Abstract
Background
The introduction of magnetic expansion control growth rods for the surgical management of EOS has gained popularity. However, there are no published studies on the incidence of proximal junctional kyphosis (PJK) using this technique.
Purpose
The aim of this study is to report the incidence of PJK following treatment with magnetic growth rods in EOS.
Methods
Retrospective review of data from 21 cases (12 males, 9 females) over 3 years. PJK was obtained from whole spine X-rays pre-op, immediate post-op and last follow-up. Cobb angle was measured between the superior end plate of vertebra two levels above the upper instrumented vertebra (UIV) and the inferior end plate of the UIV. A difference of >10° between the pre-operative x-rays and the last follow-up X-rays was recorded as PJK.
Results
6/21 (28.6 %) had proximal junctional kyphosis of more than 10° at last follow-up. Average age was 5.3. Average follow-up was 32.5 months. All the patients with PJK were syndromic. Four out of these six patients were males (66 %). Average PJK angle was 25.55°. Average pre-operative kyphosis was 52.5°. Average number of distractions was 7.4. All six patients had syndromic association. 3/6 patients (50 %) were conversion cases treated with traditional growth rods previously (TGR). None of the patients required unplanned surgery for PJK.
Conclusion
The incidence of PJK in EOS patients treated with magnetic rods is favourably comparable to that reported with traditional growth rods. Also, children who are male, syndromic, hyperkyphotic, and younger must be monitored closely.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Goals of surgical treatment for early onset scoliosis (EOS) include stabilization of the spinal deformity and optimization of the space available for the lung until the child reaches skeletal maturity and is ready for a definitive spinal fusion. The growing rod technique has been successfully used to treat spinal deformity and prevent cardiopulmonary compromise in the children who suffer from EOS [1–3]. Several authors have described various techniques of growing rod application, starting from Harrington (1962) who described the use of a single rod on the concave side of the major curve [4] to Akbarnia et al. [5] who popularised the usage of dual rod technique for management of EOS.
Recently, magnetically controlled expansile growth rods (MCGR) are gaining popularity with good early results in children suffering from EOS [6, 7]. This magnetically controlled rod construct is a minimally invasive system with noninvasive adjustment capabilities. It allows bi-directional axial adjustment as well as precision incremental distraction.
With the new techniques and technology, we have been able to overcome some of the problems and complications associated with EOS but despite these improvements, the complication rate remains relatively high [8–11]. Very little literature is available on the incidence of proximal junctional kyphosis (PJK) in children treated with growing rods for EOS [11, 12].
Our purpose is to report on the incidence of PJK following treatment with magnetic growth rods in EOS at our centre. Contrary to previously documented distraction techniques commonly associated with PJK, we have used a new method known as the ‘Tail-Gating Technique’ which uses the incremental distraction capabilities of the MCGR to ‘shadow’ growth. Distractions were done 3 monthly. The amount of distraction was calculated from the Dimeglio growth charts which describe the relationship between annual growth velocity (AGV) of T1–L5 spinal segments and expected weight for chronological age of the child: (1) birth to 5 years—20 kg with AGV of 2.2 cm/year, (2) 5 to 10 years—30 kg at 1.1 cm/year, and (3) 10 years to puberty—>30 kg at 1.8 cm/year. These figures are then divided by 4 to give the incremental distance rounded to the nearest figure by which the rod is distracted at each visit.
Materials and methods
We prospectively reviewed 21 patients with EOS who underwent dual MCGR spinal instrumentation, over a period of 3 years from 2011 to 2014. The inclusion criteria were:
-
1.
Patients who the surgeon felt would benefit from the use of the magnetic rods and
-
2.
In whom parental consent was taken.
-
3.
A minimum of two lengthening procedures.
Patient diagnosis, demographics, surgical information, including levels of instrumentation, type of instrumentation, radiographical measurements and complications were recorded. Radiographs were evaluated by two authors. Three lateral view standing radiographs were evaluated as follows:
-
1.
Pre-operatively,
-
2.
After index MCGR surgery (prior to the first formal lengthening).
-
3.
Latest follow-up.
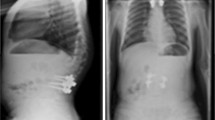
Proximal junctional kyphosis was measured from the superior endplate of two vertebral levels above the upper instrumented vertebra (UIV) to the inferior endplate of the upper instrumented vertebra [11, 14, 15]. A difference of more than 10° between the pre-op X-rays and the last follow-up X-rays was recorded as PJK Fig. 1.
