Abstract
Purpose
Intervertebral disc degeneration related to postmenopausal osteoporosis is an important issue in spinal disorder research. This study aimed to investigate the effects of salmon calcitonin (sCT), as an antiresorptive medication, on lumbar intervertebral disc degeneration using a rat ovariectomy (OVX) model.
Methods
Thirty 3-month-old female Sprague–Dawley rats were randomly divided into three groups: the sham-operated (Sham) group and two ovariectomized groups treated with vehicle (OVX+V) or sCT (OVX+CT; 16 IU/kg, sc) on alternate days for 6 months. Treatment began after OVX and continued for 6 months. At the end of the experiment, bone mineral density (BMD), micro-CT analysis, biomechanical testing, histology, and immunohistochemistry were performed for all groups.
Results
Salmon calcitonin significantly maintained vertebrae BMD, percent bone volume, and biomechanical strength, when compared with the OVX+V group. The changes of mucoid degeneration in the nucleus pulposus and calcification in the middle cartilage endplate were more moderate in the OVX+CT group compared with the OVX+V group, and immunohistochemistry revealed a significant increase in aggrecan and type II collagen expressions, but marked reductions in matrix metalloproteinase (MMP)-1, MMP-3, and MMP-13 expressions in the OVX+CT group.
Conclusions
Salmon calcitonin treatment was effective in delaying the process of the disc degeneration in OVX rats. The underlying mechanisms may be related to preservation of structural integrity and function of vertebrae, and affecting extracellular matrix metabolism by modulating the expressions of MMPs, aggrecan and type II collagen to protect the disc from degeneration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As human life span increases so does the incidence of age-associated diseases, such as osteoporosis (OP), intervertebral disc degeneration (IDD), and osteoarthritis (OA), resulting in significant socioeconomic burden. IDD and OA are the most common underlying causes of joint-related chronic disability and debilitating pain in the elderly, especially in postmenopausal women. Current treatment methods are generally not effective and involve either symptomatic relief with nonsteroidal anti-inflammatory drugs and physical therapy, or surgery when conservative treatments fail.
To date, the precise pathogenesis and pathophysiology of IDD have been obscure. However, several evidences indicate that disc degeneration is associated with the disruption of intact spinal structure, including adjacent structures such as the vertebral body [1–4], which might result in imbalanced mechanical loading on the disc. Bone mineral density (BMD) assays in both pre- and postmenopausal women revealed a correlation between the value of BMD and disc height, suggesting that the vertebral structural change is closely related to the degree of disc degeneration, and the influences occurring to one structure may similarly influence others [5]. Previous studies showed that decreases in vertebral BMD, percent bone volume and biomechanical strength have a strong relationship with IDD in the rat model of ovariectomy (OVX), suggesting that measures to reduce osteoporotic changes might have inhibitory effects on disc degeneration [3, 6].
Salmon calcitonin (CT) is a physiologic modulator of osteoclast function and a well-established antiresorptive medication that has long been widely used in the treatment of metabolic bone diseases, such as osteoporosis, hypercalcemia, and Paget’s disease. Recent lines of evidence suggest that calcitonin acts on both osteoclasts and chondrocytes [7]. Sondergaard et al. [8, 9] showed that calcitonin could increase proteoglycan and counteract type II collagen degradation, and inhibit matrix metalloproteinase (MMP) expression and activity in articular chondrocytes. These results demonstrate the efficacy of sCT against osteoarthritis; however, little is known about the effect of sCT on spinal osteoarthritis, such as disc degeneration.
In this study, we hypothesize that sCT may be an alternative drug treatment for lumbar disc degeneration resulted to osteoporosis, although the underlying mechanisms about how sCT impacts the process of disc degeneration remain unclear. Thus, the purpose of this study is to investigate the effect of sCT on lumbar IDD in OVX rats.
Materials and methods
Experimental design
Three-month-old female Sprague–Dawley rats (Peking University Animal Center, Beijing, China) were randomly divided into three groups. All rats received either ovariectomy (OVX) or sham-operation (Sham). OVX rats were divided into two groups: vehicle treatment (OVX+V, n = 10) and sCT treatment (OVX+CT, n = 10).
Rats in the OVX+CT group received sCT (Novartis AG, Switzerland) treatment starting after surgery by subcutaneous injection at a dosage of 16 IU/kg, every other day for 6 months. The dose was effective in reducing bone turnover and partially preventing cancellous bone loss in the estrogen-depleted skeleton [10, 11]. Saline was given as a placebo to rats in the OVX+V group. All animals were sacrificed at 6 months postsurgery (9 months old). All experimental procedures were reviewed and approved by the Institutional Animal Care and Use Committee.
