Abstract
Purpose
The study of the interrelation between hip and spine disorders is gaining increasing importance in the last years, but the link between Hip Osteoarthritis (HOA) and Low Back Pain (LBP) remains still unclear. Aim of the study is to assess the relationship between Femoral Neck Anteversion (FNA), LBP, and spinopelvic parameters in patients undergoing Total Hip Replacement (THR) for unilateral severe primary HOA.
Materials and methods
91 patients were recruited. Inclusion criteria were: grade 5 or 6 unilateral HOA, according to Turmezei, and Harris Hip score (HHS) <60. Exclusion criteria were: secondary hip osteoarthritis (dysplasia of the hip, rheumatoid arthritis, and ankylosing spondylitis); previous surgery of the spine, hip or knee; scoliosis with a Cobb angle greater than 10°; spondylolisthesis; history of spine fractures; previous bone tuberculosis or any spine infections; any contraindications to CT; BMI >30. Patients were divided into two homogeneous Groups according to the presence (Group-A) or not of concomitant LBP (Group-B). All patients underwent preoperatively a hip CT scan to evaluate FNA, Acetabular Anteversion (AA), and Combined Anteversion (CA = FNA + AA). ΔFNA, ΔAA and ΔCA were calculated as the differences between the arthritic hip and the normal hip angles in each Group. Full spinal X-rays in upstanding position were performed before (baseline) and 6 months after THR (follow-up) to calculate spinopelvic parameters. The health-related quality of life (HRQoL) was evaluated at baseline and at follow-up using Visual Analogue Scale (VAS), HHS, Oswestry Disability Index (ODI), Roland–Morris Disability Questionnaire (RM), and Short-Form Health Survey (SF-36). The intra-group and inter-group variability were assessed using, respectively, paired and unpaired t tests. At baseline, the association between HRQoL scores and ΔFNA, ΔAA, and ΔCA was analysed by the Pearson correlation test.
Results
At baseline, in Group-A, there was a significant difference between arthritic FNA and normal hip FNA, while no differences were found in AA between the two hips. A close correlation was observed between ΔFNA and Spine-VAS (r = 0.788), ODI (r = 0.824), and RM (r = 0.775). In Group-B, there was not a significant difference in FNA and AA between the two hips. At recruitment, in Group-A patients, we recorded a higher LL, SS, PI, SVA(C7), and a lower PT and T1-SPI compared with Group-B subjects. Six months after THR, in Group-A, an improvement of all clinical scores was recorded, as well as, a significant reduction of SS, LL, T1PA, and SVA(C7) and an increment of PT. In Group-B, at follow-up, an improvement of HHS, Hip-VAS, and SF-36 was recorded, while the changes in spinopelvic parameters were not significant.
Conclusions
Patients with concomitant unilateral HOA and LBP showed a marked anteverted FNA in the arthritic hip and a spinopelvic misalignment. After THR, a relief of both hip and low back pain and a change in spinopelvic parameters is observed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Symptomatic Hip Osteoarthritis (HOA) and Low Back Pain (LBP) are two emerging diseases, whose prevalence is increasing in the last decades, due to the aging of the population and the obesity epidemic [1]. It is estimated that the mean prevalence of HOA is 10.1% in Europe and 7.2% North America [1], while LBP has a point prevalence of 12–33% in general population [2]. Unfortunately, a subset of patients suffers for concomitant HOA and LBP [3]; it is reported that the prevalence of LBP among patients undergoing primary total hip replacement (THR) surgery varies between 21.2 and 60.4% [4].
The coexistence of lumbar spine and hip disorders depicts the Hip-Spine Syndrome (HSS), originally described by Offierski and MacNab in 1983 [5], who identified four subcategories labelled as simple, secondary, complex, and misdiagnosed HSS. “Secondary” HSS was described in patients with symptoms derived from changes in the lumbar spine, which were secondary to pathological changes in the hip [5]. Offierski and MacNab postulated that the fixed hip flexion deformity causes a progressive anteversion of the pelvis and a compensatory lumbar hyperlordosis; the subsequent subluxation of the lumbar posterior facets triggers LBP [5]. This hypothesis, however, has never been validated, to best of our knowledge.
Despite several clinical–radiological studies [3, 4, 6–8] have reported a significant improvement of LBP after THR, the pathogenesis of HSS has not been explained yet.
