Abstract
Introduction
Pelvic incidence (PI) is a key morphological parameter that reflects the relation between the sacrum and iliac wings. It is well accepted that PI remains constant after reaching maturity. However, recent studies indicated that PI might be altered after lumbosacral fusion. Additionally, it remains uncertain on the long-term influence of long fusion to pelvis with S2-alar-iliac screw on PI in patients with adult spinal deformity (ASD).
Study Design
A retrospective study.
Objective
To investigate whether and how PI would change during the follow-up in ASD patients who underwent S2AI fixation and to identify factors associated with the change in PI.
Methods
We retrospectively reviewed all ASD patients who underwent spinal surgery using S2AI screws between November 2014 and January 2017 at our institution. Patients with minimum follow-up of two years were included. The following sagittal radiographic parameters were measured: PI, Lumbar lordosis (LL), pelvic tilt (PT), PI-LL, sagittal vertical axis (SVA) at pre-op, post-op and 2-year follow-up. According to the changes in PI at immediate post-operation, patients were classified into two groups; Group A: Changes of PI less than or equal 5° and Group B: Changes of PI greater than 5°.
Results
A total of 82 ASD patients (Group A: 32, Group B: 50; mean age of 53.5 ± 12.6 years) with a mean follow-up period of 30.2 ± 9.2 months were included in this study. At immediate post-operation, Group A showed no significant change in PI (45.7° ± 11.4° to 45.3° ± 11.2°, p = 0.749); while Group B had a significant decrease in PI (51.6° ± 14.5° to 40.9° ± 14.0°, p < 0.001). At the last follow-up, 48% patients (24/50) in Group B had a significant increase in PI (32.8° ± 6.4° to 45.8° ± 11.2°, p < 0.001). Intergroup analysis showed that ΔPI, post-op PI, post-op PT and age were significantly different between both groups. In addition, pre-op PI, post-op PI, post-op PT, post-op PI-LL were significantly correlated with ΔPI at last follow-up. Also, logistic regression analysis showed that post-op PI was the associated risk factor (OR = 0.865, p = 0.024) for PI-LL mismatch.
Conclusion
Our study showed that PI decreased in more than half of ASD patients immediately after spinal surgery using S2AI screws. Approximately 48% of them were able to recover during the 2-year follow-up. Lower pre-op PI, post-op PI and PT were found to be strongly associated with the return of PI. Thus, these current findings indicated that patients with a high PI at pre-operation should not be over-corrected to avoid PI-LL mismatch postoperatively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
PI is used to evaluate the interaction between the spine and lower limb, which facilitates to dictate the optimal sagittal alignment to achieve a satisfactory postoperative result in correction surgery for adult spinal deformity (ASD), as it is well accepted as a constant value after maturity [1]. However, recent studies have strongly challenged this classical concept [2]. Bao et al. [3] reported that lumbosacral stress and age may contribute to increase pelvic incidence (PI) and that spinal malalignment may be associated with the discrepancy in change in PI after surgery.
A randomized prospective study demonstrated that PI could vary in 80% subjects when they changed the pelvic position, which suggested a potential functional motion at the sacroiliac joint [4]. Our preliminary study concluded that PI decreased in 55% of ASD patients after long-fusion surgery using S2-alar-iliac (S2AI) screws [5]. Some authors postulated that the unexpected PI change in ASD patients could be due to sacroiliac joint laxity, S2AI screw placement, or aggressive sagittal cantilever technique [6] of PI. In addition, PI postoperatively decreased may be due to PI has already preoperatively increased during degeneration, which reminded us to reconsider the role of PI in developing surgical plans and evaluating clinical outcome [6]. Although the index for the changes of pelvic incidence with lumber lordosis (PI–LL = ± 10°) is widely applied to predict the optimal lumbar lordosis (LL) for corrective surgery, LL overcorrection appeared to be greater in cases where PI value decreased postoperatively [7].
