Abstract
Purpose
Our study aimed to confirm the correlation between the Cranial Sagittal Vertical Axis (CrSVA) and patient-reported outcomes and to compare clinical correlation between CrSVA and C7 SVA in adult spinal deformity (ASD) patients.
Methods
108 consecutive ASD patients were evaluated using the EOS® 2D/3D radio-imaging device. A vertical plumb line from the cranial center was utilized to measure the distance to the posterior corner of S1 (CrSVA-S), and to the centers of the hip (CrSVA-H), the knee (CrSVA-K), and ankle (CrSVA-A), as well as measuring the standard C7 SVA. We analyzed the correlation between each CrSVA parameter with the Oswestry Disability Index (ODI) and Scoliosis Research Society form (SRS-22r).
Results
All 4 CrSVA measures demonstrated strong correlation with the ODI and SRS-22r total score and the pain, self-image, and function subscores. Of note, CrSVA-A (Global SVA) also strongly correlated with the SRS satisfaction subscore. Univariate linear regression showed similar results. The strongest predictor of outcomes was CrSVA, not C7 SVA; (CrSVA-H for ODI, SRS total score, and the pain, self-image, and function subscores; and Global SVA for satisfaction and mental health subscores).
Conclusions
The clinical correlation effect of outcome scores to the CrSVA measures is validated. Global SVA has an especially strong correlation with ODI and all the SRS subscores. Our study confirms that CrSVA is a stronger predictor of preoperative clinical outcomes than the C7 SVA in adult deformity patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Unlike the younger or adolescent patients with a spinal deformity, the older adult presents with a completely different set of problems and challenges to the treating physician. Low back pain and stiffness are the two most common clinical symptoms in adult spinal deformity (ASD) patients [1, 2]. In addition, numbness and cramping in the legs and neurogenic claudication due to lumbar spinal stenosis and radiculopathy can occur [3]. Spinal stiffness among other clinical findings can cause spinal sagittal imbalance. Loss of spinal sagittal balance causes patients to compensate with hyperlordosis of the cervical spine, posterior tilt of the head, pelvic retroversion, extension of the hip joints, flexion of the knee joints, and dorsiflexion of the ankle joints to try and maintain an upright posture [4–7]. Therefore, the comprehensive effect of ASD on the patient-reported outcomes has been difficult to predict based on the degree of spinal deformity alone [8–10].
Some prior studies have attempted to correlate radiographic appearance and clinical symptoms. Emami et al. [11] demonstrated that patients with positive sagittal imbalance after long fusions to the sacrum had increased pain compared with patients with negative sagittal balance. Glassman et al. [1] reported that using the C7 sagittal vertical axis (SVA) to assess balance is the most important and reliable radiographic predictor of clinical health status, as patients with positive sagittal imbalance reported worse self-assessment in SRS 22 pain, function, and self-image subscores. Consistently, several studies have already demonstrated that the improvement in sagittal balance using the C7 SVA is the strongest predictor of improved outcomes in patients with adult spinal deformity [10, 12–14]. On the other hand, a more recent study reported that an increased pelvic tilt (PT) was significantly associated with the worse results in all SRS 22 subscores. The C7 SVA was not significantly correlated with the SRS 22 subscores and their multivariate analysis demonstrated that PT was the best predictor of the function subscore [15]. Given this report, the C7 SVA may not be the best radiographic parameter for clinical prediction in adult spinal deformity. In addition, some clinical findings may have as much importance as the spinal sagittal profile in ASD. Optimal total body sagittal alignment (TBSA), from the head to the ankle joint of the human body, may be required to keep an energy-efficient erect position and horizontal gaze for ultimate clinical satisfaction. We began to evaluate TBSA using a plumbline from the cranial center of mass (CCOM), or the cranial (Cr) SVA. Our study aimed to confirm the correlation between the CrSVA and patient-reported outcomes and to compare the clinical correlation between the CrSVA and C7 SVA in ASD patients.
