Abstract
Background
The purpose of this study was to evaluate the effectiveness between percutaneous and open pedicle screw fixation without fusion for treating type A3 and A4 thoracolumbar fractures. Traumatic thoracolumbar burst fracture is a common pathology without a consensus on the best treatment approach. Percutaneous pedicle screw fixation (PPSF) systems have been recently introduced in the treatment of spinal fractures to reduce the adverse effects associated with the conventional open approaches, such as iatrogenic muscle denervation and pain.
Methods
A prospective analysis was made to evaluate consecutive 46 patients with type A3 and A4 thoracolumbar fractures. Patients were divided into a percutaneous pedicle screw fixation group (PPSF) and an open pedicle screw fixation group (OPSF). The mean age of patients in PPSF group (12 men, 11 woman) was 49.9 years and in OPSF group (10 men, 13 women) 52.2 years. For the purpose of evaluation, the radiological assessment of the bisegmental Cobb angle, the loss of correction, the volume of blood loss, operation time, cumulative radiation time and dose were recorded and compared.
Results
All patients were followed up for 12 months. There were no significant differences between OPSF and PPSF in the Cobb angle preoperative and postoperative angle and the loss of bisegmental correction. In PPSF group, the mean preoperative Cobb angle was 10.9° and improved by 4.5° postoperatively, and in OPSF group the preoperative angle was 12.1° and postoperatively improved by 3.8°. Significant differences between OPSF and PPSF were found in the mean cumulative radiation time, radiation dose and operation time. PPSF group also had a significantly lower perioperative blood loss.
Conclusions
Both open and percutaneous short-segment pedicle fixation were safe and effective methods to treat thoracolumbar burst fractures. Percutaneous fixation without fusion seems to be suitable for type A3 and A4 fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thoracolumbar fractures are usually high-energy injuries caused by motor vehicle or fall accidents. A large part of them involves the thoracolumbar junction. In an epidemiologic study by Hu et al. [1], traumatic injuries to the thoracolumbar region accounted for 75% of total spinal skeletal injuries.
The optimal treatment strategies for type A of thoracolumbar fractures remain controversial. Many reviews and meta-analyses on surgical strategies have been published, with a focus on fusion versus non fusion, minimally invasive surgery versus open surgery and anterior versus posterior approach [2,3,4,5]. The posterior open approach with fusion is considered appropriate for patients with burst fractures and posterior ligamentous complex injuries. General consensus exists that in less severe fractures (A0–A2) conservative treatment has the best risk/benefit ratio and that very severe fractures (B and C types) as well as patients with neurological compromise should be treated surgically. However, no such consensus exists in patients with incomplete (A3) and complete (A4) thoracolumbar burst fractures without neurological deficit [6, 7]. The aim of this study was to compare clinical and radiological outcomes between patients with thoracolumbar spine fractures treated either with open or percutaneous dorsal instrumentation without fusion.
Methods
This study was designed as a prospective cohort study. This study was performed between 2015 and 2016. Patients were randomly alternately included to both groups according to the common inclusion criteria: (1) thoracolumbar fracture classified as A3 or A4; (2) no other significant injury; (3) the absence of neurological deficits. The group under study included consecutive 46 patients, with only A3 and A4 fractures according to the present AO Spine classification, published by Vaccaro in 2013 were considered [8]. 23 patients (12 men and 11 women), aged 22–69 years (average 49.9 years), were enrolled into the percutaneous pedicle screw fixation (PPSF) group. The injury segments were T11 in 2 patients, T12 in 8, L1 in 9 and L2 in 4 patients. Mechanisms of injury included falls from a height (15 patients), traffic accidents (4 patients) and falls (4 patients). According to the AO fracture classification, A3 fracture occurred in 19 patients and A4 fracture in 4 patients. 23 patients, (10 men and 13 women) aged 29–74 years (average 52.2), were enrolled randomly into the open pedicle screw fixation (OPSF) control group. The injury segments were T12 in 7 patients, L1 in 12 and L2 in 4 patients. Mechanism of injury included falling from a height (15 patients), traffic accidents (3 patients), and falls (3 patients). According to the AO fracture classification, type A3 fracture occurred in 17 cases, A4 in 6 patients. In PPSF group, PathFinder NXT system (Zimmer Biomet) was implanted using four pedicle screws, one level above and one below the fractured vertebra. Patients in OPSF group were treated with open pedicle screw fixation system SOCON (Bbraun) with the same manner, one level above and one below the fractured vertebra without cross link and without fusion. For the purpose of evaluation, radiological assessment of the sagittal Cobb angle, the loss of correction, the volume of blood loss, operation time, radiation time and dose were recorded and compared. All patients were followed up for 12 months. We did not remove the metal or treat the anterior column for any patient in both groups.
