Abstract
Purpose
Sagittal spinopelvic malalignment has been reported in spinal disorders such as low back pain (LBP), and restoration of normal alignment is targeted when treating these disorders. Abnormal sagittal spinal–pelvic–leg alignment has been reported in patients with severe hip osteoarthritis (OA), who have a high prevalence of associated LBP. This prospective longitudinal study aimed to investigate changes in sagittal spinal–pelvic–leg alignment after total hip arthroplasty (THA) in patients with severe hip OA, and whether these changes contribute to LBP relief.
Methods
Patients undergoing primary THA due to severe unilateral hip OA were recruited. Physical examination and X-ray films were taken to rule out any spinal disorder. Sagittal alignment of pelvis, hip, and spine was analyzed on lateral radiographs taken before (baseline) and 1 year after (follow-up) THA. Functional instruments were completed by patients including: visual analog scale (VAS) for LBP, Roland–Morris Disability Questionnaire (RMDQ), and Harris Hip Score (HHS). Comparisons were carried out at baseline and follow-up, and between patients with and without LBP.
Results
The recruited 69 patients showed significantly reduced hip flexion and improved global spinal balance at follow-up compared with baseline. LBP was reported by 39 patients (56.5 %) before surgery; at follow-up, 17 reported complete resolution, while 22 reported significant relief. Significant decreases in VAS and RMDQ scores in lumbar spine and increase in hip HHS were observed.
Conclusions
THA in patients with severe hip OA could help correct abnormal sagittal spinal–pelvic–leg alignment and relieve comorbid LBP. Improvements in hip flexion and global spinal balance might be involved in the mechanism of LBP relief.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Normal alignment of the spine, pelvis, and lower limbs in the sagittal plane is critical to maintain an upright standing position with the least muscle energy expenditure and discomfort in human [1–3]. Abnormal sagittal spinal–pelvic–leg alignment has been identified in spinal disorders and in turn, could deteriorate to disorder such as chronic low back pain (LBP) [4, 5]. Restoration of normal sagittal alignment is prioritized in the management of these disorders to relieve LBP and to achieve good long-term outcome. In addition to spinal disorders, abnormal sagittal spinal–pelvic–leg alignment was also documented [6, 7] in patients with severe hip osteoarthritis (OA), and our recent study demonstrated flexed hip deformity, anteverted pelvis, forwardly inclined global spine, and increased risk of spinal imbalance in such patients compared with asymptomatic controls [6]. Whether these abnormalities could be corrected by total hip arthroplasty (THA), however, remains to be reported.
In older adults, LBP is a common symptom with the reported prevalence varied from 12 to 15 % [8, 9]. However, in patients with severe hip OA, the prevalence of LBP could rise from 21.2 to 49.4 % in different large cohort studies [10–13]. There was even absolute prevalence reported from a small sample size study [14]. Despite this, it is worth noted that 54–100 % of patients reported relief of LBP after THA for the affected hip [11–15]. Offierski and MacNab [16] proposed that the LBP comorbid to hip OA might be caused by hip flexion deformity, which rotates the pelvis forward and exaggerates the normal lumbar lordosis, subsequently results in further subluxation of the posterior facets and giving rise to LBP [16]. They believed that once the flexion deformity was corrected, the hyperlordosis of the lumbar spine would be overcome with the spinal symptoms being relieved [16]. To our best knowledge, this hypothesis remains to be validated.
We therefore carried out a prospective study to investigate the changes in sagittal spinal–pelvic–leg alignment after THA in patients with severe hip OA, and whether these changes would contribute to the relief of LBP.
Materials and methods
This was a prospective study of the sagittal spinal–pelvic–leg alignment and clinical outcome of LBP in patients with severe hip OA. The study was approved by the Hospital Clinical Research Ethics Committee, and informed consent was obtained from all participants.