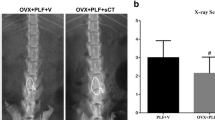
BMD analysis using dual energy X-ray absorptiometry
Segments L3–4 and L5–6 of each animal were removed, dissected free of muscle, and BMD measurements were performed on the anteroposterior plane by dual energy X-ray absorptiometry. This was performed using a densitometer (QDR Discovery, Hologic, Bedford, MA, USA) operating in high-resolution mode and specialized software for small animals supplied by the equipment’s manufacturer.
Micro-CT measurements
To investigate the effects of sCT in the trabeculae of the cancellous tissue of the L4 vertebral body, three-dimensional trabecular analysis was performed using a micro-CT system (SkyScan 1076, Aartselaar, Belgium). The micro-CT is equipped with a micro-focus X-ray tube, with a focal spot of 18 μm, producing a fan beam that is detected by a charge-coupled device array, with a turntable that can be shifted automatically in the axial direction. The energy and intensity are equal to 70 kVp and 140 μA, respectively. On the original three-dimensional images, morphometric indices were directly determined from the volume of interest (VOI), which was restricted to an inner cylinder with 1.5 mm diameter, and the height was taken below 1 mm between the bilateral growth plates, excluding the cortex. Cancellous micro-structure was characterized using standardized techniques to determine the percent bone volume (BV/TV), trabecular thickness (Tb.Th), trabecular number (Tb.N), trabecular separation (Tb.Sp), and structural model index (SMI).
Biomechanical testing
The mechanical strength of the lumbar vertebra (L4) was measured by compression testing using a mechanical strength analyzer (AG-IS, Shimadzu, Japan) [12]. In this test, the planoparallel surfaces were obtained by removing the cranial and caudal ends of the vertebral specimen, thereby allowing for a uniform compression test to be performed on individual vertebrae. From the vertebral body, a central cylinder with planoparallel ends and a height of approximately 5 mm was obtained. All compression tests were performed in the displacement-control mode at a crosshead speed of 0.5 mm/min to eliminate any strain rate effects. Maximum load, maximum stress, and yield stress were obtained from the compression tests of vertebral bodies.
Histological evaluation
After the rats were sacrificed, their lumbar spines (L5–6) were removed, fixed in 10 % buffered neutral formalin solution, decalcified in ethylenediaminetetraacetic acid, and embedded in paraffin. These blocks were cut into 5-µm-thick sections, and histological examination was performed using van Gieson (VG) stain. Morphometric analysis was performed using an image auto-analysis system (Olympus BX51, Japan).
The degenerative changes in the intervertebral discs were observed and the degrees of change in the stained sections were scored independently by an individual blind to the experimental protocol using the disc degeneration assessment scoring system (Table 1) described by Wang et al. [3].
Disc height and thickness of the cartilage endplate
Disc height measurements were taken from the cranial growth plate to the caudal growth plate in the histological samples. For each image, the height was determined by an average of three measurements made in three areas of the disc space: the left side, the center, and the right side [13]. The thickness of cartilage endplate was measured from the cranial growth plate to the border between the nucleus pulposus and the cartilage endplate in the histological samples. For each image, the thickness was determined by an average of 10 measurements made in the cartilage endplate. Histomorphometric assessment was performed using a digital image analysis system (Olympus BX51, Japan).
Immunohistochemistry
Tissue sections were deparaffinized in xylene, and rehydrated in a reverse-graded series of ethanol as usual. After antigen retrieval, quenching of endogenous peroxidase and blocking of nonspecific binding, sections were incubated overnight at 4 °C with either anti-rat MMP-1, MMP-3, MMP-13, type I collagen, type II collagen, type X collagen (1:100; all from Bioss Inc., Beijing, China) or aggrecan (1:100; ANBO Biotechnology Co., Ltd., San Francisco, CA, USA). The remaining procedures were performed according to the SA1066 SABC-FITC kit (Boster Corporation, Wuhan, China), and the color (brown) was developed by incubation in DAB (ZSGB-BIO Corporation, Beijing, China). The sections were counter stained with hematoxylin. Specimens were examined using an image analysis system (Olympus BX51).