Statistics
All analysis of raw data was performed using GraphPad Prism Version 6 (GraphPad Software, Inc. San Diego California, USA. A Kolmogorov–Smirnov test has been used to assess normality. Results demonstrated that the data did not fit a Gaussian distribution, and thus nonparametric testing was performed. Paired data was analysed with Wilcoxon matched-pairs signed-rank test and unpaired data with Mann–Whitney U test. Correlation was assessed using Spearman’s correlation co-efficient.
The following groups were analysed to assess if there were significant differences:
-
Pre-operative, immediate post-operative and last post-operative follow-up kyphosis.
-
Males and females with regard to PJK angle
-
Syndromic vs idiopathic
-
Age <5 vs >5
-
History of previous growth rod surgery
Correlation analysis was performed with regard to age and PJK angle and pre-op kyphosis and PJK angle.
Results
There were 12 male and 9 female patients with an average age of 7.7 years at the time of surgery (range 3–12 years). Average follow-up for all patients was 23.4 months. Average number of distractions was 7.4. Three patients had idiopathic scoliosis, three had visceral associations, two had central core myopathy, and one patient each had a neuromuscular disorder, congenital hemivertebra and arthrogryposis. The remaining patients (10) were syndromic. The visceral associations in the syndromic cases were multi-systemic. Examples of some of the syndromic cases were chromosome 17 disorder, Prader–Willi syndrome, Hurler syndrome, CHARGE syndrome, Stickler syndrome, Smith–Lemli–Opitz syndrome, VACTERL syndrome and Goldenhar syndrome. Some of the syndromic cases had no known diagnosis.
More than half of the patients (11/21) had been treated with traditional growing rod systems before being converted to MCGR. All patients had screw anchors at the upper instrumented level except one patient (hooks).
Tables 1, 2 shows the age, diagnosis, levels of instrumentation and whether the patients had primary surgery previously.
The thoracic kyphosis values (pre-operative and post-operative) from T4 to T12 were comparable in both the groups, i.e. PJK and non-PJK groups. We compared the pre- and post-operative values of thoracic kyphosis T4–T12 for both the groups as shown in Tables 3, 4.
Proximal junctional kyphosis—6/21 (28.6 %) had proximal junctional kyphosis of more than 10° at last follow-up. Average age of these children was 5.3 (range 4–7 years). Average follow-up was 32.5 months. Tables 5, 6, 7 summarises the demographics and diagnosis of these six children.
All the patients with PJK were syndromic. 4/6 patients were males (66 %). Average PJK angle was 25.55 (range 10.6–35.1). The proximal fixation was the same, i.e. screws, in all six children. All of them had long constructs from proximal thoracic levels to lower lumbar levels (i.e. T3, 4 to L4, 5) except one.
The average thoracic kyphosis (measured from T1 to T12) in the whole cohort before surgery was 48.8° (range 16.9°–81.6°) and after surgery was 47.8° (range 15.1°–86.4°). The six children with PJK had an average pre-operative thoracic kyphosis of 52.5° (range 38.9°–67.5°) compared to an average of 47.3° (range 16.9°–81.6°) in the rest of the cohort. 3/6 children had been treated with growing rods before conversion to MCGR.
Statistics
A Kolmogorov–Smirnov test on pre-op Kyphosis and PJK angle demonstrated a non-Gaussian distribution (p = 0.12).
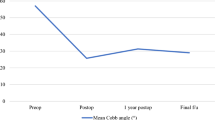
Analysis of pre-op and immediate post-op kyphosis (Wilcoxon matched-pairs signed-rank test) demonstrated a significant decrease in kyphosis (p = 0.0002) with the median decreasing by 11 degrees. Similarly, there was a significant increase in kyphosis between the immediate post-operative and latest follow-up (p = 00035) with the median increasing by eight. However, there was no difference between pre-operative and late post-operative kyphosis (p = 0.89). The results suggest that the technique itself had no significant long term effect on kyphosis although in the short term kyphosis was decreased.
The median kyphosis angle in males was higher than females (8.3 vs 2.1) but this failed to reach significance (p = 0.24 Mann–Whitney U test) Fig. 2.
When PJK angles were compared between syndromic and idiopathic curves, the angle appeared greater for syndromic curves with a median of 5.2 vs 0.9 for idiopathic curves. Again, this did not achieve significance (p = 0.15 Mann–Whitney U test) Fig. 3.
