Abstract
Study design
A cross-sectional study.
Objective
To investigate the correlation of cervical spine alignment changes with aging in asymptomatic population.
Background
Previous studies demonstrated the influence of lumbar and thoracic spine on cervical spine alignment, but few has reported the cervical spine alignment change along with aging in asymptomatic population.
Methods
Asymptomatic population were divided into four groups according to different ages (Group A: ≤20 years; Group B: 21–40 years; Group C: 41–60 years; Group D: ≥61 years). Each group was composed of 30 subjects. The following parameters were measured: C0–1 Cobb angle, C1–2 Cobb angle, C2–7 Cobb angle, C1–7 sagittal vertical axis (C1–7 SVA), C2–7 SVA, central of gravity to C7 sagittal vertical axis (CG–C7 SVA), Thoracic Inlet Angle (TIA), Neck Tilt (NT), cervical tilt, cranial tilt, T1 slope (TS), TS-CL, and ANOVA statistical method was used to analyze the differences among four groups, and then, linear regression analysis was performed to analyze correlation of the cervical spine alignment with the aging.
Results
C1–7 SVA, C2–7 SVA, CG–C7 SVA, TIA, NT, TS, and cranial tilt were found statistically different among four groups (P < 0.01). From Group A to Group D, the mean C1–7 SVA were 30.7, 26.0, 21.8, and 36.9 mm, the mean C2–7 SVA were 18.7, 14.7, 11.9, and 24.7 mm, and the mean CG–C7 SVA were 19.6, 16.6, 9.4, and 26.7 mm. The mean TIA were 62.4°, 65.0°, 71.8°, and 76.9°, the mean NT were 39.4°, 43.8°, 46.3°, and 48.2°, the mean TS were 23.0°, 21.1°, 25.5°, and 28.7°, and the mean cranial tilt were 5.7°, 4.8°, 3.0°, and 9.5°. Further linear regression indicated that TIA (r = 0.472; P < 0.0001), NT (r = 0.337; P = 0.0006), and TS (r = 0.299; P = 0.0025) were positively correlated with aging.
Conclusion
A gradual increase of TIA, NT, and TS, accompanied with an increased CL, is found along with aging in asymptomatic population, among which TIA, NT, and TS are significantly correlated with physiological nature of aging.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The cervical spine not only supports the mass of the head, but also possesses the characteristics of the widest range of motion related to the rest of the spine. The complexity of the cervical segments makes it susceptible to deformity which accompanied with alignment pathology. Cervical deformity is one of the most common neurological disorders that are being increasingly observed in the degenerative cervical dysfunction. Abnormalities of the cervical alignment can compromise the health-related quality of life (HRQOL) of the patient and impose adverse effects on the overall functioning of the subjects [1]. On the contrary, improvements in regional cervical alignment postoperatively correlated positively with improved HRQOL [2, 3].
In the past, publications defined normative values for regional and global thoracolumbar and spinopelvic parameters [4], and evaluated the influence of segmental, regional, and global balance on cervical alignment [5,6,7]. However, few literatures investigate how the cervical spine alignment changes along with aging in asymptomatic population. Therefore, understanding the aging-related cervical spine alignment changes is favorable for proper treatment consideration. In this study, we grouped asymptomatic volunteers according to different ages from the youth to the old to investigate the correlation of cervical spine alignment changes with aging.
Materials and methods
Asymptomatic subject enrollment
This study was approved by the Institutional Review Board of Nanchang University. Written informed consents were obtained from eligible volunteers. From January 2015 and December 2015, a total of 184 were enrolled in the study. Efforts were made to recruit an even distribution of volunteers because of trying to establish normative values based on age. Volunteers met the following criteria were excluded. Exclusion criteria were: (1) a history of prior spine operation; (2) coronal spine deformities (Cobb angle >10°); (3) frequent complaints of neck pain; (4) radiculopathy or myelopathy due to cervical spondylopathy; (5) congenital pathologic condition of the cervical spine; (6) history of neuromuscular, inflammatory disorders of cervical spine; (7) pregnancy; and (8) osteoporosis. Forty-four volunteers who were meet the exclusion criteria before radiography were excluded, 23 volunteers were withdrawn from the study due to fail to keep an appointment, and seven meet the exclusion criteria after radiography. Finally, a hundred twenty asymptomatic (47 male and 53 female) subjects aged 8–81 were finally included in the study. The subjects were divided into four groups according to different ages (Group A: ≤20 years; Group B: 21–40 years; Group C: 41–60 years; and Group D: ≥61 years). Each group was composed of 30 subjects. Volunteer BMI was recorded after included. The neck disability index (NDI) was accessed to reassure all volunteers to be asymptomatic.