Statistical analysis
All data were analyzed using SPSS15.0 software and results shown in tables are reported as mean ± SD. The statistical significance between groups was estimated using one-way analysis of variance (ANOVA) and Fisher’s protected least significant difference test. The results of histological scores were analyzed using a nonparametric test of Kruskal–Wallis. P < 0.05 was considered statistically significant.
Results
Bone mineral density and micro-CT parameters of the lumbar vertebral body
At 6 months postsurgery, the BMD of the lumbar segments (L3–4 and L5–6) in the OVX+V group was significantly decreased compared with the Sham group (P < 0.05) (Table 2), and the BMD of the OVX+CT group was significantly higher than the OVX+V group (P < 0.05). The L4 of each group was also analyzed with regard to the three-dimensional trabecular micro-architecture. Figure 1 shows representative three-dimensional reconstructed micro-CT images of the vertebral trabecular bone of the VOI from each group. Quantification of three-dimensional trabecular structures revealed that BV/TV and Tb.N in the OVX+V group was significantly decreased compared with the Sham group (P < 0.05), and Tb.Sp was higher in the OVX+V group than in the Sham group (P < 0.05) (Table 3). The BV/TV and Tb.N in the OVX+CT group are significantly higher than their counterparts in the OVX+V group (P < 0.05). Meanwhile, the Tb.Sp was markedly lower in the OVX+CT group than in the OVX+V group (P < 0.05). There was no significant difference in Tb.Th and SMI among the three groups (P > 0.05).
Mechanical testing of the lumbar vertebral body
The L4 of each rat was also analyzed for strength by determining the maximal compressive load in Newtons (N) each bone could sustain before structural failure. Figure 2 shows the bone mechanical properties obtained from lumbar compression. Compared with the Sham group, the values of maximum load, maximum stress, and yield stress were significantly decreased in the OVX+V group (P < 0.05). However, the values of maximum load, maximum stress, and yield stress were significantly higher in the OVX+CT group than in the OVX+V group at 6 months postsurgery (P < 0.05), suggesting that sCT could effectively maintain the biomechanical strength of the vertebrae.
Histological findings
The intervertebral discs between L5 and L6 were normal in the Sham group at the 6 months postsurgery. The nucleus pulposus contained abundant notochordal cells, surrounded by large zones of extracellular matrix, and the cartilage endplates were hyaline cartilage composed of chondrocytes (Fig. 3). In the OVX+V group, discs showed degenerative changes, where the nucleus pulposus appeared reduced in size relative to the Sham group and comprised relatively few clustered doublets of chondrocyte-like cells. Mucoid degeneration could also be seen eroding the nucleus pulposus, with clefts forming within. An increased number of small chondrocytes appeared in the inner layer of the annulus fibrosus, which was present in the form of fibers invading the nucleus pulposus. Bony tissues that contained bone marrow, hematopoietic lineage cells and mineralized bone became more obvious in the deep zone of the middle cartilage endplate. In contrast, the morphology in the OVX+CT group did not show obvious changes; there was no significant difference in the number of notochordal cells, there were only a few chondrocyte-like cells in the nucleus pulposus, and some small chondrocytes were observed in the inner layer of the annulus fibrosus. Mild mucoid degeneration was observed in some samples in the OVX+CT group and there were no bony tissues formed in the middle cartilage endplate.
Histologic illustration of L5–6 segments of lumbar spine at 6 months after operation. a van Gieson staining of the L5–6 segments of lumbar spine (×3.2). b The degenerative changes of the nucleus pulposus and the inner layer of the annulus fibrosus stained by van Gieson (×20). Arrow indicates the nucleus pulposus underwent mucoid degeneration. Arrowhead indicates doublets of chondrocyte-like cells appeared within the nucleus pulposus. c van Gieson staining of the middle cartilage endplate (×40). VP vertebral physis, CEP cartilage endplate, B bony tissues
The histological score of the discs in the OVX+V group was significantly higher than the Sham group (P < 0.05) (Fig. 4) and the histological score of the discs in the OVX+CT group was lower than the OVX+V group (P > 0.05).
Disc height and thickness of the cartilage endplate
At 6 months postsurgery, histomorphometric analysis revealed that the disc height in the OVX+V group was significantly decreased compared with the Sham group (P < 0.05) (Fig. 5a). Both the cartilage endplate thickness and the bony tissue area within the cartilage endplate, especially in the middle cartilage endplate, were markedly increased in the OVX+V group when compared with the Sham group (Fig. 5b, c). The disc height in the OVX+CT group was significantly higher than the OVX+V group (P < 0.05), but there was no significant difference between the OVX+CT and Sham groups. The thickness of the cartilage endplate and the bony tissue area of the cartilage endplate in the OVX+CT group were both significantly decreased when compared with the OVX+V group (P < 0.05).