Patients with an age at the initial surgery of less than 5 years had a median PJK angle of 24° vs 5° in those over 5 years (p = 0.54) Fig. 4.
This overall trend seems to be further illustrated when correlation analysis was performed. Spearman’s test demonstrated a correlation co-efficient of −0.19 suggesting a negative correlation between age and PJK angle Fig. 5.
There was no significant difference between those who had had previous growth rod treatment vs those who underwent de novo surgery with regard to PJK angle (p = 0.52 Mann–Whitney U test) Fig. 6.
There was a negative correlation between pre-op kyphosis and PJK angle (Spearman’s test with a correlation co-efficient of −0.225) suggesting that those already with substantial kyphosis were not made any more kyphotic by the procedure Fig. 7.
In summary, patients underwent a significant decrease in kyphosis initially but there was no significant difference between pre-op and last follow-up post-op kyphosis. Several trends seemed apparent. There was a negative correlation between age and PJK angle and Pre-op kyphosis and PJK angle. Males appeared to have a higher PJK angle than females as did syndromic patients vs idiopathic. Finally, previous growth rod surgery did not make a difference with regard to PJK angle. With larger numbers these trends may reach significance.
Complications no reoperations were performed for PJK.
Discussion
Proximal junctional kyphosis is a major complication in the management of spinal deformity. There is a paucity of literature available on the incidence of PJK in the management of early onset scoliosis and we believe there is no literature available on PJK in such patients treated with MCGR. Our primary study aim was to report on the incidence of PJK with a new device and distraction technique and secondarily, look at the possible contributing factors. This is the first study reporting on this complication in a patient cohort treated with a standardised new distraction technique performed by a single surgeon.
The tail-gating technique seeks to use charts of expected spinal growth based on age and weight to control spinal deformity and modulate growth of the spine in EOS. MCGR distraction at each clinic visit is incremental and does not seek to stimulate spinal growth by applying maximum but safe distraction forces as in TGR treatment. We believe the use of TGT minimises potential deforming forces on both the spinal anchor sites and the spine itself due to the minimalistic nature of the distraction. Also, the fusion levels were selected on the basis of the proximal and distal end vertebra of the curve. Once these landmarks had been identified the adjacent neutral vertebra was chosen as a second anchor site. This method, in the senior authors (CN) experience, allows for good correction of the spinal deformity.
Shah et al. [11] reported 45 % incidence of PJK in all screw constructs in their study. Watanabe et al. [12] reported 26 % incidence of PJK in their study but they considered a proximal junction angle of 20° greater than the pre-operative measurement as PJK. The incidence of PJK (a difference of 10°) in our group (all screw proximal foundation) was 28 % which is lesser than the incidence reported by other authors [11, 12]. There were common associations in the group of children with PJK in our cohort, namely:
-
1.
All the children with PJK were syndromic.
-
2.
Higher incidence of males (4/6).
-
3.
Younger age group compared to rest of cohort (5.3 years).
-
4.
Higher number of distractions in the PJK group (avg. 10.5 compared to 6.3 in the rest of cohort).
-
5.
Pre-operative hyperkyphosis (avg. 52.5°).
Thoracic hyperkyphosis has been reported to be an important risk factor for PJK [11–13]. Watanabe et al. [12] reported that a kyphosis of 60° or more is a significant risk factor for PJK. In our cohort with PJK, only two patients had thoracic kyphosis of more than 60°. The same study found that the distal instrumented vertebra at L4 or distal level reduced the chances of PJK, but in our study group, all patients with PJK had their distal instrumented vertebra at L4 or distal level.
Shah et al. [11] suggested that PJK in EOS patients treated with mechanical growing rods, increases over time but had no correlation to the number of distractions. Similarly, in our patients treated with MCGR who had PJK, the average follow-up period was longer but the number of distractions was also higher than the rest of the cohort. It stands to reason that the longer such patients are under follow-up, higher the number of distractions they will have.
Shroerlucke et al. [13] suggested that syndromic children are more prone to complications including PJK. All our patients with PJK were syndromic. Of the six patients, three had been previously subjected to a well recognised kyphosing treatment in the form of traditional growth rods (TGR). Although present in 6/21 patients, the magnitude of PJK is lower when compared to previous reports [11, 12] which would indicate a slower rate of progression of PJK when using the TGT. The results also show that PJK was commoner in the younger male patient with more distractions.
