Abstract
Purpose
The aim of this study is to determine the correlation between photographic sagittal parameters and patient-reported outcome measures (PROM) results in adult patients operated on spinal deformity.
Methods
Non-concurrent prospective study. Inclusion criteria: age at surgery older than 25, minimum 2-year follow-up after a 5 or more level fusion for adult spinal deformity (ASD). Full body lateral standing photographs were taken with adhesive markers placed on ten bony landmarks. SRS-22 and SF-36 questionnaires were completed for every patient. The following photographic parameters were measured: lumbar angle, lumbar curve, thoracic inclination (TI), trunk angle, pelvic tilt, head angle, neck angle, cervicothoracic angle, lumbar vector angle (LVA), dorsal vector angle (DVA), cervical vector angle (CVA), cranial pelvic angle (CrPA), cranial sacral angle (CrSA), fibular inclination angle (FIA) and cranial sagittal vertical axis measured to sacrum (Cr-S), greater trochanter (Cr-GT), knee (Cr-K) and ankle (Cr-A).
Results
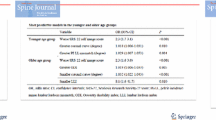
65 patients (58 female) operated on ASD in a single institution were included. Age at surgery was 61 years (26–67). Postoperative follow-up was 53 months (24–120). Spearman rank order test showed several significant (p ≤ 0.01) correlations. After multivariate linear regression analysis age, LVA and TI remained as predictors for SRS image scores (corrected r2 0.41), LVA for SRS satisfaction (corrected r2 0.27), CrPA and age for SRS total scores (corrected r2 0.33), FIA and age for SF36 physical functioning (corrected r2 0.36) and CrSA for SF36 role physical (corrected r2 0.14).
Conclusions
Some sagittal photographic parameters may predict mid-term clinical results after ASD surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several bony prominences have been suggested to serve as anatomical landmarks that may be used for analysis of human posture [1]. Surgimap software (Nemaris Inc., New York, NY, USA) has been proven to have excellent inter-rater and intra-rater reliabilities for measuring spinal postural angles from digital photographs [2].
To the best of our knowledge, no previous study has addressed photographic sagittal plane analysis in adult spinal deformity patients. Multiple studies have demonstrated a correlation between radiographic sagittal parameters and clinical results in adult spinal deformity (ASD) patients [3,4,5,6]. Considering this, the purpose of this study is to determine the correlation between photographic sagittal parameters [7] and Patient-Reported Outcome Measures (PROM) results in adult patients operated on spinal deformity.
Methods
Study design
This is a single-center single-surgeon non-concurrent prospective study approved by the Institutional Research Ethics Committee. Written informed consent was obtained from all patients after they were provided with a detailed information sheet.
Hypothesis: photographic sagittal parameters measured in full body clinical photographs may predict mid-term PROM results in patients operated on for adult deformity.
Subject inclusion
Inclusion criteria were as follows: age at surgery older than 25 years, minimum 2-year follow-up after surgery and having undergone a five or more levels fusion for idiopathic or degenerative scoliosis with main Cobb angle greater than 30°, sagittal and/or coronal imbalance greater than 5 cm, T3–T12 kyphosis greater than 80° or thoracolumbar kyphosis greater than 20°.
Exclusion criteria: tumors, neuromuscular, congenital or traumatic deformity.
Out of 130 patients operated on for adult deformity between January 2007 and December 2016, 80 met our inclusion criteria. Three patients were deceased, two patients could not be contacted and nine patients lived far away and could not participate due to logistic reasons. One patient refused to participate in our study.
Sixty-five patients were finally included. Patient’s characteristics and type of surgery [8] are summarized in Table 1.
Data collection
Data were collected by two researchers not involved in patient treatment.
Informed consent granting permission to use the photographs for this study was obtained from all individual participants included in the study. Subjects completed SRS-22 and SF36 questionnaires and full body lateral standing photographs were taken by a professional clinical photographer in a single clinical visit. Final follow-up full spine lateral radiographs were available for all 65 patients.
All photographs were taken by the same professional clinical photographer using similar camera settings and lighting, in the same room and at the same distance. To obtain results comparable to those obtained with radiographic sagittal plane analysis photographs were taken in freestanding posture with fingers on the clavicles and shoulders in 40° of forward elevation [9].