Patients with a primary diagnosis of unilateral hip OA who elected to undergo primary THA were recruited. The following exclusion criteria were applied: (1) marked OA symptoms in the knee, ankle, or contralateral hip; (2) arthritis secondary to other diseases in the hip, e.g., rheumatoid arthritis, ankylosing spondylitis, and developmental dysplasia; (3) history of surgical intervention in the spine, hip, or lower leg; (4) neurologic deficit in the lower leg; (5) other diseases that would affect the sagittal alignment of the spine, pelvis, and lower leg, including spinal deformity, spondylolistheses, and history of fracture. Furthermore, following radiographic imaging, subjects with skeletal abnormalities other than the index hip, such as severe osteophytes, vertebral collapse, spondylolisthesis, or scoliosis, were also excluded.
THA was carried out by two senior consulting arthroplasty surgeons, using a lateral modified Hardinge approach and a cementless prosthesis. The patients were examined preoperatively and at 3, 6 months, and 1 year postoperatively. At pre-operation (baseline) and 1-year post-surgery follow-up, lateral digital radiographs of the spine, pelvis, and proximal femur were taken with the subject standing upright [6]. In addition, the following functional instruments were completed by the patients: a visual analog scale (VAS) to assess the presence and severity of LBP in the previous 3 months, the Roland–Morris Disability Questionnaire (RMDQ) to evaluate the function of the lumbar spine, and the Harris Hip Score (HHS) to determine the function of the index hip.
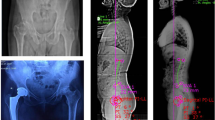
To quantify the sagittal spinal–pelvic–leg alignment, the following parameters were measured on the lateral X-rays using Surgimap Spine software (version 2.0.7; Nemaris Inc., NY, USA) as our previous study (Fig. 1) [6]. (1) Sagittal alignment of the pelvis and hip was measured by pelvic incidence (PI), pelvic tilting (PT), sacral slope (SS), pelvic femoral angle (PFA), and femoral inclination (FI), while (2) sagittal alignment and balance of the spine were measured by lumbar lordosis (LL) and T1 spinal–pelvic inclination (T1-SPI). To assess the accuracy in identifying the center of the hip after THA, the PI was measured by two independent researchers, and intra-observer reliability was then computed. If the contralateral femoral head overlapped the acetabulum cup, the center of the implanted femoral head was defined as the center of the hip.
Illustration of the radiographic parameters of the sagittal alignment of the spine, pelvis and hip. a Parameters of the pelvis and hip joint. b Parameters of the spine. FI femoral inclination, LL lumbar lordosis, PI pelvic incidence, PFA pelvic femoral angle, PT pelvic tilt, SS sacral slope, T1-SPI T1 spinal–pelvic inclination
Statistical analysis
Data analysis was performed using the Statistical Package for the Social Sciences (version 13.0, SPSS, Inc., Chicago, IL, USA). The data collected from baseline and follow-up were compared by paired t test, while data between patients with and without LBP were compared by Student’s t test. The level of significance was defined as P ≤ 0.05.
Results
Although 97 patients were recruited consecutively into the prospective study and met the criteria of being at least 1 year after operation at the time of analysis, 23 patients refused to follow-up, one patient had a peri-prosthetic fracture due to a fall 7 months postoperatively, and the questionnaires of four other patients were incomplete. As a result, a total of 69 patients (25 men and 44 women) completed the full study assessments, with an average age of 62.7 ± 9.9 years. Reliability analysis showed excellent intra-observer agreement in the postoperative PI (intraclass correlations = 0.872).
The sagittal alignment parameters are summarized in Table 1. At 1 year after operation, patients showed comparable LL, SS, PT, and PI to those measured before surgery, indicating no significant changes in lumbar and pelvic alignments. By contrast, there was significantly larger PFA, but smaller FI at 1 year after surgery when compared with baseline. This showed that THA had significantly reduced hip flexion. In addition, the T1-SPI at 1 year after surgery was significantly different from that before surgery, suggesting improved spinal balance on the sagittal plane (Fig. 2). Moreover, when compared with the asymptomatic controls [6], patients with severe hip OA showed significant differences in SS, PFA, T1-SPI, and FI before surgery, and in SS, PFA, and T1-SPI at 1 year after surgery.
