Abstract
Purpose
The lateral approach for anterior interbody fusion allows placement of a large footprint intervertebral spacer to indirectly decompress the neural elements through disc height restoration and resultant soft tissue changes. However, it is not well understood under what circumstances indirect decompression in lateral approach surgery is sufficient. This report aimed to evaluate clinical scenarios where indirect decompression was and was not sufficient in symptom resolution when using lateral interbody fusion.
Methods
A prospective study was undertaken of 122 consecutive patients treated with lateral interbody fusion without direct decompression. Pre- and postoperative symptomatology was assessed to evaluate the extent of neural decompression following implantation with a lateral polyetheretherketone spacer. Failure to improve or resolve preoperative radicular pain was considered a failure of indirect decompression and indicated these patients for additional posterior decompressive surgery.
Results
Unplanned second stage decompression was required in 11 patients. Of these patients, 7/11 early in this series had pathology that was underappreciated including spondylolisthesis from high grade facet arthropathy with instability (3), bony lateral recess stenosis (3) and both spondylolisthesis/stenosis (1). Three patients had iatrogenic leg pain through cage misplacement. There was one failure of indirect decompression that could not be explained through retrospective analysis of the patient’s record.
Conclusion
Indirect decompression clearly has a role in minimizing the amount of surgery that is required. However, it is important to consider the circumstances where this technique may be effective and preoperative considerations that may improve patient selection.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Spinal stenosis causing neurogenic claudication and radiculopathy results from either soft or calcified tissue compromise of the spinal canal, neural foramen, or both [1]. Traditionally direct decompression of the effected structures with or without fusion was the best available treatment [2, 3], but this involved significant disruption to the posterior elements [4]. Anterior column reconstruction with indirect decompression of the neural elements is now a standard and common procedure [5, 6]. One method of minimally invasive anterior column reconstruction is interbody fusion through a lateral transpsoas approach [7]. The indications and relative contraindications for this approach and procedure have become better established and understood through a significant body of clinical evidence [8–13]. There are also several reports supporting the ability of lateral interbody fusion to indirectly decompress the relevant neural structures and relieve neurogenic symptoms in selected patients [14, 15]. The clinical success of indirect decompression is a multi-factorial phenomenon that cannot be predicted by radiographic anatomical restoration alone. Factors proposed to limit the effectiveness of indirect decompression include congenital stenosis, congenitally short pedicles, disc sequestration, significant facet arthropathy/osteophyte formation, calcified disc or posterior longitudinal ligament (PLL), compromise of the lateral recess, synovial cysts, and/or radicular symptoms unimproved with flexion [16].
As such, there is a paucity of evidence that guides preoperative decision-making, patient selection and successful resolution prediction of radiculopathy when using this procedure.
The aims of this study were to (1) assess the ability of lateral interbody fusion to affect neural decompression and symptom resolution in a relatively large patient sample; (2) provide case examples where indirect decompression failed and (3) provide guidelines for appropriate patient selection to achieve satisfactory clinical outcomes.
Materials and methods
A prospective cohort study was undertaken of 122 consecutive patients undergoing extreme lateral interbody fusion (XLIF®, NuVasive, Inc. San Diego, CA) without direct decompression performed by a single surgeon (GM) between February 2011 and July 2013.
Patient demographics
Baseline patient information included demographics, medical comorbidities, and the primary diagnosis for surgery. Treatment information included levels treated, osteobiologics used, and requirement for supplemental posterior instrumentation. Patient-reported outcomes included back and leg pain [visual analog scale (VAS)], disability [Oswestry Disability Index (ODI)] and quality of life [SF-36 physical and mental component scores (PCS and MCS)]. The clinical and radiographic outcomes were recorded by an independent research assistant (RP).
XLIF procedure
The XLIF procedure has previously been described [7] and involves a 90° off-midline mini-open retroperitoneal approach to the anterior lumbar spine through the fibers of the psoas muscle to the lateral border of the disc space. Passage through the psoas muscle is guided through the use of a neuromonitoring system (NV JJB™/M5®, NuVasive, Inc.) that is integrated into approach and procedural instrumentation to protect nerves of the lumbar plexus [17, 18]. Once the lateral disc has been accessed, standard surgical techniques are used. The discectomy was undertaken first through an ipsilateral annulus incision, Cobb elevator release of contralateral annulus and then careful clearance of cartilaginous tissue from the endplates with curettes and rasps. The nerve roots were not directly visualized.