Increased femoral neck anteversion (FNA) have been implicated in the pathogenesis of HOA [9, 10], but none of the previous study has evaluated the native FNA angle in patients with HSS undergoing THR.
This prospective interventional study aims to assess the relationship between FNA, LBP, and spinopelvic parameters in patients with severe primary unilateral HOA undergoing THR.
Materials and methods
From January 2015 to May 2016, 214 patients (116 females, 98 males) underwent primary THR in our institute. According to inclusion and exclusion criteria, 91 patients (57 females, 34 males, mean age 65.8 years, and range 56–78 years) were recruited for the current study; all patients gave informed consent before enrolment. Inclusion criteria were: grade 6 or 7 unilateral HOA according to Turmezei [11] and Harris Hip score (HHS) <60. Exclusion criteria were: secondary hip osteoarthritis (dysplasia of the hip, rheumatoid arthritis, and ankylosing spondylitis); previous surgery of the spine, hip, or knee; scoliosis with a Cobb angle greater than ten degrees; spondylolisthesis; history of spine fractures; previous bone tuberculosis or any spine infections; any contraindications to CT; BMI >30.
LBP was defined as consecutive pain for more than 6 months and an Oswestry Disability Index (ODI) >41% at recruitment. The patients were divided into two Groups, depending on the presence/absence of LBP: patients suffering for LBP were included in Group-A, whereas patients without LBP in Group-B.
Each patient underwent clinical and radiological evaluations before (baseline) and 6 months after THR (follow-up); all data were gathered and analysed in blind manner. All THRs were performed by the same surgical team, using a lateral Hardinge approach and a modular cementless hip prosthesis. After surgery, all patients followed the same rehabilitation protocol.
Radiological evaluation included the routine imaging protocol used for patients undergoing THR at our institute. All radiographs and CT scans were performed by the same Group of radiological technicians.
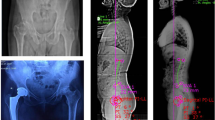
Hip CT scans were obtained using a 2 mm CT cuts (Philips CT Vision MX8000Q machine, Philips Healthcare, The Netherlands, Best) at recruitment only. A radiologist and an orthopaedist, with more than 10 years of experience, evaluated hip CT scans using the DICOM software Weasis (Atlassian). The HOA severity was staged according to CT grading system by Turmezei et al. [11]. The FNA angle (Fig. 1a) was measured using the method of Hernandez et al. [12], while the AA angle was estimated applying the method by Reikeras et al. [13]. The combined anteversion angle (CA) was defined as the sum of FNA and AA.
Femoral Neck Anteversion (FNA). FNA angle (a) is the angle subtended by the line connecting the centres of the femoral head and neck (head–neck axis) and the line connecting the centres of the femoral condyles (transcondylar axis). Hernandez et al. method for FNA angle measurement (b–d). Two axial CT scans were analysed. In the proximal slice, containing the femoral head, femoral neck, and the greater trochanter, the head–neck axis was calculated (b). In the distal image, conducted through the femoral condyles just below the upper pole of the patella, the transcondylar axis was obtained (c). FNA was finally defined as the angle subtended by the head–neck axis and the transcondylar axis (d)
Full spine standing anteroposterior and lateral X-rays were obtained at recruitment and at 6-month follow-up. The radiographs, made during inhalation, were performed to keep the natural standing position of the spine [14]; a good femoral heads resolution was achieved, as well. For the anteroposterior view, the patient was asked to stand in a natural erect posture, knees held in extension, stomach against the cassette, and arms hanging. For the lateral view, the patient was naturally standing up, looking horizontally, hands resting on a vertical support, upper limbs relaxed, and elbows half bent. Two orthopaedists, unknowing the CT results, verified the absence of spinal coronal plane deformities before and after surgery in anteroposterior full spine view and assessed the spinopelvic parameters on lateral standing full spine X-rays using Surgimap (Nemaris Inc., Ver. 2.2.9.9.1, NY, USA). The spinopelvic parameters measured included: pelvic incidence (PI); pelvic tilt (PT); sacral slope (SS); lumbar lordosis (LL); thoracic kyphosis (TK); T1-spinopelvic inclination (T1Spi); T1 pelvic angle (TPA); and sagittal vertical axis [SVA(C7)] (Fig. 2).
