Abstract
Purpose
The purpose of this study was to assess long-term follow-up data after anterior cervical decompression and fusion (ACDF) with and without Caspar plating (ACDF + PS) for the treatment of cervical spondylotic myelopathy (CSM) with special focus on functional outcome, pain, and repeat surgery for adjacent segment disease (ASD).
Method
Hospital records of 45 patients who were affected by CSM and underwent ACDF or ACDF + PS at least 17 years ago were reviewed. Information about diagnosis, surgical report, pre- and postoperative clinical process, and complications was analyzed. Clinical outcome was assessed using a standardized questionnaire including the Neck Disability Index (NDI), modified JOA-score, Odom’s criteria, limitations in quality of life, and questions about the current neurological status and pain.
Results
Twenty-three patients with a mean follow-up of 26 years were evaluated. ACDF was performed in nine and ACDF + PS in 14 patients, respectively. At follow-up 78.3% of patients were free of pain, 91.3% had no motor deficit, 73.9% had no sensory deficit, and 60.7% had no gait disturbance. The current mean NDI is 14% (range 2–44%), the mean modified JOA-score was 17.2 (range 15–18). According to Odom’s criteria 78.3% of patients had clinical success. In four patients repeat surgery was indicated due to pseudarthrosis or symptomatic ASD (17.4%).
Conclusions
ACDF and ACDF + PS yield significant decrease in neck pain, a significant increase in sensorimotor function and a high rate of clinical success. Patients with preoperative gait disturbance completely recovered in about 60% of cases. Overall prevalence for ASD was 17.4% after 25 years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical spondylotic myelopathy (CSM) is the most common disease of the cervical spine in adults over 55 years [1]. CSM is a degenerative process of the cervical intervertebral disc, the uncovertebral joint, the facet joint, the posterior longitudinal ligament, the vertebral body, and the ligamentum flavum. The clinical course can range from periods of non-progressive disease to step-wise deterioration to rapidly advanced clinical myelopathy is variable. The progression of degeneration of the aforementioned anatomical structures may result in spinal cord compression with significant disability [2, 3]. Currently there is no consensus and no clear clinical data if anterior, posterior, or combined (anterior and posterior) approach will lead to the best clinical outcome [4–6]. Traditionally, the anterior approach was favored in one-or two-segment procedures, and at the presence of regional kyphosis [3]. However, anterior approaches are criticized for increased graft- and surgery related complications in multilevel procedures and the development of adjacent segment disease (ASD) [7]. To the best of the authors` knowledge this study is the first that investigated the clinical outcome of patients who underwent ACDF and ACDF + PS for the treatment of cervical spondylotic myelopathy with a mean follow-up of over 25 years.
Materials and methods
Patient population
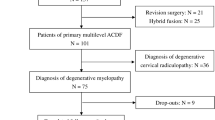
We retrospectively reviewed files of patients who had undergone surgical treatment for CSM.
Inclusion criteria were patients who underwent ACDF or ACDF + PS with an autologous iliac crest bone (AICB) at least 17 years ago, full documentation of detailed preoperative neurological status, a detailed surgical report, detailed postoperative in hospital course, detailed neurological status at discharge and full contact information.
Out of 126 patients, 45 fulfilled the inclusion criteria. Eighty-one patients were excluded because of a too short follow-up (1 patient), fusion without the use of AICB (15 patients), incomplete clinical documents (2 patients) or incomplete contact details (63 patients).
We were able to contact 40 out of 45 patients (88.9%). Five patients could not been contacted (11.1%). Twenty-three of 40 patients participated at the study (57.5%), 10 patients were not interested in participating without giving reasons (25.0%), and 7 patients were either dead or mentally and physically neither able to conduct the questionnaires nor to attend at our institution (12.5%). Eighteen out of 23 patients who completed the questionnaire attended a personal follow-up at our institution (78.3%). The study was approved by local ethical committee. Informed consent was obtained from all individual participants included in the study.
Pre- and postoperative neurological status and questionnaire
Each patient`s file was reviewed carefully. The preoperative and postoperative physical examination status of each patient was assessed according to the documentation in the patients file with special focus on symptoms which are associated with CSM, such as motor dysfunction, sensory dysfunction, abnormal brisk reflexes, pathological reflexes, pathological muscle tonus such as spasticity or weakness, disturbed fine motor activity, disturbed gait pattern and bladder dysfunction. The clinical diagnosis was made by physical examination, myelography, computed tomography-myelography, and magnetic resonance imaging.