All patients were fitted with a 10° lordotic intervertebral polyetheretherketone (PEEK) cage (CoRoent®, NuVasive, Inc.). The cages were 50, 55 or 60 mm in length (lateral dimension), 18 or 22 mm in width (anterior-posterior), and 8, 10 or 12 mm in height (inferior–superior). Cages were filled with either Infuse or Attrax. Infuse® (Medtronic, Inc. Memphis, TN) is rhBMP-2 applied to an Absorbable Collagen Sponge (ACS) (Medtronic, Inc.). The Infuse was prepared at a fixed concentration of 1.5 mg/cc, with the ACS trimmed to the required cage volume. The Infuse dose is volume dependent, i.e. internal graft volume of cage equalled Infuse volume in cc [19]. No Infuse was placed outside the cage. AttraX (NuVasive, Inc.) is an osteoinductive synthetic bone putty comprised of 95 % β-TCP (tricalcium phosphate) and 5 % hydroxyapatite.
Supplemental posterior fixation was indicated for patients with facet arthropathy, degenerative or isthmic spondylolisthesis and reduced bone density [14].
Indirect decompression
A failure of indirect decompression was defined as a patient requiring additional unplanned intervention for persisting or new onset radicular leg pain less than 6 months postoperative (to avoid misdiagnosis with pseudoarthrosis). Revision surgery was indicated if patients failed conservative management, including physical therapy, pain medication and epidural injections.
Interbody fusion
Computed tomography (CT) scans were performed on high definition (HD) CT (Somatom Definition Flash, Siemens AG, Erlangen, Germany) preoperatively, 2 days postoperatively to assess cage position and instrumentation, and then at 6 and 12 months until confirmation of solid interbody fusion was obtained on coronal and sagittal views. Patients not fused by 12 months receive a 24 or 36-month scan, depending on progression of interbody fusion. Fusion was defined as the presence of bridging interbody trabecular bone [20]. An independent radiologist (CB) from within the treating institution evaluated the CT scans.
Statistical analysis
Statistical analysis was carried out using IBM SPSS Statistics (Version 21.0, IBM Corp., Armonk, NY, USA) and included paired t tests, independent samples t tests and Fisher’s exact tests with statistical significance measured at P < 0.05.
Results
All 122 patients treated with XLIF were followed for a minimum of 12 months (mean 22.7; range 12–36 months). The mean age of patient cohort was 62.9 years (27–86) and 83 (68.0 %) were female. Forty-four (36.1 %) patients had prior lumbar surgery. A total of 169 levels were treated with a mean of 1.4 levels per patient (range 1–3 levels). PEEK interbody cages filled with either rhBMP-2 (79.5 %) or Attrax (20.5 %) were implanted in the treated disc spaces. Percutaneous posterior fixation was used in 64 (52.5 %) patients. A summary of the patient demographic and treatment information is provided in Table 1.
Overall mean back and leg pain improved from 6.7 to 3.2 and 6.4 to 2.6, representing 48.9 and 48.2 % improvements, respectively. ODI improved from 52.7 to 30.5 (41.7 %), with PCS and MCS improving 38.9 % (29.0–40.1) and 8.8 % (45.2–49.5), respectively. All outcome measures had a statistically significant improvement from baseline [P < 0.0001, except MCS (P = 0.0011)]. The outcome measures are provided in Table 2.
The overall fusion rate, confirmed on HD CT coronal and sagittal views, progressed from 28.7 % at 6 months, to 69.7 % at 12 months and 94.3 % at 24 months (Table 3).
Unplanned second stage decompression was required in only 11 (9.0 %) patients (Table 4). Of these patients, 7/11 early in this series had pathology that was underappreciated including spondylolisthesis from high grade facet arthropathy with instability (3/11 patients), bony lateral recess stenosis (3/11 patients) and 1 patient with both degenerative unstable spondylolisthesis/stenosis. Three more patients had iatrogenic leg pain through cage misplacement. There was only one failure of indirect decompression that could not be explained through retrospective analysis of the patient’s record.