The magnetically controlled rod is a hypokyphosis inducing device due to its geometry. Each distraction rod has a non-shapeable actuator section which houses the internal magnets and a shapeable rod section. The actuator section is 9 mm in diameter and 90 mm long. The shapeable rod section comes in diameter sizes of 4.5, 5.5 and 6 mm. The proximal rod end measures 256 mm and the distal rod end measures 109 mm. The actuator portion of the rod is placed over the thoracic spine and because of its non-shapeable structure tends to push down on the thoracic spine, thereby reducing the kyphosis. J Cheung et al. [16] have pointed out this drawback with MCGR and are of the opinion that distraction with MCGR causes flattening of thoracic spine, predisposing to PJK. In our experience, the shapeable proximal rod can be contoured into kyphosis and with each incremental distraction kyphosis of the thoracic spine is slowly regained as is seen with the last follow-up measurements.
In their paper, Atici et al. [17] suggested that flatback, proximal junctional kyphosis, distal junctional kyphosis, fixed sagittal imbalance, implant related complications may emerge due to the blocking effect of the implant in the children, on the dynamic changes of spinal sagittal parameters. However, planning and follow-up of the treatment according to the normal paediatric spinal sagittal parameters may help in preventing the complications. We agree that treatment of these children should take normal parameters into account for more predictable results.
El-Hawary et al. [18] conducted a nonconsecutive multicentre study on EOS treated with TGR and had similar conclusions that the spinal sagittal parameters strongly influence the risk of PJK in there group of patients. In their study, risk ratio for developing PJK was 2.8 with pre-operative hyperkyphosis and 3.1 for patients with high pelvic incidence.
Surgically treated EOS with MCGR has high complication rate. Hickey et al. [19], in their small series of six patients treated with MCGR, reported one case of screw pull out, one case of rod breakage and one case of proximal junctional kyphosis at a minimum follow-up of 2 months. As in other series, their complication rate in the management of EOS is high but they concluded that MCGR effectively controls early onset scoliosis when used as either a primary or revision procedure.
The main limitations to this study are the small number of patients in the cohort and the relatively short follow-up. Ideally, a larger group of patients and a longer follow-up would be required to detect any device related complications or anchor site failures. However, we feel that in a novel device such as the magnetic growth rod system, it is important to highlight any well-established problems normally associated with traditional growing rod systems. This can only enhance the evaluation of the safety and performance of the new system and make it easier to benchmark against predicate devices.
An advantage of the study is that the data has been collected prospectively and independently of the senior author (CN) by the members of a dedicated research team. All radiographs were independently reviewed by two experienced spinal surgeons. The distraction technique (TGT) was standardised and performed by a single surgeon (CN) using spinal growth charts [20]. This study also represents the longest follow-up of a single centre cohort of patients using this technique.
Conclusion
The incidence of PJK in EOS patients treated with MCGR is favourably comparable to that reported with the use of TGR. The use of the tail-gating technique appears to reduce the magnitude and lower the rate of progression of PJK when compared to previous reports.
Also, children who are male, syndromic, hyperkyphotic, and younger must be monitored closely and parents should be counselled regarding the higher incidence of PJK in this group.
References
Pehrsson K, Larsson S, Oden A, Nachemson A (1992) Long-term follow-up of patients with untreated scoliosis. A study of mortality, causes of death, and symptoms. Spine (Phila Pa 1976) 17(9):1091–1096
Swank SM, Winter RB, Moe JH (1982) Scoliosis and cor pulmonale. Spine (Phila Pa 1976) 7(4):343–354
Campbell RM Jr, Smith MD (2007) Thoracic insufficiency syndrome and exotic scoliosis. J Bone Joint Surg Am 89(Suppl 1):108–122 (Review)