Radiographic parameters
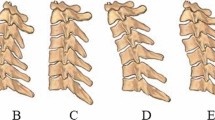
When taken X-ray, the subjects were informed of looking ahead and relaxing in a neutral posture. Standing anteroposterior and lateral radiographs of cervical spine were obtained. The following parameters were measured: C0–1 Cobb angle, C1–2 Cobb angle, C2–7 Cobb angle, C1–7 sagittal vertical axis (C1–7 SVA), C2–7 SVA, central of gravity to C7 sagittal vertical axis (CG–C7 SVA), Thoracic Inlet Angle (TIA), Neck Tilt (NT), cervical tilt, cranial tilt, T1 slope (TS), and TS-CL. All parameters were measured by two researchers at the same time, one was orthopedic surgeon and one was radiologist. Only the value of parameters agreed by both researchers was recorded. When disagreement between two researchers occurred, the value of parameter was discussed and decided in routine roundtable meeting, in which the whole research team members attended. The parameters were defined as follows: (1) C0–1 Cobb angle was an angle between McGregor’s line and the line linking the inferior of anterior arch and the inferior of posterior arch of atlas; (2) C1–2 Cobb angle was defined as an angle between the line linking the inferior of anterior arch and the inferior of posterior arch of atlas and the lower endplate of C2; (3) C2–7 Cobb angle, an angle between C2 lower end plate and C7 lower end plate; (4) C1–7 SVA, distance between a plumb line dropped from the anterior tubercle of C1 and posterior superior corner of C7; (5) C2–7 SVA, distance between a plumb line dropped from the centroid of C2 and posterior superior corner of C7; (6) CG–C7 SVA, distance between a plumb line dropped from anterior margin of external auditory canal and posterior superior corner of C7; (7) TIA, the angle between a line originating from the center of the T1 upper end plate and perpendicular to the T1 upper end plate and a line from the center of the T1 upper end plate and the upper end of the sternum; (8) NT, an angle between two lines both originating from the upper end of the sternum, with one being a vertical line and the other connecting to the center of the T1 upper end plate; (9) cervical tilt was defined as the angle between two lines, both originating from the center of the T1 upper end plate; one is vertical to the T1 upper end plate and the other passes through the tip of the dens; (10) cranial tilt was defined as the angle between two lines, both originating from the center of the T1 upper end plate, with one passing through the dens and the other being a vertical line; and (11) TS was defined as an angle between a horizontal plane and a line parallel to the T1 upper end plate. Examples of above parameters are shown in Figs. 1, 2, and 3.
