Abstract
Purpose
Narrow cervical canal (NCC) has been a suspected risk factor for later development of cervical myelopathy. However, few studies have evaluated the prevalence in asymptomatic subjects. The purpose of this study was to investigate the prevalence of NCC in a large cohort of asymptomatic volunteers.
Methods
This study was a cross-sectional study of 1211 asymptomatic volunteers. Approximately 100 men and 100 women representing each decade of life from the 20s to the 70s were included in this study. Cervical canal anteroposterior diameters at C5 midvertebral level on X-rays, and the prevalence of spinal cord compression (SCC) and increased signal intensity (ISI) changes on MRI were evaluated. Receiver operating characteristic analysis was performed to determine the cut-off value of the severity of canal stenosis resulting in SCC.
Results
NCC (<14 mm) was observed in 123 (10.2 %) subjects. SCC and ISI were found in 64 (5.3 %) and 28 (2.3 %) subjects, respectively. The prevalence of NCC was significantly higher in females and older subjects, but the occurrence of severe NCC (<12 mm) did not increase with age. The canal size in subjects with SCC or ISI was significantly smaller than in those without SCC (p < 0.0001). The cut-off values of cervical canal stenosis resulting in SCC were 14.8 and 13.9 mm in males and females, respectively.
Conclusions
The prevalence of NCC was considerably lower among asymptomatic healthy volunteers; the cervical canal diameter in subjects with SCC or ISI was significantly smaller than in asymptomatic subjects; NCC is a risk factor for SCC.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Degenerative cervical myelopathy (DCM) is one of the most common causes of spinal cord dysfunction in adults, resulting in a progressive condition due to chronic compression of the cervical spinal cord [1, 2]. The pathophysiology of DCM involves both static factors, which are either acquired or caused by developmental cervical canal stenosis, and dynamic factors, which result from repetitive injuries to the cervical cord [3, 4]. Developmental canal stenosis has been defined as a cervical canal diameter of <12–13 mm [5–8]. Narrow cervical canal has been frequently suggested as a risk factor for later development of DCM [6–12]. Several reports revealed significant and frequent coincidences of narrow cervical canal in patients with DCM; [5, 12–14] Higo et al. reported that 82 % of the patients with DCM had narrow cervical canal [14].
There is little data, however, regarding the frequency of narrow cervical canal in healthy subjects. Prior to conducting the present study, we were unaware of whether narrow cervical canal was actually significantly higher in patients with DCM because we could not compare the frequencies of occurrence between healthy and symptomatic subjects. Although Nagata et al. reported the presence of a narrow cervical canal (<15 mm at C5 vertebral body level) in 57.4 % of males (183/319) and 76.7 % in females (491/640) in a large-scale study of Japanese, their data set did not exclude symptomatic subjects and did not have a balanced gender- or age-group distribution [15]. After their study had been completed, the following issues remained unresolved: (1) how often narrow cervical canal could be identified in asymptomatic subjects; (2) whether the prevalence differs in males and females; and (3) whether the prevalence increases with age. In addition, only a limited number of studies analyzed the severity of canal stenosis which could lead to spinal cord compression (SCC) based on magnetic resonance imaging (MRI) and/or the development of myelopathy.
The objectives of the present study were (1) to investigate the frequency and distribution of narrow cervical canal, and (2) to analyze the cut-off value of the degree of cervical bony canal stenosis developing into SCC, using X-ray and MRI imaging from a large cohort (>1200) of asymptomatic healthy volunteers.
Materials and methods
A total of 1230 subjects were recruited for cervical spine X-rays and MRI imaging between February 2006 and February 2008. The subjects were relatively healthy Japanese volunteers without neurological symptoms. We recruited the subjects using newspaper advertisements and posters hung in facilities that were associated with our facility. The exclusion criteria included a history of brain or spinal surgery, comorbid neurological disease (such as cerebral infarction or neuropathy), symptoms related to sensory or motor disorders (such as numbness, clumsiness, motor weakness, and gait disturbances), rheumatoid arthritis or other autoimmune diseases, or severe neck pain. We also excluded pregnant women, individuals who received workmen’s compensation, and those who presented with the symptoms after a motor vehicle accident. Subjects with other comorbidities (smoking, diabetes, hypertension, others) were included in this study. The Institutional Review Board approved this study, and each patient signed a written consent form.