Materials and methods
We hypothesized that the CrSVA would predict health-related quality-of-life (HRQOL) outcomes in ASD better than the C7 SVA. After institutional review board approval, a retrospective radiographic and clinical analysis of 108 consecutive patients who underwent surgical correction for ASD (88 women/20 men; mean age at surgery, 50.5 ± 16.4 years, range 22–74) by a single surgeon was performed. X-rays were obtained with the EOS® 2D/3D radio-imaging device (Biospace Med, France) between 2010 and 2012 at a single institution. Patients were instructed to stand naturally with a horizontal gaze and their fingertips resting comfortably on the ipsilateral clavicle. Data were collected and analyzed by an independent senior spine surgeon not involved in the surgical treatment. The diagnoses were adult idiopathic scoliosis (n = 30 patients, 28 %), degenerative lumbar kyphoscoliosis (n = 29 patients, 27 %), fixed sagittal imbalance due to the previous surgery (n = 40 patients, 37 %), and Scheuermann’s kyphosis (n = 9 patients, 8 %). The demographic and diagnosis data are further illustrated in Table 1.
Radiographic parameters
The four TBSA distance parameters measured from the CrSVA and three commonly accepted sagittal parameters (the C7 SVA, lumbar lordosis, (LL), and PT) which are significantly associated with clinical outcomes were measured on preoperative full-body sagittal radiographs for all patients. All measurements were made by a single attending spine surgeon using the digital measuring capabilities of a picture archiving and communication system (PACS).
The four TBSA distance parameters were based on five anatomic landmarks (Fig. 1): the cranial center of mass (CCOM), the posterior, superior corner of the sacrum, and the centers of the hips, knees, and ankles. The CCOM was defined as the midpoint of the nasion-inion line (root of the nose to the external occipital protuberance), above and slightly in front of the external auditory meatus [16, 17]. The posterior superior corner of the S1 endplate defined the lumbosacral pivot point. The center of the hips was defined as the midpoint of the line drawn through the center of the two femoral heads. Similarly, the center of the knees was the midpoint of the line connecting the center of the two tibial plateaus on the lateral view, and the center of the ankles was the midpoint of the line connecting the apices of the talar domes [18, 19]. The four TBSA distance relationships were generated relative to a plumb line from the CCOM, which we referred to as the cranial sagittal vertebral axis (CrSVA): to the sacrum (CrSVA-S); to the hip center (CrSVA-H); to the knee center (CrSVA-K); and to the ankle center (CrSVA-A). This final term, CrSVA-A, represented global sagittal balance (Fig. 2).
In addition, the C7 SVA was measured as the distance from the C7 plumbline to the perpendicular line drawn from the superior posterior endplate of the S1 vertebral body. The Cobb method [20] was used for the currently accepted sagittal radiographic parameters, and PT and pelvic incidence (PI) were measured as per standard techniques.
Patient-reported outcomes
Preoperatively, all the patients completed the Oswestry Disability Index (ODI) [21] and Scoliosis Research Society form (SRS-22) [22].
Statistical correlation between radiographic parameters and patient-reported outcomes
Data were summarized by mean ± SD for numeric variables. The Pearson’s correlation coefficients were estimated to investigate the association between predictors and response variables. The effect of independent variables on response variables was analyzed using the univariate and multivariate linear regressions, and the statistically significant variables were selected in a stepwise manner with 0.05 alpha level. To check the multicollinearity problem, the variance inflation factor (VIF) was also estimated. The VIF quantifies the severity of multicollinearity in regression analysis, and a VIF less than 10 indicates that there was no problematic multicollinearity among the independent variables (VIF <10) [23].
All statistical analyses were performed using the SPSS 21.0 version and p values less than 0.05 were considered significant.
Results
Value of radiographic parameters and patient-reported outcomes
The mean C7 SVA was 5.9 ± 7.8 cm; while the mean CrSVA measures were as follows: CrSVA-S, 7.8 ± 8.5 cm; CrSVA-H, 2.4 ± 7.3 cm; and CrSVA-K, 2.9 ± 5.0 cm; and the mean CrSVA-A was 5.0 ± 5.6 cm. The mean ODI for the patients in this study was 44.5 ± 18.4. For the SRS 22, the mean domain scores were: pain, 2.2 ± 0.9; self-image, 2.5 ± 0.7; function, 3.1 ± 0.9; satisfaction, 2.9 ± 0.9; and mental health, 3.6 ± 0.8. The mean total SRS score was 2.9 ± 0.6 (Table 2).