Surface anatomical landmarks
25-mm diameter spheres and 35-mm base diameter cones were used as skin markers.
Marker placement was based on previous research. Ten adhesive skin markers were attached on the following bony landmarks: the spinous process of C7 [10, 11], T1 [12], T12 [10, 13], L3 [10, 12] and S1 [13], lateral malleolus [10, 14, 15], fibular head [10, 14], greater trochanter [10, 14, 15], anterior superior iliac spine [10, 14, 15] and ear tragus [15, 16].
Photographic sagittal parameters
Photographic measures were obtained by a single unbiased trained observer with image analysis software (Surgimap, Nemaris Inc., New York, NY, USA).
The following previously described [2, 7, 13, 17] photographic sagittal parameters (Fig. 1) were measured:
-
1.
Lumbar curve (LC): angle between the line joining the center of the base of the cones marking S1 and L3 and the line joining the center of the base of the cones marking L3 and D12 (Fig. 1a).
-
2.
Lumbar angle (LA): angle between the line joining the center of the base of the T12 marker with the anterosuperior iliac spine (ASIS) marker and the line joining ASIS with the greater trochanter (GT) marker (Fig. 1b).
-
3.
Thoracic inclination (TI): angle between a vertical line extending upward from the T12 marker and a line joining T12–C7 (Fig. 1c).
-
4.
Pelvic tilt (PT): angle between a vertical line extending upward from the GT and a line joining GT-ASIS (Fig. 1d).
-
5.
Head angle (HA): the angle between the line joining the tragus and the canthus (out slit in the eyelid), and the vertical (Fig. 1e).
-
6.
Neck angle (NA): the angle between a line joining C7 to the tragus, and the vertical (Fig. 1f).
-
7.
Trunk angle (TA): angle between the lines joining C7–T12 and T12–GT (Fig. 1g).
-
8.
Cervicothoracic angle (CTA): the angle between a line joining the tragus to C7 and a line joining C7–T12 (Fig. 1h).
-
9.
Lumbar vector angle (LVA): the angle between two vectors created using the lines joining the vertex with the Center of the base of the cones marking T12 and S1 (Fig. 1i).
-
10.
Cervical vector angle (CVA): angle between the T1 vector and the line perpendicular to a line from the forehead to the chin [13, 19] passing through the center of the forehead (Fig. 1j).
-
11.
Dorsal vector angle (DVA), the angle between two vectors created using the lines joining the vertex with the center of the base of the cones marking T12 and T1 (Fig. 1k).
Four total body sagittal alignment distance parameters were generated relative to a plumb line from the tragus (cranial center of mass) [18, 20] to four different skin markers (Fig. 2):
-
1.
Cranial Sagittal vertical axis to sacrum (Cr-S)
-
2.
Cranial Sagittal vertical axis to the greater trochanter (Cr-GT)
-
3.
Cranial Sagittal vertical axis to the fibular head (Cr-Knee)
-
4.
Cranial Sagittal vertical axis to the external malleolus (Cr-Ankle)
Two newly global alignment angles were described:
-
1.
Cranial pelvic angle (CrPA) (Fig. 3a) is defined by the angle between a line from the center of the greater trochanter to the base of the S1 marker and a line joining the center of the greater trochanter marker to the cranial center of mass (CCM).
-
2.
Cranial sacral angle (CrSA) (Fig. 3b). This is the angle between a line from the center of the base of the S1 marker to the CCM and a line from the center of the base of the S1 marker to the center of the greater trochanter marker.
A new parameter, the fibular inclination angle (Fig. 4) (FIA) was measured to account for distal lower limb compensation. During mechanical compensation, the knees are flexed, ankles are extended and the fibulas become oblique [21, 22] on a full-body lateral photograph. The FIA corresponds to the angle between the lines joining the center of the fibular head marker with the lateral malleolus and the vertical.
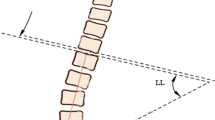
Radiographic parameters
Five commonly accepted [3,4,5,6] sagittal parameters were measured using Surgimap software (Nemaris Inc., New York, NY, USA): lumbar lordosis (LL), pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS) and C7-Sagittal Vertical Axis (SVA). Two global alignment angular parameters, the spinopelvic angle (SPA) and the T1 pelvic tilt (TPA) were measured to determine their association with the CrPA and the CrSA.