All participants underwent imaging analysis by two spinal surgeons (F.K. and K.S.). The X-ray and MRI data from 1211 subjects were included in the analyses, after excluding 29 subjects with measurement difficulties resulting from artifacts (such as those due to motion or the presence of metals). There were approximately 100 volunteers representing each sex and decade of life (from the third to the eighth decades of life). There were 606 male subjects: 101 in their 20s, 104 in their 30s, 100 in their 40s, 99 in their 50s, 101 in their 60s, and 101 in their 70s. There were 605 female subjects: 100 in their 20s, 99 in their 30s, 100 in their 40s, 103 in their 50s, 103 in their 60s, and 100 in their 70s.
Lateral (neutral) X-rays of the cervical spine were taken with a distance of 1.5 m between the X-ray tube and the film for all subjects. A lateral (neutral) X-ray was taken while subjects were standing and facing forward. The anteroposterior (AP) diameter of the spinal canal was determined at vertebral level C2–C7 and each disc level from C2–C3 to C6–C7 [16].
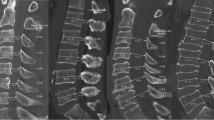
MRI scans were performed using a 1.5-Tesla superconductive magnet (Signa Horizon Excite HD version 12; GE Healthcare, UK). Scans were acquired at a slice thickness of 3 mm in the sagittal plane. T2-weighted images (fast spin echo TR, 3500 ms; TE, 102 ms) were acquired during sagittal scans. Axial scans were performed using T2-weighted images (fast spin echo TR, 4000 ms; TE, 102 ms). AP diameters of the dural sac and spinal cord and the cross-sectional area of the spinal cord were determined at each disc level from C2–C3 to C6–C7 [17]. All images were transferred to a computer as Digital Imaging and Communications in Medicine (DICOM) data to measure AP diameters and cross-sectional areas using imaging software (Osiris 4; Icestar Media Ltd, Essex, UK).
(The radiographical measurement methods used in this study have already been described in detail elsewhere [16, 17], and therefore will not be explained further here.)
Evaluation of cervical spinal cord compression
Cervical SCC was positively diagnosed when the AP diameter of the spinal canal at its narrowest was ≤ the AP diameter of the spinal cord at the mid C5 vertebral body level [18]. SCC was evaluated at each intervertebral level from C2–C3 to C7–T1.
Evaluation of increased signal intensity change (ISI) in the spinal cord
Increased signal intensity was defined based on sagittal T2-weighted images [19]: grade 0, none; grade 1, light (increased intensity, but less intense compared with cerebrospinal fluid signal); grade 2, intense (similar intensity to cerebrospinal fluid signal). Grades 1 and 2 signal intensity changes were included in this study.
Statistical analysis
Frequency distribution analysis was performed using Fisher’s exact test. Multiple comparison analysis was performed using analysis of variance (ANOVA) and Bonferroni post hoc tests. We used receiver operating characteristic (ROC) analysis to determine the cutoff values of cervical canal size resulting in SCC. A p value of <0.05 was considered to be statistically significant. All analyses were conducted using PRISM version 6 (GraphPad Software, San Diego, CA, USA).
Results
The mean canal AP diameter at the mid-C5 vertebral body level was 15.8 ± 1.5, 16.2 ± 1.5 and 15.4 ± 1.4 in all subjects (n = 1211), males alone (n = 606), and females alone (n = 605), respectively [16]. The data for cervical canal diameters at the other levels on X-ray for each subject were summarized in our previous paper [16]. Narrow cervical canals at mid-C5 vertebral body level (<14 mm in AP diameter) were observed in 123 subjects (10.2 %). AP diameters of <12 mm, 12–13 mm, and 13–14 mm were observed in 6 subjects (0.5 %), 29 subjects (2.4 %), and 88 subjects (7.3 %), respectively (Table 1). The majority of the subjects with narrow canal diameters (<14 mm) were female (68.3 %). This distribution with regard to gender was statistically significant (p < 0.0001), and the rate of occurrence in females was significantly higher in subjects with narrow cervical canals. The numbers of subjects with cervical narrow canals are listed by decade of life in Table 2. The frequency of narrow cervical canal (<14 mm) was significantly higher in the sixth and seventh decades than in the second decade (p < 0.0001), but the occurrence of severe narrow canal (<12 mm) was not found to increase with age.