A detailed telephone interview was performed to inquire the recovery process of each patient after discharge. The participants were asked about the postoperative recovery concerning sensorimotor deficits and other symptoms associated to CSM; as well as neck pain, which was assessed by the numeric pain rating scale (NPRS). Furthermore, each participant was asked about limitations in their daily life which were associated with the procedure, and about limitations in their daily life which were associated with iliac crest bone graft donor site. Each participant completed a standardized questionnaire which assessed the functional outcome according to Odom’s criteria (Table 1), Neck Disability Index (NDI), and Benzel´s modified JOA scale (mJOA) (Table 2). The patient`s quality of life was assessed using only the five questions of the EQ-5D questionnaire (Table 3), and HADS-Scale was used to detect if patient had emotional disorder. In addition to the telephone interview and questionnaire, a personal examination was offered to each patient.
Statistical analysis
The SPSS statistical software package (IBM, Armonk, NY, USA) was used for statistical analysis of the data. We used Fisher’s exact Tests and Fisher-Freeman-Halton exact Test to compare relative frequencies of a binary outcome and an outcome with more than two categories between two independent groups, respectively. The Wilcoxon was used to compare non-parametric paired sample tests and Mann–Whitney U test was applied for the comparison of a quantitative non-normal outcome between two groups. Any p values given were two sided. A p value of <0.05 was assumed sufficient to indicate statistical significance.
Results
Twenty-three patients (16 male, 7 female) participated in this study and completed the telephone interview and the questionnaire. Eighteen out of 23 patients attended a physical examination at our department (78.3%). The mean follow-up was 26 years (range 17–36 years). The patients’ mean age at time of ACDF or ACDF + PS was 43 years (range 28–57 years). At follow-up the mean age was 70 years (range 55–82 years).
In none of the preoperative imaging report, and in none of the operation report an ossification of the posterior longitudinal ligament (OPLL) was described. The cause of spinal cord compression was mainly due to disc degeneration and minor posterior spondylophyte formation. A detailed breakdown of all operated segments is shown on Fig. 1.
There was no significant difference regarding gender, surgical technique, and operated segments between the patients who participated in the study and the patients who were lost at follow-up (Two sided Fisher exact test p = 0.790, Two sided Fisher exact test p = 0.193, Fisher-Freeman-Halton test p = 0.867).
There was a significant difference regarding the age of patients who participated in the study and patients who were lost at follow-up (Mann–Whitney U test: p = 0.009).
Preoperative and postoperative neurological status and results of questionnaire
The following data concerning the preoperative and postoperative neurological status is based on the documentation in the patients file. Preoperatively, motor dysfunction such as disturbed fine activity, and weakness were documented in thirteen patients (56.5%), a sensory dysfunction in 18 patients (78.3%), gait disturbance in 20 patients (86.9%), spasticity in 11 patients (47.8%), hyperreflexia in all and pathological reflexes in 14 patients (60.8%), and in one patient a bladder dysfunction (4.3%). In 19 patients, neck pain and limitation of neck rotation due to pain was documented prior to surgery (82.6%).
Postoperatively, an improvement of motor dysfunction was documented in ten patients (76.9%). An improvement of sensory dysfunction were documented in 15 patients (83.3%), an unchanged sensory dysfunction was documented in three patients at discharge (16.7%). Improved gait disturbance was documented in seventeen patients (85.0%), and improved spasticity was documented in nine patients (81.2%). No improvement was documented for bladder dysfunction. In one patient a new sensorimotor deficit was documented postoperatively (4.4%). At discharge in eighteen patients with preoperative pain complete or nearly complete pain relief was documented (94.7%). In none of the cases a new onset of hoarseness or dysphagia was documented.
The following data concerning the neurological status at final follow-up is based on the telephone interview. At final follow-up twenty-one patients reported to have no limitations of their motor strength (91.3%), seventeen patients reported to be free of sensory disturbance (73.9%), fourteen patients reported to have no gait disturbance (60.7%), nine patients reported that initial improvement of gait disturbance was followed by worsening in the course of follow-up (39.1%). All patients reported to have normal micturition (100%).
The median pain intensity decreased from 6.1 (range 0–10) to 2 (range 0–4) on the NPRS (Wilcoxon test: p < 0.001) at follow-up. At the follow-up eighteen patients were free of pain (78.3%) among those two had second surgery at the cervical spine due to symptomatic ASD (11.1%). A compilation of frequency of clinical symptoms is shown on Table 4.