In light of several studies have reported that PI changes after S2AI fixation, we hypothesized that the PI may still remain dynamic during the follow-up. However, there were few longitudinal studies reporting how PI would change during the follow-up. Therefore, the aim of this study was to investigate whether and how PI would change during the follow-up in ASD patients who underwent S2AI fixation and identify possible factors associated with the changes in PI.
Materials and methods
Subjects
This retrospective case series study was approved by the institutional review board of our hospital. Informed consent was obtained from all patients included in this study. Patients who underwent a long fusion to pelvis with S2-alar-iliac screw in our center (Department of Orthopedics at a local tertiary hospital) between January 2010 and January 2018 were retrospectively reviewed. Inclusion criteria included: Patients (1) who were diagnosed as adult spinal deformity (ASD), (2) with follow-up period longer than two years. Patients with a prior history of spinal or pelvic surgery and non-ambulatory patients were excluded from the study.
Radiographic evaluation
Standing posteroanterior and lateral radiographs of the spine were obtained at the initial and last visit in our clinic. All the radiographic parameters were measured by two senior spine surgeons (a surgeon with 5 years of experience and a senior surgeon with 10 years of experience). After 3 months, the same two surgeons re-measured the parameters independently and were blinded to patient details. Radiographic parameters were measured using a validated software (Surgimap, Nemaris, Inc., New York, NY). The following sagittal radiographic parameters were measured: PI, pelvic tilt (PT), sacral slope (SS), sagittal vertical axis (SVA), and LL. Meanwhile, changes in PI, PT, SS, LL, SVA and PT/PI were calculated by subtracting the initial values from the last visit values.
Mechanical complications were documented after surgery including proximal junctional kyphosis (PJK) or failure (PJF), distal junctional kyphosis or failure, rod breakage, and implant-related complications.
Statistical analysis
Statistical analysis was performed using SPSS version 22.0 (SPSS Inc., Chicago, IL). All values were expressed as mean ± standard deviation. Inter-observer and intra-observer reliability were assessed using intra-class correlation (ICC) coefficients.
According to the changes in PI at immediate post-operation, patients were classified into two groups; Group A = Changes of PI less than or equal 5° and Group B = Changes of PI greater than 5° [4, 5]. Toward Group B, they are further grouped based on PI recovering during follow-up: Group B1 = PI recovery greater than 5° and Group B2 = recovery equal or less than 5°. Changes in radiographic parameters between the initial and the last follow-up were assessed by Paired Student’s t-tests. Mann–Whitney test was used to evaluate intergroup parameters. Correlation tests were performed to analyze the correlation between each radiographic parameter and the change in PI. All P values were two-sided, and P < 0.05 was considered statistically significant.
Results
In this study, 82 ASD patients with a mean age of 53.5 ± 12.6 years (rang, 38–73 years) were enrolled in this study with a mean follow-up period of 30.2 ± 9.2 months (range, 24–96 months). The intra- and inter-observer ICCs for estimating the radiographic parameters were from 0.85 to 0.96, suggesting good to excellent reliability of these measurements among the two observers.
At post-operation, Group A showed no significant change in PI (45.7° ± 11.4° to 45.3° ± 11.2°, t = 0.326, p = 0.749); while Group B showed a significant decrease in PI from 51.6° ± 14.5° to 40.9° ± 14.0° (t = 9.911, p < 0.001) (Table 1). As compared with Group A, Group B had significantly lower pre-op LL (14.7° ± 22.8° vs. − 5.3° ± 24.1°, p = 0.009), higher pre-op PI-LL (30.8° ± 24.0° vs.57.0° ± 23.7°, p = 0.002), as well as lower post-op PT (22.9° ± 7.5° vs.15.4° ± 9.8°, p = 0.019) (Table 1).