SCC and ISI on T2-weighted MRI images were observed in 64 (5.3 %) and 28 subjects (2.3 %), respectively [18]. Cervical canal diameters at the mid-C5 vertebral body level were significantly different among subjects without SCC (15.87 ± 1.49), with SCC (14.60 ± 1.33) or with ISI (14.31 ± 1.02) [one way ANOVA, p < 0.0001 (Fig. 1)]. These canal diameters in patients with SCC or ISI were significantly narrower than in those without SCC (Bonferroni’s multiple comparison test; p < 0.0001), although significant differences were not observed between subjects with SCC and ISI.
To identify the cutoff value of cervical canal size which could result in SCC on MRI, we performed a gender-dependent ROC analysis. In males, 14.8 mm was the significant cutoff value [area under curve: 0.76, p < 0.0001 (Fig. 2a)], while 13.9 mm was the significant cutoff value for females [area under curve: 0.76, p < 0.0001 (Fig. 2b)].
Discussion
The current study represents the largest analysis yet undertaken of cervical X-rays and MRI images to determine the prevalence of narrow cervical canal in neurologically asymptomatic healthy subjects. Our findings indicated that the prevalence of narrow cervical canal (<14 mm) was considerably lower in asymptomatic subjects (10.2 %) than in symptomatic subjects. We also found narrow cervical canal to be more common in women and older subjects. In addition, cervical canal diameter was observed to be significantly narrower in patients with SCC or ISI, suggesting that narrow cervical canal diameter could be a risk factor for SCC and DCM.
Cervical bony canal size has been suspected to influence the occurrence of cervical myelopathy [6–12]. A normal sagittal AP diameter for the cervical spinal canal is approximately 17–18 mm between C3 and C7 on lateral X-rays [16, 20], and a cervical canal diameter of <12 or 13 mm has been defined as developmental canal stenosis [5–7]. A narrow cervical canal could predispose a person to possible SCC, particularly if there were disc protrusion and cervical alignment changes [4]. The prevalence of narrow cervical canal in DCM patients has been found to be high, with reported rates ranging from 19.8 to 82.0 % [5, 12–14].
There have been few reports regarding the prevalence of narrow cervical canal among healthy subjects. Higo et al. reported finding narrow cervical canal in 4 % of young asymptomatic people (seven out of 197 subjects) [21]. Nagata et al. performed a large-scale population-based cervical X-ray and MRI study of 959 Japanese subjects (319 men and 640 women; mean age, 66.4 years) which included both symptomatic and asymptomatic subjects, and reported that the prevalence of narrow cervical canal (<15 mm) in this mixed group was 70.3 % [15]. However, prior to the present study, there were no large-scale studies focusing specifically on neurologically asymptomatic subjects. To address this gap in our knowledge, we undertook the present study, which examined asymptomatic subjects from various age groups. We found narrow cervical canal to be present in only a minimal number of these subjects, a number that was smaller than those appearing in other reports [5, 12–15].
Our study of the prevalence of narrow cervical canal in asymptomatic subjects also investigated gender- and age-based differences in the prevalence of this condition. In their mixed study, Nagata et al. found that narrow cervical canal was much more common in females (76.7 %) than in males (57.4 %). In general, cervical canal diameter is significantly narrower in females [16], and the prevalence of canal stenosis could actually be greater in females for this reason. With respect to age-based differences in the prevalence of narrow cervical canal, there have only been a limited number of reports concerning healthy subjects. It was reported that older subjects have narrower cervical canal, [15, 16, 22] a finding confirmed in the present study, where the prevalence of narrow cervical canal (<14 mm) was indeed higher in older subjects. On the other hand, while the percentage of subjects with moderate canal stenosis (from 12 to 14 mm) was significantly higher in older subjects, the percentage of subjects with severe canal stenosis (<12 mm), which puts them at risk of developing cervical myelopathy (as described below), was not observed to increase with age. This might be due to the fact that older subjects with severe narrow cervical canal might become symptomatic, resulting in their exclusion from this study.