Case examples where indirect decompression failed
Case study 1: Missed bony lateral recess stenosis
A 60-year-old male presented with 6 months of worsening leg pain worse with walking and standing, relieved by sitting. Lower extremity exam showed no neurological deficits with normal pulses. CT showed L2/3 central and lateral recess stenosis with facet arthropathy (Fig. 1). No response to physical therapy and epidural injections was observed. The patient subsequently underwent an L2/3 XLIF with posterior fixation. Persistent leg pain postoperatively was non-responsive to further epidural injections. Thus, the surgeon proceeded to perform a L2/3 posterior decompression 3 weeks postoperatively with successful relief of bilateral leg pain.
Case study 2: Degenerative spondylolisthesis/instability
A 59-year-old male presented with 18 months of low back pain and bilateral leg pain. CT revealed L4/5 degenerative anterolisthesis with canal stenosis (Fig. 2a). No response to physical therapy and epidural injections was observed. The patient underwent an L4/5 standalone XLIF. The patient presented 2 weeks postoperatively with severe low back pain and left lower limb pain, exacerbated by flexion despite adequate restoration of disc height (Fig. 2b). The surgeon proceeded to perform an L4/5 posterior instrumented decompression and fusion 3 months after failure of conservative management with marked improvement in both back and leg pain postoperatively.
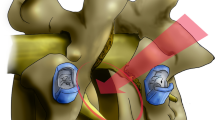
Case study 3: Misaligned cage
A 67-year-old female presented with 4 months of worsening back and right >left leg pain. Lower extremity exam showed no neurological deficits with normal pulses. CT revealed an L2/3 degenerative disc with facet arthropathy. No response to physical therapy and epidural injections. The patient underwent an L3/4 XLIF with posterior fixation. Severe new onset contralateral left L3 radiculopathy was observed postoperatively with CT showing a posteriorly misaligned interbody cage encroaching on the left L3/4 exiting foramen (Fig. 3). The surgeon proceeded to perform a left L2/3 posterior foraminotomy with incomplete relief of left leg pain.
Case study 4: Idiopathic radiculopathy
A 62-year-old female presented to the clinic with 6 months of severe low back pain and left L3 radiculopathy. CT showed a large left L3/4 extra-foraminal disc prolapse (Fig. 4a). No response to physical therapy and epidural injections was seen. Nerve conduction studies (NCS) found left L3 active denervation. The patient subsequently underwent an L3/4 standalone XLIF with satisfactory foraminal decompression (Fig. 4b). Persistent left L3 radiculopathy postoperatively with repeat NCS showing incomplete reinnervation. No response to epidural injections or direct decompression with left L3/4 far lateral microdiscectomy and rhizolysis of left L3 nerve root was seen. The patient required ongoing pregabalin for persisting neuropathic left leg pain. It is questionable whether this is a failure of indirect decompression or chronic intrinsic nerve root damage that decompression, direct or otherwise, would be unable to resolve.
Discussion
Lateral interbody fusion has an extensive body of literature supporting its general efficacy [8–13]. However, as is the case with every form of spinal fusion surgery, treatment for varied pathologies and indications has the potential to have a relatively different effect on symptom resolution and outcome improvement magnitude. Radiographic studies have shown significant increases in foraminal area between 26 and 35 % [21, 22], dural sac area up to 143 % [23] and posterior disc height in 13–20 % [16, 21]. Numerically these values of radiographic improvement are impressive; however, experience shows that there is a range of both radiographic and clinical outcomes. In theory, a greater degree of indirect decompression should correlate with a greater degree of clinical improvement, though this is not always the case. Some patients may improve clinically with only minimal indirect decompression where others have a large indirect decompression without clinical resolution. This may be due to anatomical needs and individual pathology, where predictability is not able to be achieved in all cases. In general, the indirect decompression afforded by interbody fusion is sufficient to resolve symptoms in selected patients. This has been shown by the relief of back and leg pain by lateral interbody fusion, even in the absence of direct decompressive surgery [15, 23].