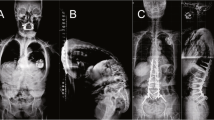
From immediate post-operation to last follow-up, PI in Group A (ΔPI = − 2.3° ± 6.2°) remained stable (t = − 1.483, p = 0.159). In Group B, the PI in 24 patients (48%) returned with an increase in PI of larger than 5° (Group B1) (Fig. 1), while the other 26 (52%) showed no increase (mean ΔPI = − 4.2° ± 10.7°) (Group B2) (Figs. 2 and 3). Subgroup analysis revealed that, in addition to ΔPI, post-op PI, post-op PT and age were significantly different between Group B1 and B2 (all p values < 0.05) (Table 2). Correlation analysis showed that ΔPI (pre-to-post) was significantly correlated with pre-op PI, LL PI-LL (Table 3).
Correlation and regression analysis were performed to determine the influential factors associated with PI returning in Group B (PI decreased higher than 5° at post-op while increased higher than 5° at last follow-up). The correlation analysis showed that pre-op PI (r = − 0.562, p = 0.003), post-op PI (r = − 0.678, p < 0.001), post-op PT (r = − 0.023, p = 0.023), post-op PI-LL (r = − 0.570, p = 0.003) were significantly correlated with ΔPI at last follow-up (Table 4). Furthermore, the logistic regression analysis showed that post-op PI was the associated factor (OR = 0.865, p = 0.024).
Mechanical complications were occurred in 15 patients (36.6%) after surgery, which include PJK in 18 patients, screw loosening in 10 and rod breakage in 2. The incidence of mechanical complications showed no significant between Group A and B (37.5% vs. 36.0%, p = 0.874). Subgroup analysis showed that the incidence in Group B1 and B2 were 33.3% (8/24) and 38.4% (10/26), respectively, and no significant difference was observed (p = 0.857).
Discussion
The current study represents a longitudinal analysis of how PI changes from immediate post-operation to 2-year follow-up in ASD patients who underwent S2AI screw fixation. Based on our findings, PI decreased in 60.9% patients at immediate post-operation, while 48% of them had PI returned at last follow-up which was associated with post-op PI.
As PI has been considered as a fixed anatomical parameter due to limited mobility of sacroiliac (SI) joint, it determines the relative position of the sacral plate in relation to the femoral heads, as well as represented the cornerstone for maintaining spinal balance and postural equilibrium [8]. However, in recent years, a number of studies have questioned the fixed nature of PI. For instance, Skalli et al. [9] were the first to report that 10 out of 21 patients had more than 5° change of PI after posterior spinal fusion. Similarly, Bao et al. [3] found that PI was higher in elder female patients. Likewise, they also shown the increased PI may be associated with sagittal malalignment which led to an increase in L5-S1 bending moment [10]. Moreover, some authors attributed the change in PI at immediate post-operation to the motion of sacroiliac joint [6, 11]. In this study, we also found that PI was significantly decreased (from 49.3° ± 13.7°to 42.6° ± 13.1°) postoperatively, which supported previous findings that PI was not a constant value.
Previously, studies have also reported the changes in PI for ASD patients who have undergone S2AI screw fixation. In this regard, our current study found similarly that PI greatly decreased after S2AI screw fixation in 48% (24/50) of ASD patients with a mean ΔPI of 11.4° ± 4.8° in Group B. Similar to our finding, Ishida et al. [12] found that PI significantly changed from 63.6° ± 12.3° to 57.4° ± 9.6° in S2AI group postoperatively. Likewise, Wei et al. [6] reported that 36.8% had a PI change ≥ 6.0°, and pointed that PI decreased was more commonly in patients with higher pre-op PI and greater PI-LL mismatch. The authors speculated that this observation may be due to longstanding compensatory measures and greater SI joint laxity. Recently, a study demonstrated mobile SI joint is related to the change in PI in aging spine [10]. Our previous study also suggested that PI decreased more when ASD patients who had lumbar kyphosis or had a greater PI preoperatively, which echoed the hypothesis that sagittal spinopelvic malalignment may contribute to the change in PI [5, 13]. Taken together, these findings would imply the importance on considering the role of PI when making surgical plan and evaluating clinical outcomes. However, further investigation on the dynamic change of PI using a longitudinal follow-up cohort would still be warranted.