Acetabular Anteversion (AA). AA angle measures the fixed orientation of the acetabulum within the horizontal plane, relative to the pelvis. The AA angle is estimated using the method by Reikeras et al., as the angle between a line conducted through the anterior and posterior edges of the acetabulum and a reference line, drawn perpendicular to a line between the posterior pelvic margins
The health-related quality of life (HRQoL) was evaluated by an orthopaedist, who was unaware of radiographic and CT measurement, at baseline and at 6-month follow-up using Visual Analogue Scale (VAS) for spine, VAS for hip, HHS, ODI, Roland–Morris Disability Questionnaire (RM), and Short-Form Health Survey (SF-36).
Statistical analysis
Statistical analysis was performed using the SPSS® 11.0 software (SPSS Inc., Chicago, IL, USA). The FNA, AA, and CA angle of the two hips were compared within each group at baseline using the unpaired t test after ANOVA (analysis of variance). The arthritic hip FNA, AA, and CA between the two groups were compared at baseline using the unpaired t test after ANOVA.
Pearson correlation test was used to evaluate the association between HRQoL scores and ΔFNA, ΔAA, and ΔCA at baseline in both groups.
The paired t test was used to compare changes within each group at 6-month follow-up versus baseline. The tests were two-tailed with a confidence level of 5%.
Results
The main study data are summarized in Table 1. Forty-seven patients (29 females, 18 males, mean age 64.7 years, and range 56–77 years) suffered for concomitant LBP at baseline (Group-A), whereas 44 patients (28 females, 16 males, mean age 67.2 years, and range 60–78) complained only unilateral HOA (Group-B).
Table 2 reports FNA, AA, and CA p values for differences between the two hips within groups (unpaired t test). A significant difference (p = 0.005) between arthritic hip FNA angle and normal hip FNA angle was recorded at baseline in Group-A, while no differences were found in AA angles between the two hips (Table 2). In Group-B patients, there was not a significant difference in FNA, AA, and CA angles between the two hips (Table 2). Furthermore, no significant differences in arthritic hips FNA, AA, and CA between the two groups were observed at recruitment (Table 3).
ΔFNA, ΔAA, and ΔCA were calculated as the differences between the arthritic hip and the normal hip angles (ΔFNA = arthritic hip FNA − normal hip FNA; ΔAA = arthritic hip AA − normal hip AA; ΔCA = arthritic hip CA − normal hip CA). A close correlation was observed at baseline between ΔFNA and Spine-VAS (r = 0.788), ODI (r = 0.824) and RM (r = 0.775) (Table 4).
Table 5 shows spinopelvic parameters’ p values for differences between groups at baseline unpaired t test). In Group-A patients, we observed a higher LL, SS, PI, SVA(C7), and a lower PT and T1-SPI compared with Group-B subjects.
Table 6 reports p values for differences between clinical scores and spinopelvic parameters, at 6-month follow-up versus baseline within each group (paired t test). A significant improvement of all clinical scores was recorded at 6-month follow-up in Group-A (Fig. 3a); a significant improvement of HHS, Hip-VAS, and SF-36 was observed at 6-month follow-up in Group-B. Six months after THR, in Group-A, significant spinopelvic alignment changes were recorded: a reduction of SS (mean change = −6.47, p = 0.0001), LL (mean change = 13, p = 0.007), T1 pelvic angle (mean change = −4.33, p = 0.028) and sagittal vertical axis (mean change = 24.75; p = 0.0086) as well as a significant increment of PT (mean change = 5.62, p = 0.0001). At 6-month follow-up, in Group-B too, we observed some changes in spinopelvic parameters, but they were not statistically significant.
Discussion
The study of the interdependence between spine and the pelvis is gaining an increasing importance in the last years [3–9, 15–24].
In the field of total hip arthroplasty, several clinical studies [3–8, 22, 23] have investigated the relationship between HOA and LBP, documenting that patients with HHS may experience, after THR, in addition to resolution of their hip pain, a significant improvement of LBP [7, 8, 22]. Contrasting findings, however, have been reported on spinopelvic alignment in patients with concomitant HOA and LBP, and the mechanism for HSS remains still unclear (Figs. 4, 5).