Histomorphometric assessment of intervertebral discs among the three groups at 6 months after operation. a Histomorphometric assessment of disc height, b histomorphometric assessment of the thickness of cartilage endplate, c histomorphometric assessment of newly formed bony tissue in the cartilage endplate. Values are the mean ± SD of ten rats. *P < 0.05 vs. Sham group; # P < 0.05 vs. OVX+V group
Immunohistochemistry
Immunohistochemical analysis of the Sham group revealed strong immunostaining for aggrecan and type II collagen in the nucleus pulposus (Fig. 6). In the OVX+V group, because the notochordal cells were replaced by some chondrocyte-like cells, the density of aggrecan and type II collagen staining in the OVX+V group was markedly decreased compared with the Sham group. However, much stronger immunostaining was observed for aggrecan and type II collagen in the OVX+CT group compared with the OVX+V group. Weak immunostaining for MMP-1, MMP-3, and MMP-13 were observed in the Sham group, and stronger immunostaining could be observed in chondrocyte-like cells in the OVX+V group. In the OVX+CT group, immunostaining for MMP-1, MMP-3, and MMP-13 were much weaker than in the OVX+V group.
Immunohistochemistry assay for a aggrecan, b type II collagen, c MMP-1, d MMP-3, and e MMP-13 in the nucleus pulposus among the three groups (×40). Immunohistochemical analysis showed that the protein levels of aggrecan and type II collagen in the OVX+V group were much weaker than that in the Sham and OVX+CT groups, and MMP-1-, MMP-3-, and MMP-13-positive staining in the nucleus pulposus were stronger in the OVX+V group than in the Sham and OVX+CT groups
The IOD value of MMP-1-, MMP-3-, and MMP-13-positive cells in the annulus fibrosus was significantly higher in the OVX+V group than that in the Sham group (P < 0.05) (Fig. 7). The IOD values of type II and type I collagens were significantly lower and higher, respectively, in the OVX+V group compared with the Sham group (P < 0.05). However, the IOD values of MMP-1, MMP-3, and MMP-13 were significantly lower in the OVX+CT group compared with the OVX+V group (P < 0.05), and the IOD values for type II and type I collagens were significantly higher and lower, respectively (P < 0.05).
Immunohistochemistry assay for a MMP-1, b MMP-3, c MMP-13, d type I collagen and e type II collagen in the annulus fibrosus among the three groups (×40). MMP-1-, MMP-3-, MMP-13-, and type I collagen-positive staining in the annulus fibrosus were stronger in the OVX+V group than in the Sham and OVX+CT groups, and type II collagen-positive staining in the annulus fibrosus was much weaker in the OVX+V group than that in the Sham and OVX+CT groups *P < 0.05 vs. Sham group; # P < 0.05 vs. OVX+V group
Expression of type X collagen was also evaluated in the cartilage endplate. The chondrocytes in the middle cartilage endplate were stained more strongly positive for type X collagen in the OVX+V group than in Sham group, but stained milder in the OVX+CT group than that in OVX+V group (Fig. 8).
Discussion
Previous studies have largely focused on the effects of sCT on the physiology and pathology of osteoporotic bone; however, this study is the first to investigate the effect of sCT on IDD in OVX rats. We have previously shown in the OVX model of osteoporosis in rats, histological evidence demonstrating that estrogen deficiency induced by OVX accelerated vertebral body bone loss, concomitantly causing degeneration of lumbar intervertebral discs. In this study, the administration of sCT could preserve the structural integrity and biomechanical properties of the vertebrae, preventing abnormal stress loading on the discs. In contrast, sCT could also effectively modulate extracellular matrix metabolism, such as inhibiting the expression of MMPs, maintaining type II collagen and aggrecan expression, thereby helping sustain the biological characteristics of the intervertebral disc.