Five patients reported taking pain medication, if required (21.7%). Among those one indicate none (20.0%), two moderate (40.0%) and two serious (40.0%) limitations in their daily activities. The current mean NDI is 14% (range 2–46%), the mean mJOA-score was 16.0 (range 11–18), and the results of the EQ-5D questionnaire are shown on Table 3. The median HADS-score was 4 (range 0–13). Nineteen patients had a score between 0–6 (82.6%) and show normal state of mind. Four patients had a score in the range from 10 to 13 (17.4%). Seventeen patients report no or minor problems in their daily life (73.9%), four patients reported moderate limitations in daily life (17.4%), and two patients reported serious limitations in their daily life (8.7%). At final follow-up none of the patients reported hoarseness or dysphagia. Eighteen patients report good-to-excellent functional recovery according to Odom’s criteria (78.3%).
Concerning pain at the iliac crest donor side (ICDS) the patients reported a mean pain intensity of 1 (range 0–5) on the NPRS, and the mean time period of discomfort was three month (range 0–24 month). Currently, one patient reported to take pain medication temporarily due to discomfort at the iliac crest donor side (4.3%). Two patients reported about smaller limitations in their daily life due to problems at the bone harvest site (8.6%).
A compilation of the clinical outcome after ACDF and ACDF + PS with respect to the number of operated segments is shown on Table 5.
There was no significant difference regarding clinical success according to Odoms, NDI, and mJOA-score between patients operated via ACDF and patients operated via ACDF + PS (Two sided Fisher exact test p = 0.056, Mann–Whitney U test: p = 0.109, Mann–Whitney U test: p = 0.425).
When asked, all patients said they would undergo anterior cervical fusion again, if required.
Neurological examination
Eighteen patients attended a personal examination at our institution. At follow-up examination all patients with preoperative motor dysfunction improved to normal fine motor activity and muscle strength. In one patient, a sensory dysfunction remained unchanged (7.7%), and two patients presented with a new sensibility deficit (11.1%). A mild paresis remained in one patient with a new postoperative sensorimotor deficit. None of the patients presented with pathological reflexes. Seven patients presented with a mild gait disturbance (43.8%), none of the patients needed a hand rail, a cane or a crutch to walk. In one patient, an abnormality in the bladder function was documented preoperatively. At follow-up all of the patients reported normal micturition.
Patients with repeat procedure
Six out of 23 patients underwent repeat procedure (26.1%). In one patient each repeat procedure was performed due to postoperative wound infection, and due to chronic dysphagia with removal of the Caspar plate 13 month after initial ACDF + PS.
In four patients repeat procedure was indicated due symptomatic ASD (17.4%). One patient developed symptomatic ASD due recurrence of CSM at the caudal segment 1 year after initial one-level ACDF (C5/6), one patient developed symptomatic ASD caused by a soft cervical disc herniation at the caudal segment 8 years after initial two-level ACDF (C5–7) the same patient had laminectomy of C4–6 as a third procedure 11 years after initial anterior fusion.
Another patient developed a recurrent CSM caused by pseudarthrosis at the caudal of two index segments 5 years after two-level ACDF (C5–7), and one patient developed symptomatic ASD due recurrence of CSM at the caudal segment 12 years after initial one-level ACDF + PS (C6/7). The preoperative radiological report was focused on the segment(s) that was about to be fused. Rarely information about degenerative changes of the adjacent segment was described. Therefore, no profound conclusion can be drawn about the development of symptomatic ASD in these patients.
There was no significant difference regarding the rate of repeat surgery due to ASD between patients operated via ACDF and patients operated via ACDF + PS (two sided Fisher exact test p = 0.260).
Discussion
Retrospective studies are often criticized for a low follow-up rate. In studies with as follow-up of more than 10 years a lost at follow-up rate of 50% or more is frequently reported [8–13]. In this study, with a mean follow-up of 26 years 57% of patients how fulfilled inclusion criteria participated in the study. However, 25% of the contacted patients were not interested in participating in the study. The exact reason remains unclear, but this loss of patients is a bias to all of the presented outcome percentages.