Yashimoto et al., in a retrospective radiographic study, reported that patients with HOA had significantly higher PI, SS, and LL compared with those suffering from LBP, suggesting that a higher PI may contribute to the development of HOA because of the anterior uncovering of the acetabulum [26]. These authors, however, recruited both patients with primary HOA and acetabular dysplasia (Crowe type I) and considered, between patients with LBP, patients with degenerative lumbar spine disorders, so their results may be affected by a bias, as already noticed by Weng et al. [6].
Weng et al, in a prospective study, reported in patients with HOA compared with normal controls a significant larger SS and T1-SPI, comparable LL and PI, and smaller PT and C7T [6]. In a more recent study, Weng et al. reported, at 1 year after THR, a relief of LBP in patients suffering for HSS, but surprisingly, they found no significant changes in LL, PT, and SS [27]. These authors, however, have not indicated the HOA radiological stage neither have reported the range of movement of the arthritic hip at recruitment and after THR.
Ben-Galim et al, in a prospective observational study on 25 patients undergoing THR, observed at 3-month follow-up, and a significant improvement of LBP in the absence of sacral inclination and LL changes [7]. These authors suggest, however, that this lack of change may be related to the radiographic technique rather than to the true clinical posture or gait [7].
Eyvazov et al, in a prospective study on 28 patients with HSS undergoing THR, observed an improvement in LBP levels and postural balance after surgery, but they have recorded neither significant change in spinopelvic alignment after THR, nor a significant correlation between postural changes and LBP reduction [8]. It must be noted that these results may be affected by the limited sample size and the high variability of the data, since these authors recorded postoperatively a posterior shift of the C7 SVA and a change of SS and PT in the range of 1°–2°, but they did not result statistically significant [8].
In the field of spinal surgery, on the other hand, interesting acquisition has been achieved in the last years. Lafage et al, in retrospective study on 70 patients undergoing pedicle subtraction osteotomy (PSO) for spinal imbalance, reported that an increase of LL has a strong negative correlation with a PT reduction [27].
Buckland et al, in a retrospective study on 33 patients with spinal deformities who had undergone THR prior to recruitment, evaluated the spinopelvic parameters and the acetabular cup anteversion before and after (6–12 weeks postoperatively) spinal realignment surgery. A significant acetabular anteversion cup reduction was observed after spinal surgery; this change correlated with PT, SS, SVA, and TPA changes [28].
In the current study, we investigated the relationship between FNA, LBP, and spinopelvic parameters, in patients undergoing THR for primary unilateral HOA. Thus, we recruited 91 patients with severe unilateral HOA, i.e., grade 5 (36 patients out of 91; 39.56%) or grade 6 (55 patients out of 91; 60.04%) according to Turmezei [11] (Table 1), and severe functional limitation of the hip, defined as HHS <60. We finally compared 47 patients with concomitant LBP and primary unilateral HOA (Group-A) to 44 patients with only primary unilateral HOA (Group-B) undergoing THR; all the patients underwent clinical and radiological evaluations at recruitment and at 6-month follow-up.
It is reported that in adults, FNA averages between 8° and 14°, with an average of 8° in men and 14° in women [29] and a high FNA is a proved risk factor for HOA [9, 10].
In this study, Group-A patients showed, at recruitment, a higher FNA angle at the arthritic hip, compared with the contralateral normal hip FNA, while, surprisingly, no significant differences in FNA between the two hips were observed in Group-B (Table 2). The ΔFNA observed in Group-A influenced the CA, since no differences were observed in AA between the two hips. These ΔFNA and ΔCA were strongly related to Spine-VAS, Hip-VAS, ODI, and RM in Group A patients (Table 3). Even if the arthritic hip showed in Group-A a more anteverted femoral neck, compared with Group-B arthritic hip FNA, this difference was not significant. We concluded, therefore, in patients with unilateral HOA, the FNA of the arthritic hip should be compared to the contralateral normal one, because ΔFNA between the two hips has an important role in the genesis of both hip and low back pain.
Previous studies have reported an asymmetric hip range of movement (ROM) in patients with LBP [30]. Tanaka et al., in a cross-sectional study on 35 patients with unilateral HOA, have recently noted that an asymmetric hip flexion reduction may explain LBP in this kind of patients [31]. The present study shows that besides the hip ROM asymmetry, also a structural asymmetry between the two hips is implicated in the pathogenesis of LBP in patients with unilateral HOA. This new finding may help to better understand the interrelation between hip and spine.