Illustration of the change of sagittal alignment in patients with ipsilateral HOA by THA. A female aged 56 years underwent right THA. The patient showed poor sagittal spinopelvic alignment before operation a with the C7 plumb line located anterior to femoral head line, and flexed hip with backward femoral inclination. At 1 year after operation b the sagittal spinopelvic alignment was significantly improved. The C7 plumb line located on the S1 vertebra. In addition, the patient showed reduced fixed hip flexion and less femoral backward inclination
Of the 69 patients recruited, 39 reported LBP before surgery, giving an incidence of 56.5 %. At 1 year postoperatively, 17 reported complete resolution of LBP, while the remaining 21 patients reported significant pain relief compared with baseline. No patient required any medication to relieve LBP in the 3 months prior to the 1-year follow-up. The mean VAS score for LBP decreased from 4.6 before surgery to 1.5 at 1 year after THA (Table 2). A similar trend of improvement was also found in the RMDQ score in these patients. In patients both with and without LBP, the HHS had increased significantly at 1 year after surgery. There was no difference observed between the two groups in HHS before or at 1 year after THA, or in changes to HHS after operation.
In comparing the sagittal alignment between patients with and without LBP, it showed no significant difference between baseline and 1 year after surgery. Patients in both groups showed comparable changes in hip flexion and restoration of spinal balance after THA.
Discussion
In this study, patients with severe hip OA treated by THA were followed up for at least 1 year. Our results showed that the abnormal sagittal spinal–pelvic–leg alignment in these patients was significantly corrected, although it was still different from that of asymptomatic controls [6]. In addition, the LBP reported by 56.5 % of patients before surgery was significantly relieved at 1 year after THA. These findings indicate that THA not only treated the hip disease, but also helped to correct sagittal balance and relieve LBP in patients with severe hip OA.
Abnormal sagittal spinal–pelvic alignment has been documented in patients with LBP [5], and the importance of its role in the pathogenesis of LBP was strengthened [4]. Hence, the finding of abnormal sagittal spinal–pelvic–leg alignment in patients with severe hip OA by our previous study [6] raised the question of whether the treatment of severe hip OA by THA could correct the sagittal malalignment. The results of the current study showed comparable SS, PT, and LL before and at 1 year after operation, indicating that THA did not result in any significant change in the sagittal alignment of the pelvis and lumbar spine. Lack of significant changes in SS and LL in patients with hip OA was also reported by Ben-Galim et al. [14] and Radcliff et al. [17], at 3 and 9 months after THA, respectively (Table 3). However, the significant increase in PFA and decrease in FI at 1 year after THA compared with baseline indicated less flexion of the hip joint, while a more negative value in T1-SPI suggested greater backward inclination of the spine and reduced spinal imbalance. It should note that at 1 year after THA, the PFA and T1-SPI findings in patients with hip OA were still different from those in asymptomatic controls [6], but the differences were reduced compared with the measurements before surgery. These findings suggested that THA could partially correct the abnormal sagittal spinal–pelvic–leg alignment in patients with severe hip OA.
LBP is common in patients suffering from hip OA [11–14]. By excluding disorders of the lumbosacral spine by plain radiology, Hsieh et al. [12] found that 21.2 % of patients with severe hip OA had chronic LBP. In the present study, we found a rate of 56.5 % (39/69). Despite the high prevalence of LBP in our patients with hip OA, previous [11, 14, 15] and the present study found that LBP in these patients could be relieved by THA, with some having complete resolution (Table 4). At 1 year after THA, Staibano et al. [11] found that LBP rated as “moderate” to “worst imaginable pain” was significantly improved in 54 % (44/82) of patients with hip OA, and Parvizi et al. [13] reported resolution in 113 of 170 patients (66.5 %). However, these studies did not exclude disorders of the lumbar spine, and could not distinguish whether the remaining LBP was caused by pathogenesis in the hip or the spine. By further analyzing the 150 patients with spine work in the study by Parvizi et al. [13], we found that LBP was resolved in 72 (92 %) of 78 patients without spinal disorders, but only in 41 (57 %) of 72 patients with spinal disorders. In the present study, physical examination and plain film radiography were used to exclude spinal disorders in patients recruited. Our results showed that at 1 year after surgery, 17 patients had complete relief from LBP, and all the others had significant improvement in LBP, presenting significantly decreased VAS score for the back compared with that before THA. None of the patients required any medication to relieve the LBP by the time of the final follow-up. Hence, we conclude that the LBP comorbid to hip OA has a strong chance of being relieved by THA, if there is no coexisting spinal disorder.