Statistical analysis
The collected data were analyzed using IBM SPSS Statistics 23 for Windows. Descriptive statistics are presented as median and interquartile range (IQR) (25–75%).
Spearman's correlation coefficient was used to evaluate the correlation between quantitative variables. To account for multiple comparisons p values less than or equal to 0.01 were considered statistically significant in the bivariate analysis, whilst in multivariate analysis p values less than 0.05 were considered statistically significant. For the variables in which a significant (p < 0.01) correlation was detected between photographic sagittal parameters and PROM scores a multivariate linear regression was carried out. Each model included as a dependent variable a PROM domain and the photographic parameters as the independent variables. Age was included in the multivariate analysis when it showed highly significant correlation (p < 0.01) with PROM domains. The models were developed with the use of the forward selection procedure with F probability entry criteria set as 0.05. The assumption of homocedasticity was tested with scatter plots. Multicollinearity was assessed using the tolerance and variance inflation factor (VIF) statistics.
Results
Radiographic sagittal parameters, SRS-22 and SF-36 questionnaires
Radiographic sagittal parameters and HRQOL results are shown in Table 2.
Correlations between the two novel photographic global alignment angular parameters and radiographic global alignment angular parameters
The CrPA was highly correlated with the TPA (r = 0.88; p = 0.000). The CrSA showed a highly significant correlation with the SPA (r = 0.71; p = 0.000).
Correlations between photographic sagittal parameters and patient-reported outcomes
Table 3 summarizes the sagittal photographic parameters measured in full body photographs. Many correlations found between photographic parameters and PROM results (Tables 4, 5) were significant (p < 0.05), although most were not very strong (r < 0.5). To adjust to the high probability of finding significant values by chance when performing multiple comparisons only highly significant correlations (p < 0.01; r > 0.25) were acknowledged.
Age significantly correlated with SRS image (r − 0.36; p 0.008), SRS total score (r − 0.40; p 0.003), SRS pain (r − 0.38; p 0.004) and SF-36 physical functioning (r − 0.39; p 0.004). TI showed a significant correlation with SRS image (r − 0.45; p 0.009), SRS satisfaction (r − 0.37; p 0.007), SRS total (r − 0.33; p 0.009), SF36 physical functioning (r − 0.34; p 0.008), and SF-36 role physical (r − 0.36; p 0.005). LVA demonstrated a significant correlation with SRS image (r 0.42; p 0.001), SRS satisfaction (r 0.44; p 0.001), SRS total (r 0.38; p 0.003), SF36 physical functioning (r 0.35; p 0.008), and SF-36 role physical (r 0.37; p 0.005). Cr-GT showed correlation with SRS image (r − 0.37; p 0.004), SRS satisfaction (r − 0.36; p 0.009), SF36 physical functioning (r − 0.40; p 0.002) and SF-36 role physical (r − 0.39; p 0.003). CrPA was correlated with SRS satisfaction (r − 0.44; p 0.000), SRS total (r − 0.34; p 0.007) and SF36 bodily pain (r − 0.34; p 0.008). CrSA showed a significant correlation with SF36 role physical (r 0.33; p 0.01). The FIA was significantly correlated with SRS pain (r − 0.36; p 0.004) and SF36 physical functioning (r − 0.41; p 0.001).
Multivariate analysis on photographic parameters for patient-reported outcomes
A multiple linear regression was performed to determine the variability in patient-reported outcomes attributable to the variables that showed a highly significant (p < 0.01) correlation with PROM results in the Spearman rank-order test.
Maximum models are presented in Table 6.
After multivariate linear regression analysis age, LVA and IT remained as predictors for SRS image scores (corrected r2 0.41), LVA for SRS satisfaction (corrected r2 0.27), CrPA and age for SRS total scores (corrected r2 0.33), FIA and age for SF36 physical functioning (corrected r2 0.36) and CrSA for SF36 role physical (corrected r2 0.14). The final modeling results are summarized in Table 7.