The spinopelvic parameters of all patients were assessed before and 6 months after THR. At recruitment, in Group-A patients, we observed a higher LL, SS, PI, SVA (C7), and a lower PT and T1-SPI compared with Group-B subjects. The classification by Legaye et al. [15] was used to describe the sagittal imbalance patterns observed at recruitment. These authors assessed the relationship between PI and SS (SS = (PI × 0.5481) + 12.7° [±6.39°]), as well as between SS and LL (LL = (SS × 1.087) + 21.61° [±4.16]) and identified three typical patterns of perturbation of the sagittal balance [15]. The first one shows an SS conforming to the value determined by the PI, with an observed value for LL which is excessive with regard to the theoretical value calculated according to the SS. In this pattern, the hyperlordosis observed is a compensatory mechanism for the excessive kyphosis in the upper spinal segments [15]. The second pattern has an observed SS excessive with regard to the value determined by the PI, but the LL is adapted to the observed SS; in this situation, the excessive SS results from a flexion deformity of the hips and the high value for LL reflects the spinal compensation of this excessive slant of the pelvis [15]. The third pattern is a lower value of SS with regard to the PI and a low value for LL. In this case, the disruption is caused by a stiff hypolordosis that forces the pelvis to a horizontalisation of the SS to keep the trunk from tilting forward [15]. In this study, preoperatively 44 patients out of 47 (93.6%) showed a type II sagittal balance pattern according to Legaye et al. [15] in Group-A, while in only two patients, out of 44 (4.5%) was observed this sagittal pattern in Group-B. These data confirm that patients with HOA and concomitant LBP have an observed SS which is excessive, with regard to the value determined by PI due to the fixed hip flexion; LL, however, is adapted to the observed SS, since it reflects the spinal compensation of the excessive slant of the pelvis [15].
At 6-month follow-up, a significant change of the hip HRQoL scores was recorded in both groups (Table 6). In Group-A patients, furthermore, a significant change of the spine HRQoL scores and some changing in the sagittal balance were observed, i.e., an increase of PT and a reduction of SS, LL, TK, and TPA (Table 6).
Pelvic tilt is commonly recognized as a compensatory mechanism that the subject uses to maintain an economic standing position [32]. After THR, we observed a significant increment of PT (Table 6). Thus, we have reported that in patients with severe HOA and concomitant LBP, PT reduces to compensate the hip fixed flexion; after THR, may be achieved a restoration of physiological PT. Similar data were reported by Weng et al. [6], who observed a lower PT in patients with concomitant HOA and LBP, compared with asymptomatic controls.
Sacral slope is the spinopelvic parameter which completes the geometrical relationship where “Pelvic Incidence = Pelvic Tilt + Sacral Slope” [32]; PI is a morphologic parameter, specific to each individual in adulthood, which defines the shape of the pelvis independently from its spatial orientation [33]. At 6-month follow-up, we recorded a significant SS reduction (p = 0.0001).
A significant change of LL (p = 0.007) was observed after THR in Group-A patients, whereas the change of LL observed in Group-B, in the order of 2°, was not significant. The higher LL recorded in Group-A at recruitment, together with the different change of LL observed in the two groups after THR, depicts that hyperlordosis may also be implicated in LBP genesis in patients with HSS, as hypothesized by Offierski and MacNab.
It must be noted, however, that the true impact of LL on LBP is not easy to asses, because the definition of pathological lordosis is somewhat challenging. Different formulas have been proposed to predict the ideal lordosis [32, 34, 35], but these methods provide contrasting findings, so that the same patient may result normolordotic or hyperlordotic, according to the the formula that we applied.
Schwab et al. [32] developed the formula LL = PI + 9° (±9°), estimating LL from mean PI based on 75 asymptomatic adult subjects (mean age: 48 years, SD: 18). The authors, however, have not detailed the characteristic of the recruited subjects, so this formula may have a limited validity, especially in patients with a pathologic LL.
Aurouer et al. [34] used the equation LL = 32.56 + 0.54 × PI and developed by Gille, to plan preoperatively the correction of sagittal deformity of the spine in 11 patients (female = 9; male = 2; mean age = 53.8; range 36–73). Even these authors have developed a very accurate planning method, they have not detailed how the formula for LL calculation was obtained. Moreover, Aurouer et al. applied this formula to 11 patients only, so the small sample size is another limitation of this method.