The mechanism underlying the relief of LBP by THA in patients with severe hip OA has not been well documented. Considering hip rotation and sagittal spinal alignment, Offierski and MacNab [16] proposed that by correcting the flexion deformity of the hip, the pelvic rotation and the hyperlordosis of the lumbar spine in patients with hip OA would be overcome, resulting in the relief of spinal symptoms. In agreement with this proposal, the present study found that patients with LBP had significant improvement in hip flexion and spinal imbalance, although there was no significant change in pelvic rotation and LL at 1 year after surgery. These changes might reduce the tension of the back muscles and relieve LBP. Furthermore, previous studies [18, 19] have shown that reduced range of motion (ROM) in the hip might contribute to the pathogenesis of LBP, by leading to a greater lumbopelvic rotation in compensation, subsequently inducing increased mechanical stress in the lumbopelvic region. In patients with hip OA, the hip function accessed by the Western Ontario and McMaster Universities Arthritis Index was found to correlate significantly with LBP [10], and limitation of flexion has been identified as an independent risk factor for LBP [20]. In addition, the improved motion in medial and lateral rotation of the affected hip [19, 21], and the reduced asymmetry in the range of hip rotation [22, 23] might also contribute to the relief of LBP after THA in patients with hip OA. In the present study, significantly improved hip motion and function were achieved at 1 year after THA in patients with hip OA, presenting as less hip flexion and improved HHS. These changes might contribute to the relief of LBP.
Some limitations of the present study should be acknowledged. 23 of 97 patients failed to have follow-up at 1 year after THA. When contacted by telephone, we were informed of their self-satisfactory outcome. Hence, they were reluctant to travel afar for us to follow-up. As for the patients analyzed, X-ray radiography was used to exclude any skeletal spinal abnormalities. However, disorders in spinal cord and disks could have been overlooked. In addition, direct assessment of hip ROM was not carried out. Although improved hip flexion was demonstrated by comparing the pre- and postoperative lateral X-rays, the dynamic movement of the hip cannot be accurately represented by a single static radiographic position. Furthermore, other factors such as lifestyle, body mass index, and strength of the trunk muscles, which have previously been reported to be involved in the pathogenesis of LBP, were not assessed in the present study.
Despite these limitations, the present study demonstrated that the abnormal sagittal spinal–pelvic–leg alignment in patients with severe hip OA could be partially restored by THA. LBP is very common in these patients, with a prevalence of 56.5 %, but had a high chance of being relieved by THA. Hence, we are in agreement with Stupar et al. [10] that the management of patients with hip OA also manages their LBP. Thus, the improvement in hip motion and global spinal balance might contribute to the relief of LBP.