Graphical definition of C0–1 Cobb angle, C1–2 Cobb angle, and C2–7 Cobb angle. C0–1 Cobb angle was an angle between McGregor’s line (line A) and the line linking the inferior of anterior arch and the inferior of posterior arch of atlas (line B); C1–2 Cobb angle was defined as an angle between the line linking the inferior of anterior arch and the inferior of posterior arch of atlas (line B) and the lower endplate of C2 (line C); C2–7 Cobb angle, an angle between C2 lower end plate (line C); and C7 lower end plate (line D)
Graphical definition of C1–7 sagittal vertical axis (C1–7 SVA), C2–7 SVA, central of gravity to C7 sagittal vertical axis (CG–C7 SVA). C1–7 SVA was defined as the distance between a plumb line dropped from the anterior tubercle of C1 and posterior superior corner of C7 (showed with green line); C2–7 SVA, distance between a plumb line dropped from the centroid of C2 and posterior superior corner of C7 (showed with yellow line); and CG–C7 SVA, distance between a plumb line dropped from anterior margin of external auditory canal and posterior superior corner of C7 (showed with red line)
Graphical definition of Thoracic Inlet Angle (TIA), Neck Tilt (NT), T1 slope (TS), cervical tilt, and cranial tilt. TIA was defined as the angle between a line originating from the center of the T1 upper end plate and perpendicular to the T1 upper end plate and a line from the center of the T1 upper end plate and the upper end of the sternum; NT, an angle between two lines both originating from the upper end of the sternum, with one being a vertical line and the other connecting to the center of the T1 upper end plate; Cervical tilt was defined as the angle between two lines, both originating from the center of the T1 upper end plate; one is vertical to the T1 upper end plate and the other passes through the tip of the dens; Cranial tilt was defined as the angle between two lines, both originating from the center of the T1 upper end plate, with one passing through the dens; and the other being a vertical line; TS was defined as an angle between a horizontal plane and a line parallel to the T1 upper end plate
Statistical analysis
Data were analyzed using the SPSS statistical software (version 17.0; SPSS, Inc., Chicago, IL, USA). All values are expressed as mean ± standard deviation (SD). ANOVA statistical method was used to analyze the differences among four groups, and then, linear regression analysis was performed to analyze correlation of the cervical spine alignment with the aging. A P value of <0.05 was considered statistically significant.
Results
Demographics
All 120 volunteers were recruited and imaged. The average age was 40.6 years (range 8–81). The average BMI was 23.8 ± 6.6. The average NDI score was 2.8 ± 2.4 which reflected the asymptomatic nature of this cohort. The demographic data of volunteers are shown in Table 1.
Parameters analysis
From group A to group D, the mean C1–7 SVA were 30.7 ± 11.0, 26.0 ± 10.4, 21.8 ± 12.9, and 36.9 ± 11.2 mm, the mean C2–7 SVA were 18.7 ± 8.9, 14.7 ± 8.6, 11.9 ± 11.2, and 24.7 ± 8.8 mm, and the mean CG–C7 SVA were 19.6 ± 13.5, 16.6 ± 13.6, 9.4 ± 16.7, and 26.7 ± 10.8 mm. The mean TIA were 62.4 ± 8.5°, 65.0 ± 11.9°, 71.8 ± 10.3°, and 76.9 ± 8.6°, the mean NT were 39.4 ± 8.4°, 43.8 ± 8.0°, 46.3 ± 9.4°, and 48.2 ± 6.7°, the mean TS were 23.0 ± 7.1°, 21.1 ± 7.8°, 25.5 ± 7.6°, and 28.7 ± 9.0°, and the mean cranial tilt were 5.7 ± 6.2°, 4.8 ± 5.7°, 3.0 ± 6.7°, and 9.5 ± 8.4°. Above significant difference parameters with mean values are shown in Table 2. In addition, the change tendency of above parameters is shown in Figs. 4 and 5.
Mean values of C2–7 Cobb angle, C1–7 SVA, C2–7 SVA, and CG–C7 SVA. All these parameters had the most significant difference between group C and group D (P < 0.001), which implied an obvious anterior translation of cervical spine occurring in old population. Correspondingly, the decreasing tendency of C2–7 Cobb angle from group C to group D was marked, which implied a obvious increasing of cervical lordosis occurring to compensate for anterior translation of cervical spine in old population
Through analyzing the significant change in cervical alignment (shown in Table 3), we found that C1–7 SVA had significant difference between group A and group C (P = 0.008), group B and group D (P = 0.001), and group C and group D (P < 0.001), C2–7 SVA had significant difference between group A and group C (P = 0.014), group A and group D (P = 0.028), group B and group D (P < 0.001), and group C and group D (P < 0.001), CG–C7 SVA had significant difference between group A and group C (P = 0.011), group B and group D (P = 0.012), and group C and group D (P < 0.001), and Cranial tilt (P = 0.0011) had significant difference between group B and group D (P = 0.017) and group C and group D (P = 0.001). C1–7 SVA, C2–7 SVA, and CG–C7 SVA had the most significant difference between group C and group D (P < 0.001). Correspondingly, although C2–7 Cobb angle had not significant difference between group C and group D (P = 0.105), the tendency of decreasing was marked. Between group A (the youngest) and group D (the oldest), the most significant difference was found in the change of TIA (P < 0.0001) and NT (P < 0.0002). TS was found to be significantly different between group A and group D (P < 0.0107), group B and group C (P = 0.0465), and group B and group D (P = 0.0007).