The results confirm our hypothesis that some photographic sagittal parameters may predict mid-term clinical results of adult spinal deformity surgery.
Discussion
Patients with adult spinal deformity receive multiple radiographs over time to track deformity progression and surgical results [23]. Considering the risks associated with radiation exposure from repeated radiographs, there is an increasing need for a less invasive assessment to monitor spinal alignment [24].
Recent efforts in this direction have been made with the development of modern systems of surface topography [25]. However, given the high cost of the equipment, its use in both clinical practice and research is limited.
Digital photography has been successfully used as a tool for postural assessment in children with scoliosis [26]. To the best of our knowledge, this pilot study is the first aiming to standardize photographic postural assessment in adult spinal deformity patients.
Bony landmarks and photographic variables used in our study were selected based on previous research [1, 2, 7, 10, 12, 14,15,16,17] performed on healthy volunteers. However, some modifications were introduced to improve the method. Firstly, our patients were asked to stand with fingers on the clavicles and shoulders in 40° of forward elevation instead of with the arms extended and hands on either side. Arm positioning has previously been reported to have an effect on the sagittal spinal alignment [9, 21] and our study aimed to obtain reproducible results comparable to those obtained in conventional X-rays. Secondly, while most previous studies use only spheres as surface markers [1, 7, 10, 12, 14, 15] with the use of adhesive cones we were also able to calculate vector angles [13]. Thirdly, several new parameters needed to be defined. Static global balance of a patient cannot be evaluated properly without assessing all the elements of the chain of balance advocated by Dubousset [27] (lower limbs, cervical spine and head). Bearing this in mind, six new photographic sagittal parameters (Cr-S, Cr-GT, Cr-Knee, Cr-Ankle, CrSA and CrPA) were developed for global balance analysis while one parameter (FIA) was created for lower limb compensation assessment.
The four linear parameters (Cr-S, Cr-GT, Cr-Knee, Cr-Ankle) were defined relative to a plumb line from the cranial centre of mass instead of C7 considering recent findings by Kim et al. [20].
The two angular parameters, CrSA and CrPA, were described aiming to combine information of pelvic tilt and spinal inclination. They were developed to be the photographic equivalents of radiographic Spino-pelvic angle (SPA) [28] and T1 Pelvic Angle (TPA) [29] but trying to avoid their main drawbacks, that is, not including the head and cervical spine [21]. These two new photographic parameters—CrSA and CrPA—showed a highly significant correlation with SPA and TPA, but we must keep in mind that photographic global alignment parameters are expected to be more sensitive to positional changes than their radiographic counterparts.
With the advent of full-body stereoradiography, several radiographic parameters have been described for assessing lower extremities compensatory mechanisms [22]. One of the most commonly used radiographic parameters in the evaluation of lower limb compensation in adult spinal deformity is the femoral obliquity angle [21, 30]. Since no reliable surface anatomical landmark [1] has been identified for the femoral head, defining the mechanical axis of the femur in a lateral photograph seemed a challenging task. Thus, instead of the femoral obliquity our study evaluated the fibular inclination to account for ankle dorsiflexion and knee flexion.
Recent studies have found that normative values for PROM scores vary with age [31, 32]. Hence, we decided to include age in the analysis to account for this effect. Our results suggested that age was associated with poorer clinical results, which is consistent with previously reported studies [33].
Lumbar vector angle was positively correlated with SRS image, SRS satisfaction, SRS total, SF36 physical functioning and SF-36 role physical in the bivariate analysis. In multivariate analysis, it remained a significant predictor of better results in SRS Satisfaction and SRS image. LVA can be considered as an indirect measure of lumbar lordosis. Our results were in agreement with published data reporting a loss of lordosis [3,4,5,6] as a factor that may contribute to suboptimal clinical results in ASD.
TPA has been shown to be one of the best predictors of clinical outcome following adult deformity surgery [34]. It combines information of pelvic tilt and thoracic inclination [29]. Bearing this in mind, it is no surprise that patients with higher TI values reported worst outcomes and that this association persisted after multivariate regression. However, we must keep in mind that the mean age of our patients was 61 years. Given the high incidence of proximal functional kyphosis (PJK) in this age group and its possible clinical implications [35], the relationship between TI and PROM scores could also be attributed to the development of PJK after ASD surgery in patients in which the upper instrumented level at or below T10.