Prior to this study, it was unclear how narrow the cervical canal would have to be to constitute a risk factor for SCC on MRI or for developing myelopathy. Wolf et al. reported that a cervical canal <10 mm is a risk factor for developing myelopathy [23]. Edward et al. reviewed 63 patients’ cervical X-rays and reported that patients with cervical canal diameters <10 mm are more likely to have myelopathy [9]. Patients with diameters ranging from 10 to 13 mm were considered to be in premyelopathic condition. Other researchers reported that patients with developmental cervical spinal canal stenosis of ≤12 mm are highly likely to develop cervical myelopathy [7, 8]. In the current study, a cervical canal diameter <14.8 mm in men and 13.9 mm in women was considered a risk factor for SCC on MRI. Then, it was hypothesized that subjects with cervical canals <12 mm were at high risk for cervical myelopathy, and the subjects with diameters from 12 to 15 mm (in males) and from 12 to 14 mm (in females) were in a premyelopathic state for SCC as shown on MRI.
There are some limitations to this study. First, our survey was limited to Japanese subjects, and so possible ethnic differences were not considered. Second, we enrolled only asymptomatic subjects, which could have resulted in a selection bias when determining the cutoff value used to diagnose SCC. (This cutoff value is limited to only those cases with SCC observed on MRI; the value might have been lower if the study had included symptomatic patients.) Third, we compared different individuals in the different age groups, because this was a cross-sectional rather than a longitudinal study. Longitudinal studies would be required to determine whether young subjects with developmental canal stenosis could develop SCC at a future time and to determine the relationship between developmental canal stenosis and DCM.
In conclusion, this large cross-sectional analysis of cervical X-rays and MRIs in asymptomatic subjects demonstrated that the prevalence of narrow cervical canal in an asymptomatic population was considerably lower than in patients with DCM focused on in past reports. The percentage of subjects with narrow cervical canals was significantly higher among females and older subjects, but the prevalence of severe narrow cervical canal (<12 mm) was not observed to increase with age. According to MRI images, the diameters of cervical canals were significantly narrower in subjects with SCC or ISI. It appears that a narrow cervical bony canal size could be a risk factor for DCM.
References
Kalsi-Ryan S, Karadimas SK, Fehlings MG (2013) Cervical spondylotic myelopathy the clinical phenomenon and the current pathobiology of an increasingly prevalent and devastating disorder. Neuroscientist 19:409–421
Nouri A, Tetreault L, Singh A, Karadimas SK, Fehlings MG (2015) Degenerative cervical myelopathy: epidemiology, genetics and pathogenesis. Spine (Phila Pa 1976). doi:10.1097/brs.0000000000000913
Baptiste DC, Fehlings MG (2006) Pathophysiology of cervical myelopathy. Spine J Off J N Am Spine Soc 6:190s–197s. doi:10.1016/j.spinee.2006.04.024
Karadimas SK, Erwin WM, Ely CG, Dettori JR, Fehlings MG (2013) The pathophysiology and natural history of cervical spondylotic myelopathy. Spine 38(22 Suppl 1):S21–S36
Kasai Y, Akeda K, Uchida A (2007) Physical characteristics of patients with developmental cervical spinal canal stenosis. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 16:901–903. doi:10.1007/s00586-007-0358-2
Hayashi H, Okada K, Hamada M, Tada K, Ueno R (1987) Etiologic factors of myelopathy. A radiographic evaluation of the aging changes in the cervical spine. Clin Orthop Relat Res (214):200–209
Inoue H, Ohmori K, Takatsu T, Teramoto T, Ishida Y, Suzuki K (1996) Morphological analysis of the cervical spinal canal, dural tube and spinal cord in normal individuals using CT myelography. Neuroradiology 38:148–151
Sasaki T, Kadoya S, Iizuka H (1998) Roentgenological study of the sagittal diameter of the cervical spinal canal in normal adult Japanese. Neurol Med Chir (Tokyo) 38:83–88 discussion 88–89