In the present study, our results revealed that the decreased PI (mean ΔPI: 13.1°) in Group B returned in 24 patients (Group B1, 48%). Whereas for the remaining 26 patients (Group B2; 52%), they showed no increase of PI (mean: ΔPI of − 4.2°). To our knowledge, this is the first study on the observation of the decreased post-op PI in patients after S2AI screw fixation recovering during follow-up. In addition to ΔPI, our study also shown Group B1 had a significantly lower post-op PI and post-op PT than Group B2. Interestingly, these significant differences disappeared spontaneously at follow-up. Based on our correlation analysis, it showed that pre-op PI, post-op PI and post-op PI-LL were significantly correlated with ΔPI at last follow-up, which indicates that sagittal malalignment would play an important role to the recovery of PI. This finding revealed that the patients with a higher pre-op PI may be less likely to recover for those with a decrease of PI at immediate post-op during follow-up. Therefore, more attention should be recognized on avoiding the mechanical complications for these patients with high PI at pre-op [14]. In addition, these results may be explained by the fact that the patients in Group B1 had a relatively lower post-op PI than those in Group B2. Similarly, previous report also showed that spinal malalignment may lead to an increased PI in patients with severe sagittal malalignment [3]. Moreover, our linear regression analysis confirmed that lower post-op PI was the associated factor on contributing to the recovery of PI during follow-up.
In recent years, the dynamic change of PI has become a hot topic [5, 6, 15]. It is well believed that position altering from standing to prone intraoperatively, as well as SI joint motion through S2AI screw placement, could account for the decrease in PI postoperatively 16,17,18]. However, it was found that the change in PI does not stop during follow-up period in nearly half of the patients. The current study implied that the patients with lower PI and PT at immediate post-op may have their PI recovered during follow-up. Although pelvic retroversion may generate reaction force on the SI joint in patients with sagittal malalignment and SI joint motion could play a role in PI change, it is hard to explain whether the recovery of PI in some patients during follow-up may be due to the SI joint being completely fixed [19].
Although our study has provided evidence, there remains several limitations toward our findings. Firstly, due to the strict inclusion criteria, the sample size included in our study was relatively small to possibly bias the statistical result. Secondly, the anatomical change at the SI joint needs to be further confirmed by using the routine standard of computed tomography (CT). However, owing to ethical concern on radiation exposure, this was not provided for all patients in this study. Thirdly, this study is limited by its retrospective nature. Therefore, future longitudinal studies with a long-term follow-up would be required to elucidate the change in PI and its recovery after spinal surgical correction using S2AI screws.
In conclusion, PI decreased in more than half of ASD patients after spinal surgery using S2AI screws, with 48% of them reported the recovery of PI during the 2-year follow-up. Lower pre-op PI, post-op PI and PT were strongly associated with the recovery of PI. Therefore, spine surgeons should be aware of that the patients with a higher PI at pre-op should not be over-corrected to avoid mechanical complications after surgery.