In the non-parametric correlation analysis, patients with higher values for FIA had significantly worse SRS pain and SF36 physical functioning scores. This association with SF36 physical functioning scores was confirmed after multivariate regression analysis. No association was found between FIA and SRS scores after multivariate analysis. This could be interpreted in the light of previous studies showing that patients showing lower limb compensatory mechanisms develop leg symptoms related to spinal sagittal malalignment [36]. General health-related quality of life questionnaires, like the SF36, sometimes uncover unexpected effects that may not be detected by a disease-specific questionnaire like the SRS22. The SF-36 Physical Functioning domain asks respondents to report limitations on several mobility activities [32], such as walking specified distances, carrying groceries, climbing several flights of stairs and bathing or dressing. It is not farfetched to consider, as our results suggested, that SF-36 could be a better tool than the SRS-22 questionnaire to assess leg symptoms related to spinal sagittal malalignment.
Spearman rank order correlation showed that out of the four total body photographic sagittal alignment distance parameters evaluated only Cr-GT associated with clinical outcomes. Cr-GT showed significant correlation (p < 0.01, r > 0.25) with SRS image, SRS satisfaction, SF36 physical functioning and SF-36 role physical. No previous research has evaluated the clinical significance of Cr-GT. However, our results could be interpreted in the context of previous findings by Kim et al. [20]. Their study defines the cranial sagittal vertical axis to the center of the hips (Cr-SVA-H) as the best predictor of PROM results. Cr-SVA-H could be considered as the radiographic equivalent of Cr-GT although this should be confirmed in further studies using full-body stereoradiography.
Although C7-Sagittal vertical axis (SVA) is the most commonly used radiographic parameter for evaluating global sagittal alignment [21, 34], it has two limitations in its applicability. Firstly, the pelvis has a larger anteroposterior diameter in high pelvic incidences and SVA does not take into account the value of pelvic incidence. This induces considerable interpretation bias, particularly in high pelvic incidences. Thus, SVA should be used mainly to compare the balance situation of a patient over time or before and after surgical treatment. Secondly, the SVA radiographic evaluation is limited to the spinal column alone, as it does not consider the cervical spine [20, 21]. These to limitations of the SVA could be overcome by the use of the Cr-GT, which could be a more useful parameter to compare the results of a series of patients.
The Spearman's rank correlation suggested a positive correlation of CrSA with SF36 role physical domain and a negative correlation of CrPA with SRS satisfaction, SRS total and SF36 bodily pain.
These results suggest that patients with higher CrPA have worse PROM results, similarly as it happens with patients with higher values of radiographic TPA [29].
On the other hand patients with greater CrSA showed better clinical results after surgery for ASD, just as happens with patients with greater SPA [37] or higher spino sacral angle [37, 38] values.
Nevertheless, we must take into account that the CrPA—unlike the SSA [21]—is a postural angle, not a fixed parameter. The main drawback of using photographic global alignment parameters is that they are more likely to be affected by patient positioning than their radiographic counterparts [39].
While CrSA and CrPA remained as predictors of clinical results after multivariate analysis, the relationship between Cr-GT and PROM results was not significant after multivariate analysis. This seems to suggest that photographic angular global alignment parameters correlate better with PROM results than photographic linear global alignment parameters. A similar phenomenon has been described for radiographic global alignment parameters [34].
The global body sagittal alignment analysis, including the head to the ankles is nowadays mandatory treating adult spinal deformity patients [20, 21, 40]. This can be evaluated only with the EOS low-dose imaging system (EOS imaging, Paris, France) [41].
Although EOS imaging has proven a decrease in radiation dose when compared to conventional radiography giving an equivalent or better image quality [42]. It has not reached widespread use yet due to the higher cost of an EOS machine [43].
If further developed, photographic sagittal plane analysis could provide an innocuous, and inexpensive assessment of total body sagittal alignment as well as lower limb lower-limb compensatory mechanisms.