CSM can be treated safe and effectively via an anterior or posterior approach. The selection of the appropriate operative strategy is influenced by various factors such as the underlying pathology of compression, the dominant side of compression, the number of affected levels, and the curvature of the cervical spine 4, 14]. The anterior approach is favored in case of soft disc herniation, concomitant severe axial neck pain and kyphosis. Its advantage is the ability of resecting the object which compresses the spinal cord and its vascular supply by removing the disc, the posterior longitudinal ligament and posterior spondylophyte formation. In general anterior, approaches are preferred in one-to-two-level disease but its effectiveness has been demonstrated in multilevel procedures [15, 16]. However, multilevel ACDF using autologous iliac crest graft is performed less frequently due to ICDS morbidity and the fact that patient satisfaction is very high with bone graft substitutes compared with autograft [17]. In out series, 8.6% of patients reported about limitations due to the bone harvest even more than 20 years after the procedure.
Additional anterior cervical plating is recommended for restoration of the sagittal alignment, to reduce graft collapse or graft dislocation, and to achieve higher fusion rates in one-three level procedures [18–21].
Despite all the advantages the anterior approach is associated with higher complication rate, a higher reoperation rate, more blood loss and a longer surgical time. However, the aforementioned has no influence on patients` postoperative recovery because the length of hospital stay has also been reported to be shorter after anterior approach [22, 23]. In this series, adding of a cervical plate was the cause for repeat procedure (i.e. plate removal due to chronic dysphagia) in 7.1% of cases. In none of the cases implant related complications (i.e. plate breakage) or pseudarthrosis occurred.
If pseudarthrosis is considered to be associated to ACDF without plating then the rate for repeat procedure specific to the surgical technique is 11.1%. However, due to the fact that this is a series with only 23 patients and no preoperative and follow-up radiographic data no profound conclusion can be made whether cervical plating offers a benefit or not.
The natural history of CSM is more likely one of neurological deterioration. The neurological deterioration after anterior and posterior approach is not well investigated in a long-term follow-up because the number of studies with a follow-up of more than 15 years is rare.
There is only 1 paper by Kawaguchi et al. with a 20-year follow-up study for the treatment of cervical myelopathy via “en bloc” laminoplasty in the literature. At last follow-up about 50% of patients showed worsening of the JOA-score (mean JOA-score was 10.6) and 60% of patients had a loss of their cervical lordosis.
Kawaguchi et al. stated that cause of deterioration in the majority of patients was caused by pathologies other than myelopathy. A closer look on the listed pathologies shows that 40.6% of patients were operated on spinal or musculoskeletal disorders, 37.5% had a cognitive disorder or stroke and in 21.8% of cause for deterioration were unknown. The mean mJOA-score of this study was 16.0 points and, therefore, much closer to normality compared to Kawaguchi’s cohort.
There is no obvious explanation for the difference in the clinical outcome between Kawaguchi’s series and our series of patients. But three aspects should be reconsidered. First, the average age of patients in this study was 7–10 years younger, which might have significant influence to the physical status of our participants.
Second, none of our participants had a cognitive disorder or stroke, which again might have significant influence too.
Third, a lordotic curvature and a decrease of the sagittal vertical axis are important factors to achieve good clinical outcome. However, the restoration of the cervical alignment can be achieved via ACDF but this is influenced by several factors such as the number of levels fused, the preoperative status of degeneration and the alignment of the upper cervical spine. Further, spine surgeons should be aware that ACDF might achieve segmental lordosis by increasing kyphosis in non-fused levels [24].
Therefore, influence of the cervical alignment on the clinical outcome might be greater than the repeat procedure rate which was 9.5% in Kawaguchi’s series and, therefore, lower compared to this study (i.e., 17.4%) [10].
However, the authors have no radiographic data of these patients to prove this theory. Since the pathophysiology for the development of symptomatic ASD is poorly understood no conclusions can be made whether ACDF is correlated with acceleration of adjacent segment degeneration. A multitude of studies have addressed and debated about this question in the past two decades but there is still no consensus. The design of this study is not suited to thoroughly address the question of symptomatic ASD since several factors such as the interbody graft, the number of levels fused, the use of instrumentation, smoking, and other patient related factors might have influence on the development of symptomatic ASD. A worsening of the clinical outcome and JOA score after posterior approach via laminoplasty in a more than 10 year follow-up as well as after anterior approach in a 7 year follow-up study has been also reported by several other authors [8, 9, 21, 25].
Similar to the aforementioned findings the results of this study demonstrate that patients initially showed an improvement of their preoperative symptoms which was followed by worsening in the course of a long-term follow-up.
Postoperatively, in our study 95.6% of patients reported to be free of neck pain or an improvement to almost no neck pain, respectively. At final follow-up the rate of patients decreased to 78.3% of patients who reported to be free of pain. Further, 39.1% of patients reported that initial improvement of their gait disturbance was followed by worsening. Some might argue that this is caused due to accelerate degeneration of the adjacent segments after fusion. However, in the clinical examination no obvious signs for myelopathy were detected. Therefore, a deterioration of the patient’s physical activity caused by aging might be more reasonable.