Edwards WC, LaROCCA H (1983) The developmental segmental sagittal diameter of the cervical spinal canal in patients with cervical spondylosis. Spine 8:20–27
Torg JS, Naranja RJ Jr, Pavlov H, Galinat BJ, Warren R, Stine RA (1996) The relationship of developmental narrowing of the cervical spinal canal to reversible and irreversible injury of the cervical spinal cord in football players. J Bone Jt Surg Am 78:1308–1314
Gore DR (2001) Roentgenographic findings in the cervical spine in asymptomatic persons: a 10-year follow-up. Spine (Phila Pa 1976) 26:2463–2466
Morishita Y, Naito M, Hymanson H, Miyazaki M, Wu G, Wang JC (2009) The relationship between the cervical spinal canal diameter and the pathological changes in the cervical spine. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 18:877–883. doi:10.1007/s00586-009-0968-y
Shigematsu H, Ueda Y, Koizumi M, Takeshima T, Tanaka Y, Satoh N, Matsumori H, Oshima T, Matsuyama E, Kugai A, Takakura Y (2008) Does developmental canal stenosis influence surgical results of bilateral open-door laminoplasty for cervical spondylotic myelopathy? J Neurosurg Spine 9:358–362. doi:10.3171/spi.2008.9.10.358
Higo M (1987) Roentgenological study of anterior–posterior diameter in developmental canal stenosis of cervical spine. Nihon Seikeigeka Gakkai Zasshi 61:455–465
Nagata K, Yoshimura N, Hashizume H, Muraki S, Ishimoto Y, Yamada H, Takiguchi N, Nakagawa Y, Minamide A, Oka H (2014) The prevalence of cervical myelopathy among subjects with narrow cervical spinal canal in a population-based magnetic resonance imaging study: the Wakayama Spine Study. Spine J 14:2811–2817
Yukawa Y, Kato F, Suda K, Yamagata M, Ueta T (2012) Age-related changes in osseous anatomy, alignment, and range of motion of the cervical spine. Part I: radiographic data from over 1200 asymptomatic subjects. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 21:1492–1498. doi:10.1007/s00586-012-2167-5
Kato F, Yukawa Y, Suda K, Yamagata M, Ueta T (2012) Normal morphology, age-related changes and abnormal findings of the cervical spine. Part II: magnetic resonance imaging of over 1200 asymptomatic subjects. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 21:1499–1507. doi:10.1007/s00586-012-2176-4
Nakashima H, Yukawa Y, Suda K, Yamagata M, Ueta T, Kato F (2015) Abnormal findings on magnetic resonance images of the cervical spines in 1211 asymptomatic subjects. Spine 40:392–398
Yukawa Y, Kato F, Yoshihara H, Yanase M, Ito K (2007) MR T2 image classification in cervical compression myelopathy: predictor of surgical outcomes. Spine 32:1675–1678
Murone I (1974) The importance of the sagittal diameters of the cervical spinal canal in relation to spondylosis and myelopathy. J Bone Jt Surg Br 56:30–36
Higo M, Sakou T, Suzuki Y, Matsumoto R, Ito H, Kosakura H (1984) Roentogenologicalstudyoftheantero-posteriordiameter in cervical developmental canal stenosis [in Japanese]. Rinsho Seikei Geka 19:361–366
Goto S-I, Umehara J, Aizawa T, Kokubun S (2010) Comparison of cervical spinal canal diameter between younger and elder generations of Japanese. J Orthop Sci 15:97–103
Wolf BS, Khilnani M, Malis L (1956) The sagittal diameter of the bony cervical spinal canal and its significance in cervical spondylosis. J Mt Sinai Hosp N Y 23:283–292
Acknowledgments
This study was supported by institutional funds and by grant research funds, which are intended for promoting hospital functions, of the Japan Labor Health and Welfare Organization (Kawasaki, Japan).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Disclosure of funding
No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Rights and permissions
About this article
Cite this article
Nakashima, H., Yukawa, Y., Suda, K. et al. Narrow cervical canal in 1211 asymptomatic healthy subjects: the relationship with spinal cord compression on MRI. Eur Spine J 25, 2149–2154 (2016). https://doi.org/10.1007/s00586-016-4608-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4608-z