Several limitations must be pointed out when interpreting the results of this pilot study. Since this is monocentric study with a small sample size, our results must be confirmed in a larger multicenter study. Like the vast majority of literature on ASD surgery [3, 5, 20, 24, 31] our study included patients with deformity caused by different etiological factors. Although we found some significant correlations between photographic sagittal parameters and PROM results their correlation coefficients were predominantly moderate. It should be noted that this limitation is commonly encountered in ASD research [4,5,6, 20, 33]. Moreover, the lack of preoperative photographic data in our study significantly limits its utility in the operative decision-making process. In addition, although the lumbar spinous processes are commonly used in literature as surface landmarks [44, 45], the placement of the L3 and T12 markers can sometimes be challenging. Several bony landmarks were used in our study for identifying lumbar spinous processes including de sacral base, Tuffier’s line and the 12th rib [46]. However, as the patient´s body mass index increases, palpation through increasing subcutaneous fat becomes more difficult [46] and the accuracy for marker placement may be compromised. Finally, a static photographic sagittal analysis does not take into account changes occurring during gait. A balanced but compensated spine, on static position, can become unbalanced when set in motion [21].
Despite these limitations, we provide the first photographic sagittal postural analysis in ASD patients. We provide preliminary evidence for the first time that sagittal photographic parameters may predict mid-term clinical results after ASD surgery. We also provide some ground for the use of clinical photographs for total body sagittal alignment assessment.
References
do Rosário JL (2014) Photographic analysis of human posture: a literature review. J Bodyw Mov Ther 18:56–61
Helmy NA, El-Sayyad MM, Kattabei OM (2015) Intra-rater and inter-rater reliability of Surgimap Spine software for measuring spinal postural angles from digital photographs. Bull Fac Phys Ther 20:193–199
Schwab FJ, Blondel B, Bess S, Hostin R, Shaffrey CI, Smith JS, Boachie-Adjei O, Burton DC, Akbarnia BA, Mundis GM, Ames CP, Kebaish K, Hart RA, Farcy JP, Lafage V, International Spine Study Group (ISSG) (2013) Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976) 38:E803–E812
Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR (2005) Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976) 30:682–688
Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F (2005) The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 30:2024–2029
Lafage V, Schwab F, Patel A, Hawkinson N, Farcy JP (2009) Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976) 34:E599–E606
Claeys K, Brumagne S, Deklerck J, Vanderhaeghen J, Dankaerts W (2016) Sagittal evaluation of usual standing and sitting spinal posture. J Bodyw Mov Ther 20:326–333
Schwab F, Blondel B, Chay E, Demakakos J, Lenke L, Tropiano P, Ames C, Smith JS, Shaffrey CI, Glassman S, Farcy JP, Lafage V (2014) The comprehensive anatomical spinal osteotomy classification. Neurosurgery 74:112–120
Vedantam R, Lenke LG, Bridwell KH, Linville DL, Blanke K (2000) The effect of variation in arm position on sagittal spinal alignment. Spine (Phila Pa 1976) 25:2204–2209
Miranda R, Schor E, Girão MJ (2009) Postural evaluation in women with chronic pelvic pain. Rev Bras Ginecol Obstet 31:353–360
Engsberg JR, Lenke LG, Bridwell KH, Uhrich ML, Trout CM (2008) Relationships between spinal landmarks and skin surface markers. J Appl Biomech 24:94–97
Claus AP, Hides JA, Moseley GL, Hodges PW (2009) Is “ideal” sitting posture real? Measurement of spinal curves in four sitting postures. Man Ther 14:404–408
Dunk NM, Lalonde J, Callaghan JP (2005) Implications for the use of postural analysis as a clinical diagnostic tool: reliability of quantifying upright standing spinal postures from photographic images. J Manip Physiol Ther 28:386–392