Correlations between radiographic parameters and patient-reported outcomes
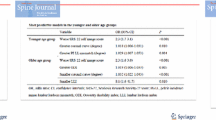
Results from the Pearson correlation analysis between radiographic parameters and HRQOL (Table 3) revealed that the C7 SVA significantly correlated with the ODI (r = 0.510), SRS total score (r = −0.316), pain (r = −0.416), and function subscores (r = −0.514), but was not significantly correlated with SRS self-image, satisfaction, and mental health subscores. The CrSVA-S, -H, -K, and -A measures demonstrated a significant correlation with the ODI (r = 0.331–0.514), SRS total score (r = −0.382 to −0.499), pain (r = −0.331 to −0.441), self-image (r = −0.290 to −0.363), function (r = −0.299 to −0.550), satisfaction (r = −0.215 to −0.429), and mental health subscores (r = −0.229 to −0.249). However, the four CrSVA measures, although statistically significant, showed weaker correlation with SRS satisfaction and mental health subscores than with other SRS scores and ODI. Of note, only the CrSVA-A (Global SVA) demonstrated a relatively strong correlation with the SRS satisfaction subscore (r = −0.429) (Table 3).
Univariate analysis showed the similar results for the effect of the C7 SVA and CrSVA-S, -H, -K, and -A measures on ODI and SRS subscores using the Pearson correlation coefficient (Table 4).
Multivariate analysis on radiographic parameters for patient-reported outcomes
A multiple linear regression was performed, in which each ODI and SRS 22 score were the dependent variables, and age, sex, LL, PT, C7 SVA, CrSVA-S, -H, -K, and -A measures were independent variables to evaluate the combined effect of these independent variables. Multivariate analysis showed that the strongest radiographic predictor for ODI and all SRS subscores was CrSVA, not C7 SVA; (CrSVA-H for ODI (β = 1.292; P < 0.001), SRS total score (β = −0.044; P < 0.001), pain (β = −0.052; P < 0.001), self-image (β = −0.036; P < 0.001), and function subscores (β = −0.061; P < 0.001); and the CrSVA-A for the SRS satisfaction (β = −0.046; P < 0.001) and mental health subscores (β = −0.023; P = 0.018) (Table 5).
Discussion
The biomechanical function of the spine is to cranially support the weight of the head and to caudally transfer the body’s weight to the lower extremities connecting through the pelvis. In addition, it provides both structural support and balance to maintain an upright posture and provides forward visual gaze as well as functional range of motion to the trunk [24, 25]. Therefore, total body sagittal alignment, including the head to the ankles, may certainly have an important effect on patient-reported outcomes of adult spinal deformity patients. The C7 SVA radiographic evaluation is limited to the spinal column alone (plumbline of the 7th cervical vertebra to the sacrum) and is not sufficient in evaluating global spinal balance, as it does not consider the cervical spine [26–28]. Thus, it may have shortcomings in accounting for patient-reported outcomes from a global body alignment perspective. Actually, we often anecdotally experienced that some patients showed relatively poor improvement of clinical scores, despite the improvement in spinal sagittal balance evaluation using the C7 SVA after surgical correction for ASD. Spine surgeons have recently evaluated the postoperative results using radiographic parameters limited to the spine-pelvic area [10–15] which does not consider the role of the linear chain of total body sagittal alignment from the skull to the ankle joint which appears to influence patient-reported outcomes.
According to our current study on preoperative ASD patients, Pearson correlation and univariate analysis confirmed that the CrSVA is significantly associated with the ODI and all SRS subscores, whereas the C7 SVA is significantly associated with the ODI and only three of the SRS subscores (pain, function, and total score). Interestingly, the CrSVA-K showed relatively weaker correlation with the ODI and all the SRS subscores versus the other three CrSVA measures. We think that this finding reinforces that the knee joint is a relatively dynamic component in the lower extremity linear chain of TBSA between the hip and ankle joints. We also postulate that this result is likely due to the fact that the ankle joints are fixed on the ground and the hip joints are relatively fixed in the pelvis.