The technique of lateral interbody fusion intentionally spares the anterior longitudinal ligament (ALL), posterior longitudinal ligament (PLL) and anterior and posterior regions of the annulus. As a result of the laterally implanted interbody cage, with dimensions similar to those of traditional ALIF implants, anatomical vertebral body alignment is restored through ligamentotaxis [23, 24]. The distraction of the vertebral endplates via this application of an axial tensioning force enabled proportional restoration of neural foramen dimensions [16].
In this study, we aimed to determine the clinical success rate of indirect decompression by following a carefully selected cohort of patients that, according to the treatment protocols of the senior author, should have benefited from lateral interbody fusion without direct decompression [14]. As such a failure of indirect direct decompression was defined as the patient requiring unplanned second stage decompressive surgery for persisting or new onset radicular leg pain originating at the index level less than 6 months postoperatively. The unresolved radicular leg pain was initially treated conservatively with physical therapy, medications and epidural steroid injections and a failure of this management protocol was required before surgery was indicated.
There were 9 % (11/122) of patients who ultimately required an unplanned decompression. Retrospective analysis of the case notes demonstrated that revision surgery was required for missed unstable spondylolisthesis (3/11 patients), bony lateral recess stenosis (3/11 patients), both unstable spondylolisthesis/stenosis (1/11 patients), misaligned cages resulting in contralateral foraminal encroachment (3/11 patients) and one case (1/11 patients) where no cause could be attributed.
In review, failure due to instability only occurred early in the series and represented part of the learning curve described by the author [10]. This experience shows that unstable spondylolistheses may not always be adequately indirectly decompressed. Although it is not an absolute requirement to decompress patients with spondylolisthesis, it may be helpful to evaluate the extent of instability preoperatively. The grade of facet arthropathy (with CT and bone scans) [25] and the degree of stenosis on flexion are important indicators. Preoperative attention to axial magnetic resonance imaging and CT may be able to provide information on the extent of bony lateral recess stenosis and guide decision-making as to whether or not an indirect decompression would be successful. The failures due to bony lateral recess stenosis occurred throughout the series and represent an attempt to minimize surgery with the expectation that occasionally this pathology may require a subsequent direct decompression. The preoperative indicators for when this will be required remain unknown. Misaligned cages reinforce the imperative need for the surgeon to remain orthogonal to the spine. While the idiopathic neuropathy is most likely related to the chronicity of the pathology, it highlights that some patients cannot be cured by surgery alone.
Conclusion
Indirect decompression clearly has a role in minimizing the amount of surgery that is required. However, it is important to consider the circumstances where this technique may be effective and preoperative considerations that may improve patient selection. Patients with neurogenic claudication and radiculopathy from spinal canal and foraminal stenosis can be successfully treated with lateral interbody fusion. Patients with leg pain due to bony lateral recess stenosis or unstable degenerative spondylolisthesis may benefit from being treated with lateral interbody fusion follwed by second stage posterior direct decompression and fixation.
References
Lurie JD, Tosteson AN, Tosteson TD et al (2008) Reliability of readings of magnetic resonance imaging features of lumbar spinal stenosis. Spine 33:1605–1610
Weinstein JN, Tosteson TD, Lurie JD et al (2008) Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med 358:794–810
Smorgick Y, Park DK, Baker KC et al (2013) Single- versus multilevel fusion for single-level degenerative spondylolisthesis and multilevel lumbar stenosis: four-year results of the spine patient outcomes research trial. Spine 38:797–805
Burkus JK, Gornet MF, Dickman CA, Zdeblick TA (2002) Anterior lumbar interbody fusion using rhBMP-2 with tapered interbody cages. J Spinal Disord Tech 15:337–349