Operative procedures
All patients were operated on by two experienced trauma and spine surgeons. The patients were in the prone position, with a pad beneath breast and pelvis to increase the lordosis and to obtain partial reduction.
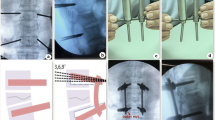
23 patients were treated by short segment, minimally invasive, percutaneous pedicle screw instrumentation. Four small incisions were made and the transpedicular guide wires were inserted by means of fluoroscopy. The surrounding tissues were stripped off with dilatators. The cannulated pedicle screws were slid over the guide wires. The position of the pedicle screws was controlled via fluoroscopy. The cranial incisions allowed percutaneous insertion of the rods (Fig. 1a).
The control group was composed of 23 patients who were stabilized using a short segment construct through a standard midline incision. The position of the pedicle screws was controlled via fluoroscopy (Fig. 1b). There was no fusion performed in the control group.
Postoperative treatment
Patients were mobilized on the second day after surgery, when wound drains (OPSF group) and urinal catheter were removed. A clinical and radiological check-up took place after 6 weeks, 3 months, 6 months and 12 months. There was no construct failure or others complications recorded during follow-up.
All the data were analysed using Minitab 15 Statistical software (Minitab Inc., State College, PA, USA). Descriptive statistics including mean, minimum and maximum value, median, were used to describe PPSF (23 patients) and OPSF (23 patients) data (Tables 1, 2). The Anderson–Darling test was used to determine whether data meets the assumption of normality (Table 3). The paired Student’s t test and Wilcoxon signed-rank tests were used to compare Cobb variables in groups PPSF and OPSF (Tables 4, 5). The Wilcoxon signed-rank test does not assume normality in the data. The boxplot was plotted to assess and compare Cobb sample distributions (Fig. 2a, b). All variables were compared between PPSF and OPSF groups (Table 6). One-way ANOVA test was performed to compare normally distributed variables. Where the normality assumption was not met, the nonparametric Kruskal–Wallis test was used. Statistical differences were considered to be significant when the p value was less than or equal to 0.05.
Results
In PPSF group, the mean preoperative Cobb angle was 10.9° (range 0.7°–25.8°) and postoperatively improved by 4.5°(range 0°–10.0°). In OPSF group, the mean preoperative Cobb angle was 12.1° (range 3.5°–16.5°) and postoperatively improved by 3.8° (range 0.6°–7.5°). No significant differences were found between OPSF and PPSF in the loss of bisegmental correction after 1 year. The mean surgical duration in the percutaneous screw group was on average 49.7 min (range 29.0–65.0), compared with the average of 52.0 min (range 44.0–70.0) in the OPSF group. The percutaneous screw group had a lower perioperative blood loss of 29.0 ml (range 19.0–40.0) compared with 328.7 ml (range 150.0–600.0) in the OPSF group. The cumulative radiation dose ranged from 188.0 to 540.0 and averaged 379.9 cGycm2 in PPSF group, and from 147.0 to 284.0 with the average of 207.6 cGycm2 in OPSF group. The C-arm exposure time was in average 29.0 s (range 15.0–50.0) in PPSF group and 17.3 s (range 13.0–23.0) in OPSF group. There were no neurological, wound infections or medical complications in both groups.
Discussion
The advantages of percutaneous technique are preservation of posterior musculature, less blood loss, shorter operative time, and lower infection risk. Lee et al. [9] also revealed that PPSF provided relatively earlier pain relief and functional improvement in comparison with OPSF.
Limitations of percutaneous fixation include the inability to achieve direct spinal canal decompression and impossibility to perform a fusion.
Diniz [10] published a systematic review and meta-analysis of the articles, compared the use and non-use of fusion in association with internal fixation for the treatment of thoracolumbar burst fractures. The data reviewed in this study suggest that the use of fusion did not improve clinical outcomes, but it was associated with increased surgical time and higher intraoperative bleeding and did not promote significant improvement in radiological parameters. No significant difference between groups in the degree of kyphosis correction, loss of kyphosis correction, or final angle of kyphosis was observed.