References
Le Huec JC, Roussouly P (2011) Sagittal spino-pelvic balance is a crucial analysis for normal and degenerative spine. Eur Spine J 20(Suppl 5):556–557
Le Huec JC, Saddiki R, Franke J et al (2011) Equilibrium of the human body and the gravity line: the basics. Eur Spine J 20(Suppl 5):558–563
Legaye J, Duval-Beaupere G, Hecquet J et al (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7:99–103
Roussouly P, Pinheiro-Franco JL (2011) Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. Eur Spine J 20(Suppl 5):609–618
Chaleat-Valayer E, Mac-Thiong JM, Paquet J et al (2011) Sagittal spino–pelvic alignment in chronic low back pain. Eur Spine J 20(Suppl 5):634–640
Weng W-J, Wang W-J, Wu M-D et al (2014) Characteristics of sagittal spine–pelvis–leg alignment in patients with severe hip osteoarthritis. Eur Spine J 24:1228–1236
Yoshimoto H, Sato S, Masuda T et al (2005) Spinopelvic alignment in patients with osteoarthrosis of the hip: a radiographic comparison to patients with low back pain. Spine (Phila Pa 1976) 30:1650–1657
Knauer SR, Freburger JK, Carey TS (2010) Chronic low back pain among older adults: a population-based perspective. J Aging Health 22:1213–1234
Plouvier S, Gourmelen J, Chastang JF et al (2011) Low back pain around retirement age and physical occupational exposure during working life. BMC Public Health 11:268
Stupar M, Cote P, French MR et al (2010) The association between low back pain and osteoarthritis of the hip and knee: a population-based cohort study. J Manip Physiol Ther 33:349–354
Staibano P, Winemaker M, Petruccelli D et al (2014) Total joint arthroplasty and preoperative low back pain. J Arthroplast 29:867–871
Hsieh PH, Chang Y, Chen DW et al (2012) Pain distribution and response to total hip arthroplasty: a prospective observational study in 113 patients with end-stage hip disease. J Orthop Sci 17:213–218
Parvizi J, Pour AE, Hillibrand A et al (2010) Back pain and total hip arthroplasty: a prospective natural history study. Clin Orthop Relat Res 468:1325–1330
Ben-Galim P, Ben-Galim T, Rand N et al (2007) Hip-spine syndrome: the effect of total hip replacement surgery on low back pain in severe osteoarthritis of the hip. Spine (Phila Pa 1976) 32:2099–2102
Redmond JM, Gupta A, Hammarstedt JE et al (2014) The hip-spine syndrome: how does back pain impact the indications and outcomes of hip arthroscopy? Arthroscopy 30:872–881
Offierski CM, MacNab I (1983) Hip-spine syndrome. Spine (Phila Pa 1976) 8:316–321
Radcliff KE, Orozco F, Molby N et al (2013) Change in spinal alignment after total hip arthroplasty. Orthop Surg 5:261–265
Kim SH, Kwon OY, Yi CH et al (2014) Lumbopelvic motion during seated hip flexion in subjects with low-back pain accompanying limited hip flexion. Eur Spine J 23:142–148
Harris-Hayes M, Sahrmann SA, Van Dillen LR (2009) Relationship between the hip and low back pain in athletes who participate in rotation-related sports. J Sport Rehabil 18:60–75
Tanaka S, Matsumoto S, Fujii K, et al (2014) Factors related to low back pain in patients with hip osteoarthritis. J Back Musculoskelet Rehabil 28:409–414
Cibulka MT, Sinacore DR, Cromer GS et al (1998) Unilateral hip rotation range of motion asymmetry in patients with sacroiliac joint pain. Spine (Phila Pa 1976) 23:1009–1015
Almeida GP, de Souza VL, Sano SS et al (2012) Comparison of hip rotation range of motion in judo athletes with and without history of low back pain. Manual Ther 17:231–235
Van Dillen LR, Bloom NJ, Gombatto SP et al (2008) Hip rotation range of motion in people with and without low back pain who participate in rotation-related sports. Phys Ther Sport 9:72–81
Acknowledgments
This work was supported by the Key Project of the Medical Science and Technology Development Foundation, Nanjing Department of Health (JQX13008, YKK12081, QRX11174), the Six Categories of Top Talents, Jiangsu Provincial Department of Human Resources and Social Security (WSW-002), the Jiangsu Province’s Key Medical Center (ZX201107), the Jiangsu Provincial Special Program of Medical Science (BL2012002) and the Nanjing clinical Medical Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Weng, W., Wu, H., Wu, M. et al. The effect of total hip arthroplasty on sagittal spinal–pelvic–leg alignment and low back pain in patients with severe hip osteoarthritis. Eur Spine J 25, 3608–3614 (2016). https://doi.org/10.1007/s00586-016-4444-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4444-1