Further linear regression disclosed that TIA (r = 0.472; P < 0.0001), NT (r = 0.337; P = 0.0006), and TS (r = 0.299; P = 0.0025) were positively correlated with aging (shown in Fig. 6).
Discussion
In this study, we grouped asymptomatic subjects according to age, measured sagittal alignments of cervical spine and found that TIA, NT, and TS significantly increase along with aging.
As the pivotal element of cervicothoracic junction, the thoracic inlet is a fixed bony circle that is composed of the T-1 vertebral body, the first ribs on both sides, and the upper part of the sternum. The TIA was defined as the angle subtended between a line originating from the center of the T-1 upper endplate and perpendicular to the T-1 upper endplate and a line from the center of the T-1 upper endplate and the upper end of the manubrium [6]. Therefore, TIA and TS were primarily determined by T1 declination in the sagittal plane. If the relative position of T1 to manubrium unchanged, a lager T1 declination results in a larger TIA and TS which yields a greater magnitude of cervical lordosis just as a greater pelvic incidence leads to greater lumbar lordosis. In this cohort, TIA and TS significantly increase from the youth group to the old group accompanied with an increased cervical lordosis which is required to balance the head over the thoracic inlet. Similar results were also reported in the study form Amabile [8] who measured global spine alignment parameters of 41 volunteers (49–76 years) and found that the cervical lordosis increased in these volunteers, compared with younger group(less than 40 years). Besides aging, gender was found to be another factor influencing the change in C3–C7 lordosis [9].
An increased T1 declination throughout the life span may result from increasing of thoracic kyphosis. Yokoyama [10] found that TIA, TK, and C2–C7 lordosis were found to markedly increase with age from late middle age and considered that increases in cervicothoracic curvature occurring along with thoracic deformation underlie age-related changes in the spine. Ailon [11] reported that thoracic kyphosis tends to increase with age. The cause is multifactorial and involves an interaction between degenerative changes, vertebral compression fractures, muscular weakness, and altered biomechanics. More early, Goh [12] elaborated that an age-related decline was noted in the ratio of anterior height to posterior height of thoracic vertebra, corresponding to an increase in the degree of vertebral wedge configuration which leads to thoracic hyperkyphosis during the later years of life. Thoracic hyperkyphosis influences the configuration of thoracic inlet and increases the age-related T1 declination in the sagittal plane.
Not only TIA but NT also was determined by the relative position of T1 to manubrium in sagittal plane including the vertical distance from T1 to the level of the end of manubrium, as well the horizontal distance from T1 to the perpendicular line drawn from the end of manubrium. First, T1 vertebra is normally located above the level of the end of manubrium. If the T1 declination unchanged, in other words, TS unchanged, a descended position of T1 related to the level of manubrium, which means a decrease of vertical distance from T1 to the level of the end of manubrium, results in a larger TIA, accompanied with a greater NT in this circumstance. Research [13] showed that the vertical decrease in vertebral dimension was age-associated throughout the life span which gives rise to the decrease of the height of thoracic spine. Definitely, disc degeneration and space narrowing [13, 14] also contribute to the height loss in thoracic spine. As a consequence, a descended position of T1 related to the level of manubrium is inevitable, which leads to a larger TIA and NT. Brandner [15] suggested that the accelerated rate of vertical growth and a corresponding slowing of the increase in the anteroposterior vertebral dimension during the adolescent growth spurt results in a rapid increase in the vertebral height. Contrarily, Goh [12] noted that there was a pattern of gradual decline in the ratio of posterior height of vertebra to the anteroposterior vertebral dimension throughout the adult life span. This decline may well be associated with the natural cessation of skeletal growth prior to adulthood and the eventual gradual loss in height stature during the later years of life. Thus, a decrease of vertical distance from T1 to the level of the end of manubrium will result in a larger TIA and NT. Second, an increase of horizontal distance from T1 to the perpendicular line drawn from the end of manubrium, according to the definition of TIA, can also result in a larger TIA and NT if the T1 declination unchanged. Bastir [16] indicated that from infant to adults, there is not only an increase in mediolateral dimensions, but also a marked increase in anteroposterior dimensions of the upper thorax, relative to the lower thorax. This transforms the pyramidal infant thorax into the barrel-shaped one of adults. In the following study [17], they further demonstrated that the increase of rib torsion and axial rib curvature is ontogenetic factors that contribute to the adult thorax configuration. When the anteroposterior dimensions of the upper thorax increased, the horizontal distance from T1 to the perpendicular line drawn from the end of manubrium would elongate, which results in a larger TIA and NT. Therefore, the decline of the vertical distance of T1 to manubrium and the elongation of the horizontal distance of T1 to manubrium in sagittal plane may explain the results that TIA and NT gradually increased along with aging in our study.