The mechanical interaction between the disc and vertebra has been examined in a number of studies. The normal disc acts as a fluid-filled cushion that distributes stress or load evenly across the vertebral endplate. Compression under normal circumstances creates pressures in the nucleus, leading to compressive stresses at the center of the endplate and tension at the periphery where the annulus fibers attach, suggesting a relationship between the intervertebral disc and vertebral body bone [14]. The mechanical loading and structural integrity of vertebrae might play an important role in the progression of disc degeneration, whereby aberrant loading can give rise to localized tissue injury [15]. Amling et al. [16] found that in osteoporotic subjects, the selective loss of structural elements reduced the load-bearing capacities of the vertebrae. Well-connected trabeculae are much more resistant to bending and buckling than those with reduced reinforcement orthogonal to the loading axis. Morphological changes in the vertebral bone may be a reason for disc degeneration [17]. The changes of vertebral body trabecular bone architecture may modulate the mechanical loading of the disc. Osteoporosis in an OVX setting can result in weakened vertebrae with lower BMD, which decreases the loading strength and consequently affects disc metabolism. This has been confirmed in a human study revealing that a decrease in intervertebral disc height is strongly related to menopause [18, 19]. As described earlier in the literature review, osteoporosis can lead to a concentration of stress on the center of the vertebral endplate. Biomechanical modeling has shown that increased compressive stress can lead to axial endplate bulge and compression of the trabecular bone. Indeed, the estrogenic milieu may be relevant because of the significant impact on the hydrophilic glycosaminoglycans, the water content, collagen and elastin of the intervertebral discs, suggesting that the endocrine and metabolic changes are related to disc degeneration [20, 21].
The intervertebral disc is an avascular tissue, and poor disc nutrition may be a major contributor to disc degeneration. It has been reported that the survival of disc cells can be affected by limited nutrient availability [11]. Deteriorated disc cells have a reduced capacity to synthesize aggrecan and type II collagen, leading to the dehydration of the nucleus pulposus with severe consequences for both the biological and biomechanical stability of the disc [22]. Using MR-based perfusion imaging, it has been shown that in elderly subjects as the vertebral BMD decreases, the vertebral body bone marrow perfusion also decreases [23, 24]. Because the disc nucleus obtains nutrients partially by means of diffusion from the endplate, it is feasible that decreased blood perfusion in the osteoporotic vertebral body in postmenopausal women significantly contributes to decreased diffusion and nutrient supply to the intervertebral disc nucleus, which might be another factor involved in disc degeneration in OVX rats.
Salmon calcitonin has potent antiresorptive effects directly acting on osteoclasts, and is widely used in the management of postmenopausal osteoporosis, Paget’s disease, and malignancy-associated hypercalcemia. Consistently, we found that sCT effectively inhibited OVX-induced vertebral bone loss using BMD assays, which was further confirmed by micro-CT of the micro-architecture of the vertebrae and maintenance of the BV/TV, Tb.N, and Tb.Sp parameters. In accordance with the structural characteristics, sCT administration also provided better biomechanical performance of adjacent vertebral bodies than the OVX+V group. Therefore, sCT protection of the disc function and structure might be a result of maintenance of function and structural integrity of the vertebrae.
The cartilage endplate plays an important role in preservation of the structural integrity and function of the disc. The cartilage endplate served as the main route of nutrient supply into the nucleus [25], where calcification and blocking of the endplate route may lead to loss of nutrient supply closely associated with disc degeneration [26, 27]. Increased calcification of the cartilage endplate could lead to changes to the nutritional pathway of the disc, with subsequent endplate-bone remodeling that affect the flow of solutes to and from the intervertebral disc. It is possible that the apparent disc degeneration observed in the OVX+V group in this study is due to changes in the nutritional pathway, although further investigation is required to test this hypothesis. In the current study, the cartilage endplate in the OVX+V group showed increased thickness and increased bony tissues, which might be associated with abnormal loading and poor nutritional supply. In contrast, the cartilage endplate in the OVX+CT group exhibited less degenerative changes, which was accompanied by thinner cartilage and less bony tissues, which might facilitate the maintenance of the normal loading and nutrient supply beneficial to the disc function and structure. We also found significantly increased expression of type X collagen in the cartilage endplate in the OVX+V group, which could be produced by hypertrophic chondrocytes during endochondral ossification and matrix calcification. Furthermore, sCT administration effectively decreased the expression of type X collagen.