Le Huec and Hasegawa [35] have recently published the most accurate method of LL calculation: LL = 0.54 × PI + 27.6. This equation was obtained analysing 268 Caucasian (n = 137) and Japanese (n = 131) asymptomatic subjects even if it can be critically considered inaccurate due to a wide age range (range 18–76; mean = 37.2) and to a lack of ODI and SRS-22 questionnaire, to exclude subjects with LBP.
This study has some limitations: although our sample size is quite large, our follow-up is limited to 6 months. The patients recruited in this study, however, will be evaluated in a longer follow-up time to assess the long-term impact of the clinical and radiological changes here reported.
After THR, we did not performed a hip CT to calculate the femoral stem anteversion and the acetabular cup anteversion, because for the current study, we performed the routine imaging protocol used for patients undergoing THR at our institute.
Finally, the clinical and radiological changes observed in this study have to be investigated in patients with bilateral HOA and concomitant LBP, to assess the role of bilateral versus unilateral THR on the sagittal balance.
Conclusion
This study showed that patients suffering for concomitant severe primary unilateral HOA and LBP had a significantly different FNA between the two hips, with a more anteverted femoral neck observed at the arthritic hip. This asymmetry in hip FNA is strongly related to LBP, thus a new connection between hip and spine pathology has been discovered. This new acquisition explains why THR should performed primarily in patients with secondary HSS and, at the same time, provides an explanation for the concomitant relief of both hip and low back pain observed after THR, in such a kind of patients.
The spinopelvic misalignment observed in patients with concomitant unilateral HOA and LBP, in the absence of spine structural pathologies, reflects an antalgic posture developed by the patients to keep spine as vertical as possible. After THR, a significant increase of PT and a significant reduction of SS, LL, TK, and TPA are recorded.
Change history
28 April 2017
An erratum to this article has been published.
References
Zhang Y, Jordan JM (2010) Epidemiology of Osteoarthritis. Clin Geriatr Med 26(3):355–369
Deyo RA, Dworkin SF, Amtmann D et al (2014) Focus article: report of the NIH task force on research standards for chronic low back pain. Eur Spine J 23:2028–2045
Chimenti PC, Drinkwater CJ, Li W et al (2016) Factors associated with early improvement in low back pain after total hip arthroplasty: a multi-center prospective cohort analyses. J Arthrop 31:176–179
Staibano P, Winemaker M, Petruccelli D et al (2014) Total joint arthroplasty and preoperative low back pain. J Arthroplasty 29(5):867
Offierski CM, MacNab I (1983) Hip-spine syndrome. Spine (Phila Pa 1976) 8:316–321
Weng WJ, Wang WJ, Wu MD et al (2015) Characteristics of sagittal spine–pelvis–leg alignment in patients with severe hip osteoarthritis. Eur Spine J 24:1228–1236
Ben-Galim P, Ben-Galim T, Rand N et al (2007) Hip-Spine Syndrome. The Effect of Total Hip Replacement Surgery on Low Back Pain in Severe Osteoarthritis of the Hip. Spine (Phila Pa 1976) 32(19):2099–2102
Eyvazov K, Eyvazov B, Basar S et al (2016) Effects of total hip arthroplasty on spinal sagittal alignment and static balance: a prospective study on 28 patients. Eur Spine J. doi:10.1007/s00586-016-4696-9
Terjesen T, Benum P, Anda Svein et al (1982) Increased femoral anteversion and osteoarthritis of the hip joint. Acta Orthop Scand 53(4):571–575
Zandi B, Hozhabri H (2015) Correlation between femoral neck anteversion in patients with osteoarthritis of the hip and normal controls. Patient Saf Qual Improv. 3(2):206–210
Turmezei TD, Fotiadou A, Lomas DJ et al (2014) A new CT grading system for hip osteoarthritis. Osteoarthritis Cartilage. 22(10):1360–1366
Hernandez RJ, Tachdjian MO, Poznanski AK et al (1981) CT determination of femoral torsion. AJR 137:97–101
Reikeråls O, Bjerkreim I, Kolbenstvedt A (1983) Anteversion of the Acetabulum and Femoral Neck in Normals and in Patients with Osteoarthritis of the Hip. Acta Orthop Scand 54(1):18–23