There are limitations in our study. First, the thoracic, lumbar, and spinopelvic segment alignments are not measured. Associating the cervical alignments with global alignments may illuminate the changes of cervical alignments more comprehensively. Taking global spine X-ray to correlate the findings of this study with changes in global alignment parameters will conducted in future study. Second, so far, there is still a lack of consensus as to the optimal method to accurately assess the cervical sagittal alignment. Donk [18] reported that an absolute measurement of the angle between C-2 and C-7 does not unequivocally define the sagittal cervical alignment and recommended the modified Toyama method as a better tool for a global assessment of cervical sagittal alignment. However, Toyama method cannot quantify the curve of lordosis. Therefore, in this cohort, we still used C2–7 lordosis as one of the alignment parameters. Third, we obtained our measures from an Asian population, which is hard to generalize our results to other populations. Data from multi-ethnic population need collected in further study. However, this is the first preliminary analysis of the change of cervical spine alignment along with aging in asymptomatic population, based on which surgeons can properly evaluate cervical alignment of patient in different lifetimes with cervical disorders, and probably map out more precise cervical realignment parameters referred to correction surgery in patient with cervical deformity.
Conclusion
A gradual increase of TIA, NT, and TS, accompanied with an increased CL, is found along with aging in asymptomatic population, among which TIA, NT, and TS are significantly correlated with physiological nature of aging.
References
Lee JS, Youn MS, Shin JK, Goh TS, Kang SS (2015) Relationship between cervical sagittal alignment and quality of life in ankylosing spondylitis. Eur Spine J 24(6):1199–1203
Protopsaltis TS, Scheer JK, Terran JS, Smith JS, Hamilton DK, Kim HJ, Mundis GM Jr, Hart RA, McCarthy IM, Klineberg E, Lafage V, Bess S, Schwab F, Shaffrey CI, Ames CP, International Spine Study Group (2015) How the neck affects the back: changes in regional cervical sagittal alignment correlate to HRQOL improvement in adult thoracolumbar deformity patients at 2-year follow-up. J Neurosurg Spine 23(2):153–158
Youn MS, Shin JK, Goh TS, Kang SS, Jeon WK, Lee JS (2016) Relationship between cervical sagittal alignment and health-related quality of life in adolescent idiopathic scoliosis. Eur Spine J 25(10):3114–3119
Diebo BG, Varghese JJ, Lafage R, Schwab FJ, Lafage V (2015) Sagittal alignment of the spine: what do you need to know? Clin Neurol Neurosurg 139:295–301
Smith JS, Lafage V, Schwab FJ, Shaffrey CI, Protopsaltis T, Klineberg E, Gupta M, Scheer JK, Fu KM, Mundis G, Hostin R, Deviren V, Hart R, Burton DC, Bess S, Ames CP, International Spine Study Group (2014) Prevalence and type of cervical deformity among 470 adults with thoracolumbar deformity. Spine (Phila Pa 1976) 39(17):E1001–E1009
Lee SH, Kim KT, Seo EM, Suk KS, Kwack YH, Son ES (2012) The influence of thoracic inlet alignment on the craniocervical sagittal balance in asymptomatic adults. J Spinal Disord Tech 25(2):E41–E47
Lee SH, Son ES, Seo EM, Suk KS, Kim KT (2015) Factors determining cervical spine sagittal balance in asymptomatic adults: correlation with spinopelvic balance and thoracic inlet alignment. Spine J 15(4):705–712