One more very interesting finding was that only the CrSVA-A (Global SVA) linking the head to the ankle joint showed strong correlation with the SRS satisfaction subscore. We suggest that the CrSVA-A is needed as a radiographic parameter to predict the widest range of patient-reported outcomes.
There are weaknesses to our study. The first is the homogeneity of the patient population with a single surgeon at one academic institution. The geographic or ethnic applicability can be a concern. Further multicenter studies are needed.
Multivariate analysis of the C7 SVA and CrSVA for ODI and all SRS subscores demonstrated that the C7 SVA is no longer the best radiographic parameter to predict clinical outcomes in ASD. The CrSVA-H was the strongest radiographic predictor for the ODI, SRS total score, and the pain, self-image, and function subscores. Given this result, the relationship between the head and the hip joints is important for predicting clinical outcomes in ASD. We also realized that using just one radiographic parameter might not be enough to fully encompass clinical outcomes. Therefore, we propose use of these objective TBSA indices as well as grouping them with other established radiographic parameters to best predict clinical outcomes in ASD patients. Moreover, this result reinforces that ASD patients can do well despite having a high C7 SVA, PT, and PI-LL mismatch and somewhat low LL as long as their CrSVA-A (Global SVA) or CrSVA-H are near 0 cm (Fig. 3).
a 60-year-old female was seen with sagittal imbalance due to degenerative lumbar kyphoscoliosis. Sagittal radiographic parameters were low LL of −13°, high PT of 25°, PI-LL mismatch of 39°, C7 SVA of 14 cm, CrSVA-H of 5.3 cm, and CrSVA-A (Global SVA) of 12 cm. Health-related quality-of-life scores showed a high ODI and low SRS subscores in all domains. b 66-year-old female was seen with sagittal imbalance due to degenerative lumbar kyphoscoliosis. Sagittal radiographic parameters were low LL of −22°, high PT of 29°, PI-LL mismatch of 33°, C7 SVA of 7.2 cm, CrSVA-H of 0.6 cm, and CrSVA-A (Global SVA) of 0.8 cm. Although she had regional imbalance from C7 to her sacrum, her clinical scores and function were better than the prior patient, because her overall global balance was good
Conclusion
The clinical correlation on outcome scores of CrSVA measures is validated for preoperative ASD patients. Global SVA has an especially strong correlation with ODI and all the SRS subscores. Our study confirms that CrSVA is a stronger predictor of clinical outcomes than the C7 SVA and should be considered as a standard measure for the analysis of adult spinal deformity patients.
References
Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR (2005) Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine 30(6):682–688
Birknes JK, White AP, Albert TJ, Shaffrey CI et al (2008) Adult degenerative scoliosis: a review. Neurosurgery 63:94–103
Sengupta K (2012) Adult spinal deformity. In: Rao RD, Smuck M (eds) Orthopaedic knowledge update: spine, 4th edn. American Academy of Orthopaedic Surgeons, Rosemont, pp 349–367
Lafage V, Schwab F, Patel A et al (2009) Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine 34:E599–E606
Lazennec JY, Ramare S, Arafati N et al (2000) Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J 9:47–55
Yoshimoto H, Sato S, Masuda T et al (2005) Spinopelvic alignment in patients with osteoarthrosis of the hip: a radiographic comparison to patients with low back pain. Spine 30:1650–1657
Lamartina C, Berjano P (2014) Classification of sagittal imbalance based on spinal alignment and compensatory mechanisms. Eur Spine J 23:1177–1189
D’Andrea LP, Betz RR, Lenke LG, Clements DH, Lowe TG, Merola A et al (2000) Do radiographic parameters correlate with clinical outcomes in adolescent idiopathic scoliosis. Spine 25(14):1795–1802
Deviren V, Berven S, Kleinstueck F, Antinnes J, Smith JA, Hu SS (2002) Predictors of flexibility and pain patterns in thoracolumbar and lumbar idiopathic scoliosis. Spine 27(21):2346–2349
Schwab FJ, Smith VA, Biserni M, Gamez L, Farcy JP, Pagala M (2002) Adult scoliosis: a quantitative radiographic and clinical analysis. Spine 27:387–392