Adding a cervical plate is recommended to preserve cervical lordosis which is believed to be associated with better clinical outcome [18, 19].
Our findings showed no significant difference in the reoperation rate between ACDF and ACDF + PS. However, the comparison of clinical success according to Odoms of the two groups showed a marginal trend towards significance for better clinical outcome in patients treated with ACDF + PS (p = 0.056).
In the practice the choice of treatment is left to the surgeon. The results of this study have demonstrated the effectiveness of ACDF and ACDF + PS with a very good clinical success rate of 78.3% for the treatment of CSM over a period of more than 20 years.
Conclusions
ACDF and ACDF + PS offer a high clinical success rate of 78.3%, rate of repeat surgery was 17.4% due to symptomatic ASD within 25 years. Worsening of gait disturbance was documented in about 40% of cases in the course of follow-up.
References
Toledano M, Bartleson JD (2013) Cervical spondylotic myelopathy. Neurol Clin 31(1):287–305. doi:10.1016/j.ncl.2012.09.003
Tetreault L, Goldstein CL, Arnold P, Harrop J, Hilibrand A, Nouri A, Fehlings MG (2015) Degenerative cervical myelopathy: a spectrum of related disorders affecting the aging spine. Neurosurgery 77(Suppl 4):S51–S67. doi:10.1227/NEU.0000000000000951
Lebl DR, Hughes A, Cammisa FP Jr, O’Leary PF (2011) Cervical spondylotic myelopathy: pathophysiology, clinical presentation, and treatment. HSS J the Musculosk J Hospit Spec Surg 7(2):170–178. doi:10.1007/s11420-011-9208-1
Lawrence BD, Jacobs WB, Norvell DC, Hermsmeyer JT, Chapman JR, Brodke DS (2013) Anterior versus posterior approach for treatment of cervical spondylotic myelopathy: a systematic review. Spine 38(22 Suppl 1):S173–S182. doi:10.1097/BRS.0b013e3182a7eaaf
Shamji MF, Massicotte EM, Traynelis VC, Norvell DC, Hermsmeyer JT, Fehlings MG (2013) Comparison of anterior surgical options for the treatment of multilevel cervical spondylotic myelopathy: a systematic review. Spine 38(22 Suppl 1):S195–S209. doi:10.1097/BRS.0b013e3182a7eb27
Cabraja M, Abbushi A, Koeppen D, Kroppenstedt S, Woiciechowsky C (2010) Comparison between anterior and posterior decompression with instrumentation for cervical spondylotic myelopathy: sagittal alignment and clinical outcome. Neurosurg Focus 28(3):E15. doi:10.3171/2010.1.FOCUS09253
Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH (1999) Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am 81(4):519–528
Kimura A, Seichi A, Inoue H, Hoshino Y (2011) Long-term results of double-door laminoplasty using hydroxyapatite spacers in patients with compressive cervical myelopathy. Eur Spine J 20(9):1560–1566. doi:10.1007/s00586-011-1724-7
Seichi A, Takeshita K, Ohishi I, Kawaguchi H, Akune T, Anamizu Y, Kitagawa T, Nakamura K (2001) Long-term results of double-door laminoplasty for cervical stenotic myelopathy. Spine 26:479–487
Kawaguchi Y, Nakano M, Yasuda T, Seki S, Hori T, Suzuki K, Makino H, Kanamori M, Kimura T (2016) More than 20 years follow-up after en bloc cervical laminoplasty. Spine 41(20):1570–1579. doi:10.1097/BRS.0000000000001579
Motosuneya T, Maruyama T, Yamada H, Tsuzuki N, Sakai H (2011) Long-term results of tension-band laminoplasty for cervical stenotic myelopathy: a 10-year follow-up. J Bone Joint Surg Br 93(1):68–72. doi:10.1302/0301-620X.93B1.24532
Burkhardt BW, Brielmaier M, Schwerdtfeger K, Sharif S, Oertel JM (2016) Smith-Robinson procedure with an autologous iliac crest graft and caspar plating: report of 65 patients with an average follow-up of 22 years. World neurosurgery 90:244–250. doi:10.1016/j.wneu.2016.02.074
Burkhardt BW, Brielmaier M, Schwerdtfeger K, Sharif S, Oertel JM (2016) Smith-Robinson procedure with an autologus iliac crest for degenerative cervical disc disease: a 28-year follow-up of 95 patients. World neurosurgery 92:371–377