Harrington PR (1962) Treatment of scoliosis. Correction and internal fixation by spine instrumentation. J Bone Joint Surg Am 44-A:591–610
Akbarnia BA, Marks DS, Boachie-Adjei O, Thompson AG, Asher MA (2005) Dual growing rod technique for the treatment of progressive early-onset scoliosis: a multicenter study. Spine (Phila Pa 1976) 30(17 Suppl):S46–S57
Hickey BA, Towriss C, Baxter G, Yasso S, James S, Jones A, Howes J, Davies P, Ahuja S (2014) Early experience of MAGEC magnetic growing rods in the treatment of early onset scoliosis. Eur Spine J 23(Suppl 1):S61–S65
Dannawi Z, Altaf F, Harshavardhana NS, El Sebaie H, Noordeen H (2013) Early results of a remotely-operated magnetic growth rod in early-onset scoliosis. Bone Joint J 95(B(1)):75–80
Akbarnia BA, Breakwell LM, Marks DS, McCarthy RE, Thompson AG, Canale SK, Kostial PN, Tambe A, Asher MA, Growing Spine Study Group (2008) Dual growing rod technique followed for three to eleven years until final fusion: the effect of frequency of lengthening. Spine (Phila Pa 1976) 33(9):984–990
Bess S, Akbarnia BA, Thompson GH, Sponseller PD, Shah SA, El Sebaie H, Boachie-Adjei O, Karlin LI, Canale S, Poe-Kochert C, Skaggs DL (2010) Complications of growing-rod treatment for early-onset scoliosis: analysis of one hundred and forty patients. J Bone Joint Surg Am 92(15):2533–2543
Thompson GH, Akbarnia BA, Kostial P, Poe-Kochert C, Armstrong DG, Roh J, Lowe R, Asher MA, Marks DS (2005) Comparison of single and dual growing rod techniques followed through definitive surgery: a preliminary study. Spine (Phila Pa 1976) 30(18):2039–2044
Shah SA, Karatas AF, Dhawale AA, Dede O, Mundis GM Jr, Holmes L Jr, Yorgova P, Neiss G, Johnston CE, Emans JB, Thompson GH, Pawelek JB, Akbarnia BA, Growing Spine Study Group (2014) The effect of serial growing rod lengthening on the sagittal profile and pelvic parameters in early-onset scoliosis. Spine (Phila Pa 1976) 39(22):E1311–E1317
Watanabe K, Uno K, Suzuki T, Kawakami N, Tsuji T, Yanagida H, Ito M, Hirano T, Yamazaki K, Minami S, Taneichi H, Imagama S, Takeshita K, Yamamoto T, Matsumoto M (2014) Risk Factors for Proximal Junctional Kyphosis Associated with Dual-Rod Growing-Rod Surgery for Early-Onset Scoliosis. J Spinal Disord Tech. doi:10.1097/BSD.0000000000000127
Schroerlucke SR, Akbarnia BA, Pawelek JB, Salari P, Mundis GM Jr, Yazici M, Emans JB, Sponseller PD, Growing Spine Study Group (2012) How does thoracic kyphosis affect patient outcomes in growing rod surgery? Spine (Phila Pa 1976) 37(15):1303–1309
Kim YJ, Bridwell KH, Lenke LG, Kim J, Cho SK (2005) Proximal junctional kyphosis in adolescent idiopathic scoliosis following segmental posterior spinal instrumentation and fusion: minimum 5-year follow-up. Spine (Phila Pa 1976) 30(18):2045–2050
Glattes RC, Bridwell KH, Lenke LG, Kim YJ, Rinella A, Edwards C II (2005) Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976) 30(14):1643–1649
Cheung Jason Pui Yin, Cahill Patrick, Yaszay Burt, Akbarnia Behrooz A, Cheung Kenneth MC (2015) Special article: update on the magnetically controlled growing rod: tips and pitfalls. J Orthop Surg 23(3):383–390
Atici Y, Akman YE, Erdogan S, Sari S, Yavuz U, Carkci E, Kaygusuz MA (2015) The effect of growing rod lengthening technique on the sagittal spinal and the spinopelvic parameters. Eur Spine J 24:1148–1157
El-Hawary R, Sturm P, Cahill P, Samdani A, Vitale M, Gabos P, Bodin N, d’Amato C, Harris C, Al Khudairy A, Smith JT (2015) What is the risk of developing proximal junctional kyphosis during growth friendly treatments for early-onset scoliosis? J Pediatr Orthop. doi:10.1097/BPO.0000000000000599
Hickey BA, Towriss C, Baxter G, Yasso S, James S, Jones A, Howes J, Davies P, Ahuja S (2014) Early experience of MAGEC magnetic growing rods in the treatment of early onset scoliosis. Eur Spine J 23(Suppl 1):S61–S65
Dimeglio A, Bonnel F, Canavese F (2010) Normal growth of the spine and thorax. The growing spine, Springer, Berlin, Heidelberg, pp 13–42
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Inaparthy, P., Queruz, J.C., Bhagawati, D. et al. Incidence of proximal junctional kyphosis with magnetic expansion control rods in early onset scoliosis. Eur Spine J 25, 3308–3315 (2016). https://doi.org/10.1007/s00586-016-4693-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4693-z