Than KD, Wang AC, Rahman SU et al (2011) Complication avoidance and management in anterior lumbar interbody fusion. Neurosurg Focus 31:E6
Arnold PM, Anderson KK, McGuire RA Jr (2011) The lateral transpsoas approach to the lumbar and thoracic spine: a review. Surg Neurol Int 3:S198–S215
Ozgur BM, Aryan HE, Pimenta L, Taylor WR (2006) Extreme lateral interbody fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J 6:435–443
Isaacs RE, Hyde J, Goodrich JA, Rodgers WB, Phillips FM (2010) A prospective, nonrandomized, multicenter evaluation of the extreme lateral interbody fusion for the treatment of adult degenerative scoliosis: perioperative outcomes and complications. Spine 35:S322–S330
Rodgers WB, Gerber EJ, Patterson J (2011) Intraoperative and early postoperative complications in extreme lateral interbody fusion: an analysis of 600 cases. Spine 36:26–32
Malham GM, Ellis NJ, Parker RM, Seex KA (2012) Clinical outcome and fusion rates after the first 30 extreme lateral interbody fusions. Sci World J 2012:246989. doi:10.1100/2012/246989
Berjano P, Balsano M, Burie J, Petruzzi M, Lamartina C (2012) Direct lateral access lumbar and thoracolumbar fusion: preliminary results. Eur Spine J 21:S37–S42
Berjano P, Lamartina C (2013) Far lateral approaches (XLIF) in adult scoliosis. Eur Spine J 22:S242–S253
Khajavi K, Shen AY (2014) Two-year radiographic and clinical outcomes of a minimally invasive, lateral, transpsoas approach for anterior lumbar interbody fusion in the treatment of adult degenerative scoliosis. Eur Spine J 23:1215–1223
Malham GM, Ellis NJ, Parker RM, Seex KA (2014) Maintenance of segmental lordosis and disc height in standalone and instrumented extreme lateral interbody fusion (XLIF). J Spinal Disord Tech. doi:10.1097/BSD.0b013e3182aa4c94
Alimi M, Hofstetter CP, Cong GT et al (2014) Radiological and clinical outcomes following extreme lateral interbody fusion. J Neurosurg Spine 20:623–635
Oliveira L, Marchi L, Coutinho E, Pimenta L (2010) A radiographic assessment of the ability of the extreme lateral interbody fusion procedure to indirectly decompress the neural elements. Spine 35:S331–S337
Uribe JS, Vale FL, Dakwar E (2010) Electromyographic monitoring and its anatomical implications in minimally invasive spine surgery. Spine 35:S368–S374
Tohmeh AG, Rodgers WB, Peterson MD (2011) Dynamically evoked, discrete-threshold electromyography in the extreme lateral interbody fusion approach. J Neurosurg Spine 14:31–37
Boden SD, Zdeblick TA, Sandhu HS, Heim SE (2000) The use of rhBMP-2 in interbody fusion cages. Definitive evidence of osteoinduction in humans: a preliminary report. Spine 25:376–381
Williams AL, Gornet MF, Burkus JK (2005) CT evaluation of lumbar interbody fusion: current concepts. AJNR Am J Neuroradiol 26:2057–2066
Malham GM, Parker RM, Goss B, Blecher CM, Ballok ZE (2014) Indirect foraminal decompression is independent of metabolically active fact arthropathy in extreme lateral interbody fusion. Spine 39:E1303–E1310
Kepler CK, Sharma AK, Huang RC et al (2012) Indirect foraminal decompression after lateral transpsoas interbody fusion. J Neurosurg Spine 16:329–333
Elowitz EH, Yanni DS, Chwajol M et al (2011) Evaluation of indirect decompression of the lumbar spinal canal following minimally invasive lateral transpsoas interbody fusion: radiographic and outcome analysis. Minim Invasive Neurosurg 54:201–206
Marchi L, Amaral R, Oliveira L et al (2012) Stand-alone lateral interbody fusion for the treatment of low-grade degenerative spondylolisthesis. Sci World J 2012:456346. doi:10.1100/2012/456346
Malham GM, Parker RM, Ballok ZE, Goss B, Diwan AD, Uribe JS (2014) Bone scans are reliable for the identification of lumbar disk and facet pathology. Glob Spine J. doi:10.1055/s-0034-1394298
Conflict of interest
No funds were received in support of this work. BG is employed by NuVasive Australia & NZ Pty Ltd. The authors have full control of all primary data and agree to allow the journal to review the data if requested.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Malham, G.M., Parker, R.M., Goss, B. et al. Clinical results and limitations of indirect decompression in spinal stenosis with laterally implanted interbody cages: results from a prospective cohort study. Eur Spine J 24 (Suppl 3), 339–345 (2015). https://doi.org/10.1007/s00586-015-3807-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-015-3807-3