Up to now, the exact pathogenesis of disc degeneration remains unknown, but the biologically mediated and mechanically induced disc degeneration is conceptualized to be a consequence of metabolic molecular changes in a dynamic structure of extracellular matrix. Molecules in the discs are continually being broken down by proteinases, such as the MMPs and aggrecanases [24, 28–30]. Some increases in degradation products in the discs associated with MMP activity were observed with advancing degenerative grade [28, 31]. The balance of matrix macromolecules determines the quality and integrity of the matrix, and thus the mechanical behavior of the disc itself. The most significant biochemical change to occur in disc degeneration is the loss of proteoglycan [32]. Aggrecan is a large proteoglycan that forms macromolecular aggregates with hyaluronic acid via an interaction that is stabilized by a linker protein. Aggrecan molecules are degraded as result of the loss of glycosaminoglycans, which causes a drop in the osmotic pressure of the disc matrix and thus a loss in hydration. Several collagen types are present in the disc, and they form a fibrous network that holds cells and proteoglycans in the matrix. Type II collagen is the most abundant collagen in the disc, and its content is crucial for proper disc function [19]. It is well known that type II collagen can be degraded by MMPs. Collagenases, such as MMP-1 (collagenase 1, interstitial collagenase), MMP-8 (neutrophil collagenase), and MMP-13 (collagenase 3), appear to be of particular importance as they can cleave intact triple-helical structure of type II collagen, while MMP-3 is capable of degrading proteoglycan, fibronectin, laminin, and the nonfibrillar collagens, activating other pro-MMPs, including MMP (-1, -8, -9, and -13) [33, 34]. In addition, it is reported that calcitonin receptors are found on articular chondrocytes and that calcitonin can inhibit MMP-mediated type II collagen degradation in ex vivo articular cartilage explants [9]. In addition, it was reported that sCT can increase the synthesis of proteoglycans and collagen type II, and decrease proteolytic and metalloproteinase activities [8, 9]. Our study showed that the mechanism of sCT protection against OVX-induced disc degeneration is via the effective inhibition of MMP-1, MMP-3, and MMP-13 expressions while sustaining aggrecan and type II collagen expressions.
There are some limitations of this study that should be taken into consideration. The nucleus pulposus of rats is populated with notochordal cells, which are not observed in the human intervertebral disc. However, the rat IDD model has been commonly used in many basic studies. Rats have been used as models in the study of IDD, in particular the mechanics of the intervertebral disc in relation to human IDD. Previous studies have shown that annulus injury can induce significant and progressive biochemical and molecular changes in the murine intervertebral disc. These studies have implied that the process of IDD induced by annulus puncture shares some similarities with human IDD. Another limitation is that the degenerative induction in this study is not physiologic, because the intervertebral discs of the rat are not affected with weight bearing. However, OVX is a simple and technically easy method of inducing IDD. This method is frequently used in many studies and can lead to IDD [3, 6]. Consequently, estrogen deficiency and long-term experimental duration applied to the rat lumbar intervertebral disc in this study produced morphological, biochemical, and structural changes representative of mild degeneration, as well as accelerate degenerative changes in very specific manners that may interact with other risk factors of degeneration, including nutrition, genetics, and aging.
In conclusion, this study sheds new light on the preventive effects of sCT on IDD, clearly showing that sCT can slow the progression of disc degeneration. The underlying mechanisms might be related to preservation of the structural integrity and function of the vertebrae, which is essential for maintaining disc function. sCT also affects extracellular matrix metabolism by modulating the expressions of MMPs, aggrecan and type I/II collagen to protect the disc from degeneration. While sCT may not be able to restore disc degeneration, it should be able to retard its progression and thus delay the need for more aggressive surgical intervention.
