Blondel B, Bess S, Hostin R, Shaffrey CI, Smith JS, Boachie-Adjei O, Burton DC, Akbarnia BA, Mundis GM, Ames CP, Kebaish K, Hart RA, Farcy JP, Lafage V (2013) Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976) 38:E803–E812. https://doi.org/10.1097/brs.0b013e318292b7b9
Schwab F, Ungar B, Blondel B, Buchowski J, Coe J, Deinlein D, DeWald C, Mehdian H, Shaffrey C, Tribus C, Lafage V (2012) Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976) 37:1077–1082. https://doi.org/10.1097/brs.0b013e31823e15e2
Place HM, Hayes AM, Huebner SB, Hayden AM, Israel H, Brechbuhler JL (2017) Pelvic incidence: a fixed value or can you change it? Spine J. https://doi.org/10.1016/j.spinee.2017.06.037
Cecchinato R, Redaelli A, Martini C, Morselli C, Villafane JH, Lamartina C, Berjano P (2017) Long fusions to S1 with or without pelvic fixation can induce relevant acute variations in pelvic incidence: a retrospective cohort study of adult spine deformity surgery. Eur Spine J. https://doi.org/10.1007/s00586-017-5154-z
Bao H, Liabaud B, Varghese J, Lafage R, Diebo BG, Jalai C, Ramchandran S, Poorman G, Errico T, Zhu F, Protopsaltis T, Passias P, Buckland A, Schwab F, Lafage V (2017) Lumbosacral stress and age may contribute to increased pelvic incidence: an analysis of 1625 adults. Eur Spine J. https://doi.org/10.1007/s00586-017-5324-z
Jean L (2014) Influence of age and sagittal balance of the spine on the value of the pelvic incidence. Eur Spine J 23:1394–1399. https://doi.org/10.1007/s00586-014-3207-0
Charles YP, Yu B, Steib JP (2016) Sacroiliac joint luxation after pedicle subtraction osteotomy: report of two cases and analysis of failure mechanism. Eur Spine J 25(Suppl 1):63–74. https://doi.org/10.1007/s00586-015-4094-8
Park S-A, Kwak D-S, Cho H-J, Min D-U (2017) Changes of spinopelvic parameters in different positions. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-017-2757-0
Jain A, Hassanzadeh H, Strike SA, Menga EN, Sponseller PD, Kebaish KM (2015) Pelvic fixation in adult and pediatric spine surgery: historical perspective, indications, and techniques—AAOS exhibit selection. J Bone Jt Surg Am 97:1521–1528. https://doi.org/10.2106/jbjs.o.00576
O’Shea FD, Boyle E, Salonen DC, Ammendolia C, Peterson C, Hsu W, Inman RD (2010) Inflammatory and degenerative sacroiliac joint disease in a primary back pain cohort. Arthritis Care Res 62:447–454. https://doi.org/10.1002/acr.20168
Lafage R, Ferrero E, Henry JK, Challier V, Diebo B, Liabaud B, Lafage V, Schwab F (2015) Validation of a new computer-assisted tool to measure spino-pelvic parameters. Spine J 15:2493–2502. https://doi.org/10.1016/j.spinee.2015.08.067
Tyrakowski M, Wojtera-Tyrakowska D, Siemionow K (2014) Influence of pelvic rotation on pelvic incidence, pelvic tilt, and sacral slope. Spine (Phila Pa 1976) 39:E1276–E1283. https://doi.org/10.1097/brs.0000000000000532
Hardesty CK, Aronson J, Aronson EA, Ranade AS, McCracken CW, Nick TG, Cordell CL (2013) Interobserver variability using a commercially available system of archived digital radiography with integrated computer-assisted measurements for scoliosis Cobb angles. J Pediatr Orthop 33:163–169. https://doi.org/10.1097/BPO.0b013e3182770bd3
Schwab F, Lafage V, Patel A, Farcy JP (2009) Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976) 34:1828–1833. https://doi.org/10.1097/brs.0b013e3181a13c08
Le Huec JC, Demezon H, Aunoble S (2015) Sagittal parameters of global cervical balance using EOS imaging: normative values from a prospective cohort of asymptomatic volunteers. Eur Spine J 24:63–71. https://doi.org/10.1007/s00586-014-3632-0
Ishida W, Elder BD, Holmes C, Lo SL, Goodwin CR, Kosztowski TA, Bydon A, Gokaslan ZL, Wolinsky JP, Sciubba DM, Witham TF (2017) Comparison between S2-alar-iliac screw fixation and iliac screw fixation in adult deformity surgery: reoperation rates and spinopelvic parameters. Global Spine J 7:672–680. https://doi.org/10.1177/2192568217700111
Elder BD, Ishida W, Lo SL, Holmes C, Goodwin CR, Kosztowski TA, Bydon A, Gokaslan ZL, Wolinsky JP, Sciubba DM, Witham TF (2017) Use of S2-alar-iliac screws associated with less complications than iliac screws in adult lumbosacropelvic fixation. Spine 42:E142–E149. https://doi.org/10.1097/BRS.0000000000001722
Faldini C, Di Martino A, De Fine M, Miscione MT, Calamelli C, Mazzotti A, Perna F (2013) Current classification systems for adult degenerative scoliosis. Musculoskelet Surg 97:1–8. https://doi.org/10.1007/s12306-013-0245-4
Lafage R, Schwab F, Challier V, Henry JK, Gum J, Smith J, Hostin R, Shaffrey C, Kim HJ, Ames C, Scheer J, Klineberg E, Bess S, Burton D, Lafage V (2016) Defining spino-pelvic alignment thresholds: should operative goals in adult spinal deformity surgery account for age? Spine (Phila Pa 1976) 41:62–68. https://doi.org/10.1097/brs.0000000000001171
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that they have no conflict of interest.
Additional information
Supported by the Nanjing Clinical Medical Center and Jiangsu Provincial Key Medical Center.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tseng, C., Liu, Z., Bao, H. et al. Long fusion to the pelvis with S2-alar-iliac screws can induce changes in pelvic incidence in adult spinal deformity patients: analysis of predictive factors in a retrospective cohort. Eur Spine J 28, 138–145 (2019). https://doi.org/10.1007/s00586-018-5738-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-018-5738-2