Morvan G, Mathieu P, Vuillemin V et al (2011) Standardized way for imaging of the sagittal spinal balance. Eur Spine J 20(Suppl 5):S602–S608
Legaye J (2005) Duval-Beaupere G Sagittal plane alignment of the spine and gravity: a radiological and clinical evaluation. Acta Orthop Belg 71:213–220
Boulay C, Tardieu C, Hecquet J et al (2006) Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J 15(4):415–422
Legaye J, Duval-Beaupere G, Hecquet J et al (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7:99–103
Obeid I, Hauger O, Aunoble S et al (2011) Global analysis of sagittal spinal alignment in major deformities: correlation between lack of lumbar lordosis and flexion of the knee. Eur Spine J 20(Suppl 5):681–685
Vaz G, Roussouly P, Berthonnaud E, Dimnet J (2002) Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J 11(1):80–87
Chaleat-Valayer E, Mac-Thiong JM, Paquet J et al (2011) Sagittal spino-pelvic alignment in chronic low back pain. Eur Spine J 20(Suppl 5):634–640
Roussouly P, Pinheiro-Franco JL (2011) Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. Eur Spine J 20(Suppl 5):609–618
Mangione P, Gomez D, Senegas J (1997) Study of the course of the incidence angle during growth. Eur Spine J 6:163–167
Mac-Thiong JM, Labelle H, Berthonnaud E et al (2007) Sagittal spinopelvic balance in normal children and adolescents. Eur Spine J 16:227–234
Barrey C, Roussouly P, Perrin G et al (2011) Sagittal balance disorders in severe degenerative spine. Can we identify the compensatory mechanisms? Eur Spine J 20(Suppl 5):626–633
Weng W, Wu H, Wu M et al (2016) The effect of total hip arthroplasty on sagittal spinal-pelvic-leg alignment and low back pain in patients with severe hip osteoarthritis. Eur Spine J 25(11):3608–3614
Yoshimoto H, Sato S, Masuda T et al (2005) Spinopelvic alignment in patients with osteoarthrosis of the hip: a radiographic comparison to patients with low back pain. Spine (Phila Pa 1976) 30:1650–1657
Lafage V, Schwab F, Vira S et al (2011) Does vertebral level of pedicle subtraction osteotomy correlate with degree of spinopelvic parameter correction? J Neurosurg Spine 14(2):184–191
Buckland AJ, Vigdorchik J, Schwab FJ et al (2015) Acetabular anteversion changes due to spinal deformity correction: bridging the gap between hip and spine surgeons. J Bone Joint Surg Am 97:1913–1920
Gulan G, Matovinović D, Nemec B et al (2000) Femoral neck anteversion: values, development, measurement, common problems. Coll Antropol 24(2):521B–527B
Cibulka MT, Sinacore DR, Cromer GS et al (1998) Unilateral hip rotation range of motion asymmetry in patients with sacroiliac joint regional pain. Spine (Phila PA 1976) 23:1009–1015
Tanakaa S, Matsumotoa S, Fujii K et al (2015) Factors related to low back pain in patients with hip osteoarthritis. J Back Musculoskelet Rehabil 28:409–414
Schwab F, Lafage V, Patel A et al (2009) Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila PA 1976) 34:1828–1833
Le Huec JC, Aunoble S, Philippe L et al (2011) Pelvic parameters: origin and significance. Eur Spine J 20(Suppl 5):564–571
Aurouer N, Obeid I, Gille O et al (2009) Computerized preoperative planning for correction of sagittal deformity of the spine. Surg Radiol Anat 31:781–792
Le Huec JC, Hasegawa K (2016) Normative values for the spine shape parameters using 3D standing analysis from a database of 268 asymptomatic Caucasian and Japanese subjects. Eur Spine J 25:3630–3637
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
The name "Carlotta Martini" was missed out in the author group of original version. It has been updated now.
An erratum to this article is available at https://doi.org/10.1007/s00586-017-5092-9.
Rights and permissions
About this article
Cite this article
Piazzolla, A., Solarino, G., Bizzoca, D. et al. Spinopelvic parameter changes and low back pain improvement due to femoral neck anteversion in patients with severe unilateral primary hip osteoarthritis undergoing total hip replacement. Eur Spine J 27, 125–134 (2018). https://doi.org/10.1007/s00586-017-5033-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5033-7