References
Benneker LM, Heini PF, Alini M, Anderson SE, Ito K (2005) 2004 Young Investigator Award Winner: vertebral endplate marrow contact channel occlusions and intervertebral disc degeneration. Spine (Phila Pa 1976) 30:167–173 (00007632-200501150-00002[pii])
Wang Y, Battie MC, Boyd SK, Videman T (2011) The osseous endplates in lumbar vertebrae: thickness, bone mineral density and their associations with age and disk degeneration. Bone 48:804–809. doi:10.1016/j.bone.2010.12.005
Wang T, Zhang L, Huang C, Cheng AG, Dang GT (2004) Relationship between osteopenia and lumbar intervertebral disc degeneration in ovariectomized rats. Calcif Tissue Int 75:205–213. doi:10.1007/s00223-004-0240-8
Homminga J, Aquarius R, Bulsink VE, Jansen CT, Verdonschot N (2012) Can vertebral density changes be explained by intervertebral disc degeneration? Med Eng Phys 34:453–458. doi:10.1016/j.medengphy.2011.08.003
Baron YM, Brincat MP, Calleja-Agius J, Calleja N (2009) Intervertebral disc height correlates with vertebral body T-scores in premenopausal and postmenopausal women. Menopause Int 15:58–62. doi:10.1258/mi.2009.009013
Luo Y, Zhang L, Wang WY, Hu QF, Song HP, Su YL, Zhang YZ (2013) Alendronate retards the progression of lumbar intervertebral disc degeneration in ovariectomized rats. Bone 55:439–448. doi:10.1016/j.bone.2013.03.002
Karsdal MA, Sondergaard BC, Arnold M, Christiansen C (2007) Calcitonin affects both bone and cartilage: a dual action treatment for osteoarthritis? Ann N Y Acad Sci 1117:181–195. doi:10.1196/annals.1402.041
Sondergaard BC, Madsen SH, Segovia-Silvestre T, Paulsen SJ, Christiansen T, Pedersen C, Bay-Jensen AC, Karsdal MA (2010) Investigation of the direct effects of salmon calcitonin on human osteoarthritic chondrocytes. BMC Musculoskelet Disord 11:62. doi:10.1186/1471-2474-11-62
Sondergaard BC, Wulf H, Henriksen K, Schaller S, Oestergaard S, Qvist P, Tanko LB, Bagger YZ, Christiansen C, Karsdal MA (2006) Calcitonin directly attenuates collagen type II degradation by inhibition of matrix metalloproteinase expression and activity in articular chondrocytes. Osteoarthr Cartil 14:759–768. doi:10.1016/j.joca.2006.01.014
Li M, Shen Y, Burton KW, DeLuca PP, Mehta RC, Baumann BD, Wronski TJ (1996) A comparison of the skeletal effects of intermittent and continuous administration of calcitonin in ovariectomized rats. Bone 18:375–380. doi:10.1016/8756-3282(96)00014-2
Shen Y, Li M, Wronski TJ (1997) Calcitonin provides complete protection against cancellous bone loss in the femoral neck of ovariectomized rats. Calcif Tissue Int 60:457–461
Mosekilde L, Danielsen CC, Knudsen UB (1993) The effect of aging and ovariectomy on the vertebral bone mass and biomechanical properties of mature rats. Bone 14:1–6
Allon AA, Aurouer N, Yoo BB, Liebenberg EC, Buser Z, Lotz JC (2010) Structured coculture of stem cells and disc cells prevent disc degeneration in a rat model. Spine J 10:1089–1097. doi:10.1016/j.spinee.2010.09.014
Keller TS, Hansson TH, Abram AC, Spengler DM, Panjabi MM (1989) Regional variations in the compressive properties of lumbar vertebral trabeculae. Effects of disc degeneration. Spine (Phila Pa 1976) 14:1012–1019
Stokes IA, Iatridis JC (2004) Mechanical conditions that accelerate intervertebral disc degeneration: overload versus immobilization. Spine (Phila Pa 1976) 29:2724–2732 (00007632-200412010-00016[pii])
Pugh JW, Rose RM, Radin EL (1973) Elastic and viscoelastic properties of trabecular bone: dependence on structure. J Biomech 6:475–485
Suri P, Miyakoshi A, Hunter DJ, Jarvik JG, Rainville J, Guermazi A, Li L, Katz JN (2011) Does lumbar spinal degeneration begin with the anterior structures? A study of the observed epidemiology in a community-based population. BMC Musculoskelet Disord 12:202. doi:10.1186/1471-2474-12-202
Sornay-Rendu E, Munoz F, Duboeuf F, Delmas PD (2004) Disc space narrowing is associated with an increased vertebral fracture risk in postmenopausal women: the OFELY Study. J Bone Miner Res 19:1994–1999. doi:10.1359/JBMR.040904
Garnero P, Sornay-Rendu E, Arlot M, Christiansen C, Delmas PD (2004) Association between spine disc degeneration and type II collagen degradation in postmenopausal women: the OFELY study. Arthritis Rheum 50:3137–3144. doi:10.1002/art.20493