Amabile C, Le Huec JC, Skalli W (2016) Invariance of head-pelvis alignment and compensatory mechanisms for asymptomatic adults older than 49 years. Eur Spine J. doi:10.1007/s00586-016-4830-8
Yukawa Y, Kato F, Suda K, Yamagata M, Ueta T, Yoshida M (2016) Normative data for parameters of sagittal spinal alignment in healthy subjects: an analysis of gender specific differences and changes with aging in 626 asymptomatic individuals. Eur Spine J. doi:10.1007/s00586-016-4807-7
Yokoyama K, Kawanishi M, Yamada M, Tanaka H, Ito Y, Kawabata S, Kuroiwa T (2017) Age-related variations in global spinal alignment and sagittal balance in asymptomatic Japanese adults. Neurol Res 39(5):414–418. doi:10.1080/01616412.2017.1296654
Ailon T, Shaffrey C, Lenke LG, Harrop JS, Smith JS (2015) Progressive spinal kyphosis in the aging population. Neurosurgery 77(Suppl 4):S164–S172. doi:10.1227/NEU.0000000000000944
Goh S, Tan C, Price RI, Edmondston SJ, Song S, Davis S, Singer KP (2000) Influence of age and gender on thoracic vertebral body shape and disc degeneration: an MR investigation of 169 cases. J Anat 197(Pt 4):647–657
Matsumoto M, Okada E, Ichihara D, Watanabe K, Chiba K, Toyama Y, Fujiwara H, Momoshima S, Nishiwaki Y, Hashimoto T, Takahata T (2010) Age-related changes of thoracic and cervical intervertebral discs in asymptomatic subjects. Spine 35(14):1359–1364
Weiler C, Schietzsch M, Kirchner T, Nerlich AG, Boos N, Wuertz K (2012) Age-related changes in human cervical, thoracal and lumbar intervertebral disc exhibit a strong intra-individual correlation. Eur Spine J. 21(Suppl 6):S810–S818
Brandner ME (1970) Normal values of the vertebral body and intervertebral disk index during growth. Am J Roentgenol Radium Ther Nucl Med 110(3):618–627
Bastir M, García Martínez D, Recheis W, Barash A, Coquerelle M, Rios L, Peña-Melián A, García Río F, O’Higgins P (2013) Differential growth and development of the upper and lower human thorax. PLoS One 8(9):e75128
García-Martínez D, Recheis W, Bastir M (2016) Ontogeny of 3D rib curvature and its importance for the understanding of human thorax development. Am J Phys Anthropol 159(3):423–431
Donk RD, Fehlings MG, Verhagen WI, Arnts H, Groenewoud H, Verbeek AL, Bartels RH (2017) An assessment of the most reliable method to estimate the sagittal alignment of the cervical spine: analysis of a prospective cohort of 138 cases. J Neurosurg Spine 26(5):572–576. doi:10.3171/2016.10.SPINE16632
Acknowledgements
Funding was provided by 5511 innovation-driven program of Jiangxi Province Department of Science and Technology (Grant No. 20165BCB18017), National Natural Science Foundation of China (CN) (Grant No. 81460405), Key Program of Jaingxi Provincial Department of Science and Technology (Grant No. 20152ACB21024), and Research Program of Health and Family Planning Commission of Jiangxi Province (Grant Nos. 20155087, 20155110).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare that we do not have any commercial or associative interest that represents a conflict of interest in connection with the work submitted.
Rights and permissions
About this article
Cite this article
Chen, Y., Luo, J., Pan, Z. et al. The change of cervical spine alignment along with aging in asymptomatic population: a preliminary analysis. Eur Spine J 26, 2363–2371 (2017). https://doi.org/10.1007/s00586-017-5209-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5209-1