Saito ET, Akashi PM, Sacco Ide C (2009) Global body posture evaluation in patients with temporomandibular joint disorder. Clinics (Sao Paulo) 64:35–39
Ferreira EA, Duarte M, Maldonado EP, Burke TN, Marques AP (2010) Postural assessment software (PAS/SAPO): validation and reliabiliy. Clinics (Sao Paulo) 65:675–681
Cuccia AM, Carola C (2009) The measurement of craniocervical posture: a simple method to evaluate head position. Int J Pediatr Otorhinolaryngol 73:1732–1736
Guan X, Fan G, Wu X, Zeng Y, Su H, Gu G, Zhou Q, Gu X, Zhang H, He S (2015) Photographic measurement of head and cervical posture when viewing mobile phone: a pilot study. Eur Spine J 24:2892–2898
Vital JM, Senegas J (1986) Anatomical bases of the study of the constraints to which the cervical spine is subject in the sagittal plane: a study of the center of gravity of the head. Surg Radiol Anat 8:169–173
Suk KS, Kim KT, Lee SH, Kim JM (2003) Significance of chin-brow vertical angle in correction of kyphotic deformity of ankylosing spondylitis patients. Spine (Phila Pa 1976) 28:2001–2005
Kim YC, Lenke LG, Lee SJ et al (2017) The cranial sagittal vertical axis (CrSVA) is a better radiographic measure to predict clinical outcomes in adult spinal deformity surgery than the C7 SVA: a monocentric study. Eur Spine J 26:2167–2175
Le Huec JC, Thompson W, Mohsinaly Y, Barrey C, Faundez A (2019) Sagittal balance of the spine. Eur Spine J 28:1889–1905
Shimizu T, Lehman RA Jr, Sielatycki JA, Pongmanee S, Cerpa M, Takemoto M, Lenke LG (2020) Reciprocal change of sagittal profile in unfused spinal segments and lower extremities after complex adult spinal deformity surgery including spinopelvic fixation: a full-body X-ray analysis. Spine J 20:380–390
Larson AN, Schueler BA, Dubousset J (2019) Radiation in spine deformity: state-of-the-art reviews. Spine Deform 7:386–394
Yoshida G, Kurosu K, Yamato Y, Hasegawa T, Yasuda T, Togawa D, Matsuyama Y (2017) Novel Measurement technique for the sagittal vertical axis and its clinical application in adult spinal deformity. Asian Spine J 11:190–197
Knott P, Sturm P, Lonner B, Cahill P, Betsch M, McCarthy R, Kelly M, Lenke L, Betz R (2016) Multicenter comparison of 3D Spinal measurements using surface topography with those from conventional radiography. Spine Deform 4:98–103
Stolinski L, Kozinoga M, Czaprowski D, Tyrakowski M, Cerny P, Suzuki N, Kotwicki T (2017) Two-dimensional digital photography for child body posture evaluation: standardized technique, reliable parameters and normative data for age 7–10 years. Scoliosis Spinal Disord 12:38
Dubousset J (1994) Three-dimensional analysis of the scoliotic deformity. In: Weinstein SL (ed) Pediatric spine: principles and practice. Raven Press, New York, pp 480–481
Roussouly P, Nnadi C (2010) Sagittal plane deformity: an overview of interpretation and management. Eur Spine J 19:1824–1836
Protopsaltis T, Schwab F, Bronsard N, Smith JS, Klineberg E, Mundis G, Ryan DJ, Hostin R, Hart R, Burton D, Ames C, Shaffrey C, Bess S, Errico T, Lafage V, International Spine Study Group (2014) The T1 pelvic angle, a novel radiographic measure of global sagittal deformity, accounts for both spinal inclination and pelvic tilt and correlates with health-related quality of life. J Bone Jt Surg Am 96:1631–1640
Ha WS, Shin MH (2019) Postoperative lower limb compensation in patients with adult spinal deformity. J Clin Neurosci 59:106–111
Lafage R, Schwab F, Challier V, Henry JK, Gum J, Smith J, Hostin R, Shaffrey C, Kim HJ, Ames C, Scheer J, Klineberg E, Bess S, Burton D, Lafage V, International Spine Study Group (2016) Defining spino-pelvic alignment thresholds: should operative goals in adult spinal deformity surgery account for age? Spine (Phila Pa 1976). 41:62–68
Ware JE Jr (2000) SF-36 health survey update. Spine 25:3130–3139