Kim et al. [11] found that the pre-surgery and post-surgery cross-sectional areas of the multifidus muscle showed no statistically significant differences in the PPSF group, but in the conventional posterior group, muscle atrophy was significant. Wild et al. [12] reported statistically lower blood loss in trauma cases after the internal fixation was implanted percutaneously than when implanted during an open procedure. Wang et al. [13] retrospectively reviewed 100 patients who were treated with open or percutaneous pedicle screws after a thoracolumbar fracture. All fractures were type A fractures, and no patient had a neurologic deficit. Patients underwent either short-segment open pedicle instrumentation or MIS short-segment pedicle fixation with four or six screws. A fusion was not performed. Postsurgical improvement in the clinical outcomes was seen in terms of blood loss, operation time, postoperative hospital stay, and VAS scores in the MIS group. Radiographically, postoperative sagittal Cobb angle, vertebral body angle, and anterior vertebral body height (VBH) were similar between all treatment arms. In the open group, one patient had poor wound healing and one patient had a loose screw. Vanek et al. [14] evaluated 37 patients treated with either percutaneous or open posterior short-segment pedicle screw fixation with fusion. All patients were thoracolumbar types A3.1–A3.3 without neurologic deficit. The authors found a significant decrease in mean surgical duration and mean perioperative blood loss in the MIS group. The VAS scores were also significantly lower in the first 7 postoperative days in the MIS group. There were no significant differences between the groups in vertebral body index and Cobb angle during follow-up. Bronsard et al. [15] published a study comparing radiation exposure doses between percutaneous pedicular screwing and open reduction internal fixation in the lumbar spine, showing that radiation dose was threefold higher in PPSF than in OPSF group. In the current study, twofold radiation dose we observed in PPSF group.
Phan et al. [16] evaluated 12 studies. There were 279 patients undergoing percutaneous fixation, compared with 340 open fixation procedures. Operative duration was significantly shorter in the percutaneous group, by 19 min. The percutaneous approach was also associated with shorter hospital stay by 5.7 days. Whilst there was no difference in screw malpositioning, the percutaneous approach had lower rates of infections and superior visual analogue scale. No difference was found between the groups in terms of postoperative Cobb angle, postoperative body angle, and postoperative anterior body height. Kreinest et al. [17] analysed perioperative complications of open versus percutaneous dorsal instrumentation after dorsal stabilization in patients suffering from fractures of the thoracic and lumbar spine. Open surgery was carried out on 169 patients and percutaneous surgery procedure was carried out on 322 patients. Fracture level ranged from T1 to L5. The complication rate was 14.8% in open surgical group and 5.3% in percutaneous surgical approach. Postoperative hospital stay was also reduced significantly in percutaneous group.
Kumar et al. [18] compared traditional open spinal surgery, minimally interventional surgery (MIS) and conservative management of thoracolumbar burst fractures in their prospective study. 30 patients were treated conservatively, 23 patients were treated via open approach and 25 patients were treated via MIS techniques. Analysis of data showed there was no difference in degree of post-traumatic kyphosis between the groups. Those patients treated with MIS techniques demonstrated superior outcomes compared to open surgery and conservative methods of treatment, with significantly reduced hospital stay and better return to work.
Tinelly et al. [19] published the results of reduction and the accuracy of screw placement in minimally invasive percutaneous posterior instrumentation. 34 of 542 screws (6.3%) in 22 patients (17.3%) were misplaced, but misplaced was minimal without neurological deficit. Most of the vertebral body fractures (82/64.5%) were located in the thoracolumbar junction. Kyphosis of these fractures changed from mean 2.5° ± 6° to 5.6° ± 5.7° lordosis (p < 0.001) and lordosis in the 45 lumbar fractures from mean 6.9° ± 10.3° to 14.5° ± 8.8° lordosis (p < 0.001).
In summary, our results suggested that PPSF had a less intraoperative blood loss, but radiation exposure dose was twofold higher than in OPSF group. No differences were found between the groups in terms of postoperative Cobb angle and loss of correction.
Conclusion
Patients with type A3 and A4 thoracolumbar fractures can be effectively managed with percutaneous or open pedicle screw placement. PPSF had a less intraoperative blood loss, but radiation exposure dose was twofold higher than in OPSF group. No differences were found between the groups in terms of postoperative Cobb angle and loss of correction. This study is limited, because it shows radiological 1 year results before material removal. In our study, none of the patients received additional ventral stabilization using cages or plates. The A3 and A4 fractures were not differentiated. It is known that the rupture of two discs leads to more loss of reduction compared to one. This study supports the hypothesis that percutaneous spine fixation can be effectively applied to a group of thoracolumbar spine fractures type A3 er A4 without neural compression. Blood loss was decreased in the percutaneous group, which may represent a potential benefit, particularly in the polytraumatized patient.
References
Hu R, Mustard CA, Burns C. Epidemiology of incident spinal fracture in a complete population. Spine (Phila Pa 1976). 1996;21(4):492–9.
Tian NF, Wu YS, Zhang XL, Wu XL, Chi YL, Mao FM. Fusion versus nonfusion for surgically treated thoracolumbar burst fractures: a meta-analysis. PloS One. 2013;8:e63995.
Barbagallo GM, Yoder E, Dettori JR, Albanese V. Percutaneous minimally invasive versus open spine surgery in the treatment of fractures of the thoracolumbar junction: a comparative effectiveness review. Evid Based Spine Care J. 2012;3:43–9.