Emami A, Deviren V, Berven S, Smith JA, Hu SS, Bradford DS (2002) Outcome and complications of long fusions to the sacrum in adult spine deformity: luque-galveston, combined iliac and sacral screws, and sacral fixation. Spine 27(7):776–786
Mac-Thiong JM, Transfeldt EE, Mehbod AA, Perra JH, Denis F, Garvey TA et al (2009) Can C7 plumbline and gravity line predict health related quality of life in adult scoliosis? Spine 34(15):E519–E527
Daubs MD, Lenke LG, Bridwell KH, Kim YJ, Hung M, Cheh G et al (2013) Does correction of preoperative coronal imbalance make a difference in outcomes of adult patients with deformity? Spine 38(6):476–483
Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F (2005) The impact of positive sagittal balance in adult spinal deformity. Spine 30(18):2024–2029
Sánchez-Mariscal F, Gomez-Rice A, Izquierdo E, Pizones J, Zúñiga L, Alvarez-González P (2012) Correlation of radiographic and functional measurements in patients who underwent primary scoliosis surgery in adult age. Spine 37(7):592–598
Vital JM, Senegas J (1986) Anatomical bases of the study of the constraints to which the cervical spine is subject in the sagittal plane: a study of the center of gravity of head. SurgRadiolAnat 8:169–173
Yoganandan N, Pintar FA, Zhang J et al (2009) Physical properties of the human head: mass, center of gravity and moment of inertia. J Biomech 42:1177–1192
Lazennec JY, Brusson A, Rousseau MA (2013) Lumbar-pelvic-femoral balance on sitting and standing lateral radiographs. Orthop Traumatol Surg Res 99S:S87–S103
Matsumoto T, Kubo S, Muratsu H et al (2011) Differing prosthetic alignment and femoral component sizing between 2 computer-assisted CT-free navigation systems in TKA. Orthopedics 34:e860–e865
Cobb JR (1948) Outline for the study of scoliosis. Instructional course lectures. Am Acad Orthop Surg 5:261–275
Fairbank JC, Pynsent PB (2000) The Oswestry disability index. Spine 25:2940–2952
Haher TR, Gorup JM, Shin TM et al (1999) Results of the Scoliosis Research Society instrument for evaluation of surgical outcome in adolescent idiopathic scoliosis: a multicenter study of 244 patients. Spine 24:1435–1440
Hair JF, Anderson R, Tatham RL et al (2006) Multivariate data analysis. Prentice Hall, Upper Saddle River
Haher TR, O’Brien M, Kauffman D et al (1993) Biomechanics of the spine in sports. Clin Sports Med 12:449–464
Guillot M, Fournier J, Vanneuville G et al (1988) Mechanics of the characteristic geometry of the human spine undergoing vertical pressure. Revue du Rhumatismeet des Maladies. Osteo Articul 55:351–359
Cecchinato R, Langella F, Bassani R, Sansone V, Lamartina C, Berjano P (2014) Variations of cervical lordosis and head alignment after pedicle subtraction osteotomy surgery for sagittal imbalance. Eur Spine J 6:644–649
Obeid I, Boniello A, Boissiere L et al (2015) Cervical spine alignment following lumbar pedicle subtraction osteotomy for sagittal imbalance. Eur Spine J 24:1191–1198
Protopsaltis TS, Scheer JK, Terran JS et al (2015) How the neck affects the back: changes in regional cervical sagittal alignment correlate to HRQOL improvement in adult thoracolumbar deformity patients at 2-year follow-up. J Neurosurg Spine 23:153–158
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
The authors certify that they have no affiliations with or financial involvement in any organization or entity with a direct financial interest in the subject matter discussed in the manuscript. There was no company or organization that sponsored or influenced this study in any way. No monies were received for this research.
Additional information
IRB Approval Statement: This study was approved by the Institutional Review Board (IRB).
All surgeries and research for this study were performed at the Department of Orthopedic Surgery, Washington University School of Medicine in St. Louis, MO.
Rights and permissions
About this article
Cite this article
Kim, YC., Lenke, L.G., Lee, SJ. et al. The cranial sagittal vertical axis (CrSVA) is a better radiographic measure to predict clinical outcomes in adult spinal deformity surgery than the C7 SVA: a monocentric study. Eur Spine J 26, 2167–2175 (2017). https://doi.org/10.1007/s00586-016-4757-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4757-0