Sánchez-Mariscal F, Gomez-Rice A, Izquierdo E, Pizones J, Zúñiga L, Alvarez-González P (2012) Correlation of radiographic and functional measurements in patients who underwent primary scoliosis surgery in adult age. Spine (Phila Pa 1976) 37:592–598
Qiao J, Zhu F, Xu L, Liu Z, Zhu Z, Qian B, Sun X, Qiu Y (2014) T1 pelvic angle: a new predictor for postoperative sagittal balance and clinical outcomes in adult scoliosis. Spine (Phila Pa 1976) 39:2103–2107
Kim HJ, Bridwell KH, Lenke LG, Park MS, Ahmad A, Song KS, Piyaskulkaew C, Hershman S, Fogelson J, Mesfin A (2013) Proximal junctional kyphosis results in inferior SRS pain subscores in adult deformity patients. Spine (Phila Pa 1976) 38:896–901
Takemoto M, Boissière L, Novoa F, Vital JM, Pellisé F, Pérez-Grueso FJ, Kleinstück F, Acaroglu ER, Alanay A, Obeid I, Obeid I, European Spine Study Group, ESSG (2016) Sagittal malalignment has a significant association with postoperative leg pain in adult spinal deformity patients. Eur Spine J 25:2442–2518
Zhang YP, Qian BP, Qiu Y, Qu Z, Mao SH, Jiang J, Zhu ZZ (2017) Sagittal vertical axis, spinosacral angle, spinopelvic angle, and T1 pelvic angle: which parameters may effectively predict the quality of life in ankylosing spondylitis patients with thoracolumbar kyphosis? Clin Spine Surg 30:E871–E876
Debarge R, Demey G, Roussouly P (2010) Radiological analysis of ankylosing spondylitis patients with severe kyphosis before and after pedicle subtraction osteotomy. Eur spine J 19:65–70
Obeid I, Boissière L, Yilgor C, Larrieu D, Pellisé F, Alanay A, Acaroglu E, Perez-Grueso FJ, Kleinstück F, Vital JM, Bourghli A, European Spine Study Group, ESSG (2016) Global tilt: a single parameter incorporating spinal and pelvic sagittal parameters and least affected by patient positioning. Eur Spine J 25:3644–3649
Diebo BG, Shah NV, Boachie-Adjei O, Zhu F, Rothenfluh DA, Paulino CB, Schwab FJ, Lafage V (2019) Adult spinal deformity. Lancet 394:160–172
Dubousset J, Charpak G, Skalli W, de Guise J, Kalifa G, Wicart P (2008) Skeletal and spinal imaging with EOS system. Arch Pediatr 15:665–666
Wybier M, Bossard P (2013) Musculoskeletal imaging in progress: the EOS imaging system. Jt Bone Spine 80:238–243
McKenna C, Wade R, Faria R et al (2012) EOS 2D/3D X-ray imaging system: a systematic review and economic evaluation. Health Technol Assess 16:1–188
Lenke LG, Engsberg JR, Ross SA, Reitenbach A, Blanke K, Bridwell KH (2001) Prospective dynamic functional evaluation of gait and spinal balance following spinal fusion in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 26:E330–E337
Shiba Y, Taneichi H, Inami S, Moridaira H, Takeuchi D, Nohara Y (2016) Dynamic global sagittal alignment evaluated by three-dimensional gait analysis in patients with degenerative lumbar kyphoscoliosis. Eur Spine J 25:2572–2579
Snider KT, Snider EJ, Degenhardt BF, Johnson JC, Kribs JW (2011) Palpatory accuracy of lumbar spinous processes using multiple bony landmarks. J Manipulative Physiol Ther 34:306–313
Acknowledgements
The authors wish to acknowledge Jose Dominguez Pallas, clinical photographer, for his involvement.
Funding
No financial support was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors state no conflict of interest.
Ethical approval
This study was approved by the institutional research ethics committee. Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work: AG-R, CM, EI, FM-M, JAFT, FS-M. Drafting the work or revising it critically for important intellectual content: AG-R, CM, EI, FM-M, JAFT, FS-M. Final approval of the version to be published: AG-R, CM, EI, FM-M, JAFT, FS-M. Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: AG-R, CM, EI, FM-M, JAFT, FS-M.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gomez-Rice, A., Madrid, C., Izquierdo, E. et al. Photographic sagittal plane analysis and its clinical correlation after surgery for adult spinal deformity: a preliminary study. Spine Deform 9, 501–514 (2021). https://doi.org/10.1007/s43390-020-00237-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-020-00237-8