Boerger TO, Limb D, Dickson RA. Does ‘canal clearance’ affect neurological outcome after thoracolumbar burst fractures? J Bone Jt Surg Br. 2000;82:629–35.
Xu GJ, Li ZJ, Ma JX, Zhang T, Fu X, Ma XL. Anterior versus posterior approach for treatment of thoracolumbar burst fractures: a meta-analysis. Eur Spine J. 2013;22:2176–83.
Verheyden AP, Holzl A, Ekkerlein H, Gercek E, Hauck S, Josten C, et al. Recommendations for the treatment of thoracolumbar lumbar spine injuries. Unfallchirurg. 2011;114:9–16.
Rometsch E, Spruit M, Hartl R, McGuire RA, Gallo-Kopf BS, Kalampoki V, Kandziora F. Does Operative or nonoperative treatment achieve better results in A3 and A4 spinal fractures without neurological deficit? Systematic literature review with meta-analysis. Glob Spine J. 2017;7(4):350–72.
Vaccaro AR, Oner C, Kepler CK, Dvorak M, Schnake K, Bellabarba C, et al. AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine (Phila Pa 1976). 2013;38:2028–37.
Lee JK, Jang JW, Kim TW, Kim TS, Kim SH, Moon SJ. Percutaneous short-segment pedicle screw placement without fusion in the treatment of thoracolumbar burst fractures: is it effective?: comparative study with open short-segment pedicle screw fixation with posterolateral fusion. Acta Neurochir (Wien). 2013;155:2305.
Diniz JM, Botelho RV. Is fusion necessary for thoracolumbar burst fracture treated with spinal fixation? A systematic review and meta-analysis. J Neurosurg Spine. 2017;27:584–92.
Kim DY, Lee SH, Chung SK, Lee HY. Comparison of multifidus muscle atrophy and trunk extension muscle strength: percutaneous versus open pedicle screw fixation. Spine (Phila Pa 1976). 2005;30(1):123–29.
Wild MH, Glees M, Plieschnegger C, Wenda K. Five-year follow-up examination after purely minimally invasive posteriori stabilization of thoracolumbar fractures: a comparison of minimally invasive percutaneously and conventionally open treated patients. Arch Orthop Trauma Surg. 2007;127(5):335–43.
Wang H, Zhou Y, Li C, Liu J, Xiang L. Comparison of open versus percutaneous pedicle screw fixation using the sextant system in the treatment of traumatic thoracolumbar fractures. Clin Spine Surg. 2017;30(3):E239–46.
Vanek P, Bradac O, Konopkova R, de Lacy P, Lacman J, Benes V. Treatment of thoracolumbar trauma by short-segment percutaneous transpedicular screw instrumentation: prospective comparative study with a minimum 2-year follow-up. J Neurosurg Spine. 2014;20(2):150–6.
Bronsard N, Boli T, Challali M, de Dompsure R, Amoretti N, Padovani B, Bruneton G, Fuchs A, de Peretti F. Comparison between percutaneous and traditional fixation of lumbar spine fracture: intraoperative radiation exposure levels and outcomes. OrthopTraumatol Surg Res. 2013;99(2):162–8.
Phan K, Rao PJ, Mobbs RJ. Percutaneous versus open pedicle screw fixation for treatment of thoracolumbar fractures: Systematic review and meta-analysis of comparative studies. Clin Neurol Neurosurg. 2015;135:85–92.
Kreinest M, Rillig J, Grutzner PA, Kuffer M, Tinelli M, Matschke S. Analysis of complications and perioperative data after open or percutaneous dorsal instrumentation following traumatic spinal fracture of the thoracic and lumbar spine: a retrospective cohort study including 491 patients. Eur Spine J. 2017;26(5):1535–40.
Kumar A, Aujla R, Lee Ch. The management of thoracolumbar burst fractures: a prospective study between conservative management, traditional open spinal surgery and minimally interventional spinal surgery. SpringerPlus. 2015;4:204.
Tinelly M, Topfer F, Kreinest M, Matschke S, Grutzer PA, Suda AJ. Minimally invasive reduction and percutaneous fixation of one-level traumatic thoracolumbar and lumbar spine fractures. Eur J Orthop Surg Traumatol. 2018. https://doi.org/10.1007/s00590-018-2224-9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Ethical approval
This study was approved by the appropriate medical local ethics committee.
Rights and permissions
About this article
Cite this article
Kocis, J., Kelbl, M., Kocis, T. et al. Percutaneous versus open pedicle screw fixation for treatment of type A thoracolumbar fractures. Eur J Trauma Emerg Surg 46, 147–152 (2020). https://doi.org/10.1007/s00068-018-0998-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-018-0998-4