References
Schlösser TPC, Janssen MMA, Hogervorst T et al (2017) The odyssey of sagittal pelvic morphology during human evolution: a perspective on different Hominoidae. Spine J. https://doi.org/10.1016/j.spinee.2017.03.016
Kleck CJ, Noshchenko A, Burger EL, Cain CMJ, Patel VV (2021) Postoperative pelvic incidence (PI) change may impact sagittal spinopelvic alignment (SSA) after instrumented surgical correction of adult spine deformity (ASD). Spine Deform 9(4):1093–1104
Bao H, Liabaud B, Varghese J et al (2018) Lumbosacral stress and age may contribute to increased pelvic incidence: an analysis of 1625 adults. Eur Spine J 27(2):482–488
Place H, Hayes A, Huebner S, Hayden A, Israel H, Brechbuhler J (2017) Pelvic incidence: A fixed value or can you change it? Spine J 17(10):1565–1569
Tseng C, Liu Z, Bao H et al (2019) Long fusion to the pelvis with S2-alar-iliac screws can induce changes in pelvic incidence in adult spinal deformity patients: analysis of predictive factors in a retrospective cohort. Eur Spine J 28:138–145
Wei C, Zuckerman SL, Cerpa M et al (2020) Can pelvic incidence change after spinal deformity correction to the pelvis with S2-alar-iliac screws? Eur Spine J. https://doi.org/10.1007/s00586-020-06658-3
Lafage R, Schwab F, Challier V et al (2016) Defining spino-pelvic alignment thresholds: Should operative goals in adult spinal deformity surgery account for age? Spine (Phila Pa 1976) 41(1):62–68
Le Huec JC, Aunoble S, Philippe L, Nicolas P (2011) Pelvic parameters: origin and significance. Eur Spine J 20(Suppl 5):564–571
Skalli W, Zeller RD, Miladi L et al (2006) Importance of pelvic compensation in posture and motion after posterior spinal fusion using CD instrumentation for idiopathic scoliosis. Spine (Phila Pa 1976) 31(12):E359-366
Bao H, Zhang Y, Shu S et al (2020) Position related change of pelvic incidence depends on the non-fused sacroiliac joint in patients with degenerative spinal diseases. Spine. https://doi.org/10.1097/BRS.0000000000003884
Cecchinato R, Redaelli A, Martini C et al (2017) Long fusions to S1 with or without pelvic fixation can induce relevant acute variations in pelvic incidence: a retrospective cohort study of adult spine deformity surgery. Eur Spine J 26(Suppl 4):436–441
Ishida W, Elder BD, Holmes C et al (2017) Comparison between S2-alar-iliac screw fixation and iliac screw fixation in adult deformity surgery: reoperation rates and spinopelvic parameters. Global Spine J 7(7):672–680
Jean L (2014) Influence of age and sagittal balance of the spine on the value of the pelvic incidence. Eur Spine J 23(7):1394–1399
Yilgor C, Sogunmez N, Boissiere L et al (2017) Global alignment and proportion (GAP) score: development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J Bone Joint Surg Am 99(19):1661–1672
Lee JH, Na KH, Kim JH, Jeong HY, Chang DG (2016) Is pelvic incidence a constant, as everyone knows? Changes of pelvic incidence in surgically corrected adult sagittal deformity. Eur Spine J 25(11):3707–3714
O’Brien JR, Yu WD, Bhatnagar R, Sponseller P, Kebaish KM (2009) An anatomic study of the S2 iliac technique for lumbopelvic screw placement. Spine (Phila Pa 1976) 34(12):E439-442
Kuo CC, Martin A, Telles C et al (2016) Biomechanical demands on posterior fusion instrumentation during lordosis restoration procedures. J Neurosurg Spine 25(3):345–351
Charles YP, Yu B, Steib JP (2016) Sacroiliac joint luxation after pedicle subtraction osteotomy: report of two cases and analysis of failure mechanism. Eur Spine J 25(Suppl 1):63–74
Oba H, Ebata S, Takahashi J et al (2019) Loss of pelvic incidence correction after long fusion using iliac screws for adult spinal deformity: cause and effect on clinical outcome. Spine (Phila Pa 1976) 44(3):195–202
Funding
This work was supported by the National Natural Science Foundation of China (NSFC) (No. 82072518), the Nanjing Medical Science and Technique Development Foundation (No. QRX17126) funds, the Jiangsu Provincial Key Medical Center, and the China Postdoctoral Science Foundation (2021M701677).
Author information
Authors and Affiliations
Contributions
Zongshan Hu and Chang-Chun Tseng contributed equally to this work.
Corresponding author
Ethics declarations
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hu, Z., Tseng, CC., Li, J. et al. Dynamic change of pelvic incidence after long fusion to pelvis with S2-alar-iliac screw: a 2-year follow-up study. Eur Spine J 31, 3566–3572 (2022). https://doi.org/10.1007/s00586-022-07391-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07391-9