Muscat Baron Y, Brincat MP, Galea R, Calleja N (2007) Low intervertebral disc height in postmenopausal women with osteoporotic vertebral fractures compared to hormone-treated and untreated postmenopausal women and premenopausal women without fractures. Climacteric 10:314–319. doi:10.1080/13697130701460640
Baron YM, Brincat MP, Galea R, Calleja N (2005) Intervertebral disc height in treated and untreated overweight post-menopausal women. Hum Reprod 20:3566–3570. doi:10.1093/humrep/dei251
Chung SA, Wei AQ, DE Connor, Webb GC, Molloy T, Pajic M, Diwan AD (2007) Nucleus pulposus cellular longevity by telomerase gene therapy. Spine (Phila Pa 1976) 32:1188–1196. doi:10.1097/BRS.0b013e31805471a3
Griffith JF, Yeung DK, Antonio GE, Lee FK, Hong AW, Wong SY, Lau EM, Leung PC (2005) Vertebral bone mineral density, marrow perfusion, and fat content in healthy men and men with osteoporosis: dynamic contrast-enhanced MR imaging and MR spectroscopy. Radiology 236:945–951. doi:10.1148/radiol.2363041425
Griffith JF, Yeung DK, Tsang PH, Choi KC, Kwok TC, Ahuja AT, Leung KS, Leung PC (2008) Compromised bone marrow perfusion in osteoporosis. J Bone Miner Res 23:1068–1075. doi:10.1359/jbmr.080233
Urban JP, Smith S, Fairbank JC (2004) Nutrition of the intervertebral disc. Spine (Phila Pa 1976 29:2700–2709 (00007632-200412010-00014 [pii])
Holm S, Holm AK, Ekstrom L, Karladani A, Hansson T (2004) Experimental disc degeneration due to endplate injury. J Spinal Disord Tech 17:64–71 00024720-200402000-00012[pii]
Turgut M, Uslu S, Uysal A, Yurtseven ME, Ustun H (2003) Changes in vascularity of cartilage endplate of degenerated intervertebral discs in response to melatonin administration in rats. Neurosurg Rev 26:133–138
Sztrolovics R, Alini M, Roughley PJ, Mort JS (1997) Aggrecan degradation in human intervertebral disc and articular cartilage. Biochem J 326(Pt 1):235–241
Weiler C, Nerlich AG, Zipperer J, Bachmeier BE, Boos N (2002) 2002 SSE Award Competition in Basic Science: expression of major matrix metalloproteinases is associated with intervertebral disc degradation and resorption. Eur Spine J 11:308–320. doi:10.1007/s00586-002-0472-0
Roberts S, Caterson B, Menage J, Evans EH, Jaffray DC, Eisenstein SM (2000) Matrix metalloproteinases and aggrecanase: their role in disorders of the human intervertebral disc. Spine (Phila Pa 1976) 25:3005–3013
Patel KP, Sandy JD, Akeda K, Miyamoto K, Chujo T, An HS, Masuda K (2007) Aggrecanases and aggrecanase-generated fragments in the human intervertebral disc at early and advanced stages of disc degeneration. Spine (Phila Pa 1976) 32:2596–2603. doi:10.1097/BRS.0b013e318158cb85
Inkinen RI, Lammi MJ, Lehmonen S, Puustjarvi K, Kaapa E, Tammi MI (1998) Relative increase of biglycan and decorin and altered chondroitin sulfate epitopes in the degenerating human intervertebral disc. J Rheumatol 25:506–514
Lauer-Fields JL, Tuzinski KA, Shimokawa K, Nagase H, Fields GB (2000) Hydrolysis of triple-helical collagen peptide models by matrix metalloproteinases. J Biol Chem 275:13282–13290 (275/18/13282[pii])
Le Maitre CL, Freemont AJ, Hoyland JA (2004) Localization of degradative enzymes and their inhibitors in the degenerate human intervertebral disc. J Pathol 204:47–54. doi:10.1002/path.1608
Acknowledgments
The authors thank Dr. Hong Xu for technical assistance with animal procedures and histological analysis, Yan-Li Zhu for help with dual energy X-ray absorptiometry scanning. This work was partly supported by National Natural Science Foundation of China (No. 31171136), and Natural Science Foundation of Hebei province (No. H2013209257).
Conflict of interest
The authors have no actual or potential conflict of interests including any financial, personal, or other relationships with other people or organizations that could inappropriately influence, or be perceived to influence, this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Luo, Y., Zhang, L., Wang, WY. et al. The inhibitory effect of salmon calcitonin on intervertebral disc degeneration in an ovariectomized rat model. Eur Spine J 24, 1691–1701 (2015). https://doi.org/10.1007/s00586-014-3611-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-014-3611-5