Fehlings MG, Barry S, Kopjar B, Yoon ST, Arnold P, Massicotte EM, Vaccaro A, Brodke DS, Shaffrey C, Smith JS, Woodard E, Banco RJ, Chapman J, Janssen M, Bono C, Sasso R, Dekutoski M, Gokaslan ZL (2013) Anterior versus posterior surgical approaches to treat cervical spondylotic myelopathy: outcomes of the prospective multicenter AOSpine North America CSM study in 264 patients. Spine 38(26):2247–2252. doi:10.1097/BRS.0000000000000047
Yalamanchili PK, Vives MJ, Chaudhary SB (2012) Cervical spondylotic myelopathy: factors in choosing the surgical approach. Adv Orthop 2012:783762. doi:10.1155/2012/783762
Ba Z, Zhao W, Wu D, Shen B, Yu B, Wang Z (2012) Box cages packed with local decompression bone were efficient in anterior cervical discectomy and fusion: 5- to 10-year follow-up. Spine 37(20):E1260–E1263. doi:10.1097/BRS.0b013e318265df75
Maharaj MM, Phan K, Mobbs RJ (2016) Anterior cervical discectomy and fusion (ACDF) autograft versus graft substitutes: what do patients prefer?: a clinical study. J Spine Surg 2:105–110. doi:10.21037/jss.2016.05.01
Kim CH, Chung CK, Hahn S (2013) Autologous iliac bone graft with anterior plating is advantageous over the stand-alone cage for segmental lordosis in single-level cervical disc disease. Neurosurgery 72(2):257–265. doi:10.1227/NEU.0b013e31827b94d4 (discussion 266)
Zoega B, Karrholm J, Lind B (1998) Plate fixation adds stability to two-level anterior fusion in the cervical spine: a randomized study using radiostereometry. Eur Spine J 7(4):302–307
Wang JC, McDonough PW, Kanim LE, Endow KK, Delamarter RB (2001) Increased fusion rates with cervical plating for three-level anterior cervical discectomy and fusion. Spine 26(6):643–646 (discussion 646–647)
Song KJ, Lee KB, Song JH (2012) Efficacy of multilevel anterior cervical discectomy and fusion versus corpectomy and fusion for multilevel cervical spondylotic myelopathy: a minimum 5-year follow-up study. Eur Spine J 21(8):1551–1557. doi:10.1007/s00586-012-2296-x
Luo J, Cao K, Huang S, Li L, Yu T, Cao C, Zhong R, Gong M, Zhou Z, Zou X (2015) Comparison of anterior approach versus posterior approach for the treatment of multilevel cervical spondylotic myelopathy. Eur Spine J 24(8):1621–1630. doi:10.1007/s00586-015-3911-4
Zhu B, Xu Y, Liu X, Liu Z, Dang G (2013) Anterior approach versus posterior approach for the treatment of multilevel cervical spondylotic myelopathy: a systemic review and meta-analysis. Eur Spine J 22(7):1583–1593. doi:10.1007/s00586-013-2817-2
Kim JT, Lee HJ, Choi DY, Shin MH, Hong JT (2016) Sequential alignment change of the cervical spine after anterior cervical discectomy and fusion in the lower cervical spine. Eur Spine J 25(7):2223–2232. doi:10.1007/s00586-016-4401-z
Li J, Zheng Q, Guo X, Zeng X, Zou Z, Liu Y, Hao S (2013) Anterior surgical options for the treatment of cervical spondylotic myelopathy in a long-term follow-up study. Arch Orthop Trauma Surg 133(6):745–751. doi:10.1007/s00402-013-1719-4
Acknowledgements
The authors thank Gudrun Wagenpfeil at Institute for Medical Biometry, Epidemiology and Medical Informatics (IMBEI), Saarland University Faculty of Medicine for her contribution to this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
B. Burkhardt, M. Brielmaier, K. Schwerdtfeger, S. Sharif and J. Oertel have no conflict of interest.
Rights and permissions
About this article
Cite this article
Burkhardt, B.W., Brielmaier, M., Schwerdtfeger, K. et al. Smith-Robinson procedure with and without Caspar plating as a treatment for cervical spondylotic myelopathy: A 26-year follow-up of 23 patients. Eur Spine J 26, 1246–1253 (2017). https://doi.org/10.1007/s00586-017-4988-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-4988-8