Abstract
Purpose
Lumbar intervertebral disc degeneration is a common cause of lower back pain that affects the physical and mental health of patients and increases social burden. Parathyroid hormone has been reported to be effective at inhibiting disc degeneration; however, these effects have not been fully established in vivo in ovariectomized (OVX) rats. Thus, in this study, we aimed to address this issue and examine the effects of parathyroid hormone treatment in OVX rats.
Methods
Thirty female Sprague-Dawley rats, three months-old, were subjected to sham or ovariectomy surgery. Twelve weeks postsurgery, OVX rats were treated with either human parathyroid hormone [hPTH(1–34), 30 μg/kg/day] or vehicle (normal saline (NS)) treatment. The L3–6 spinal segments were harvested after 12 weeks treatment. Bone mineral density (BMD), micro-architectural parameters, and biomechanical assessment were measured at the lumbar vertebral bodies. Histology and immunohistochemistry were performed to analyze the characteristics of the lumbar intervertebral discs.
Results
OVX + PTH rats had significantly higher BMD, percentage bone volume density, trabecular thickness, and biomechanical strength compared with those in Sham and OVX + NS rats. Histology and immunostaining revealed that disc degeneration was not significantly different between the OVX + NS rats and the OVX + PTH rats, compared with the Sham group; the structure of nucleus pulposus was disordered, the expression of collagen I was increased, and collagen II and aggrecan were decreased.
Conclusions
These findings confirmed that hPTH(1–34) treatment has substantial anabolic effects on bone mass and trabecular micro-architecture, while the excessively enhanced bone mass and strength were coupled with a non-significant effect on the disc degeneration in ovariectomized rats.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lower back pain (LBP) affects nearly 60% of the people by the age of 70 years [1]. Although the aetiology of LBP is still unclear, it has been proved to be closely related with intervertebral disc degeneration. Aging is one of the main culprits of intervertebral disc degeneration. Previous study evidenced a higher degenerative discs prevalence with increasing age [2]. Osteoporosis, a systemic skeletal disorder, is also an common age-related disease characterized by decreased bone mass and micro-architectural deterioration, with consequently increasing bone fragility and susceptibility to fracture. An estimated 200 million people suffer from osteoporosis worldwide [3]. Postmenopausal osteoporosis as a most common type, It is about 30% of all postmenopausal women suffer from osteoporosis in Europe and America [4]. A correlation study, performed in premenopausal and postmenopausal women, revealed that the bone mineral density (BMD) of the lumbar vertebrae is positively associated with disc degeneration [5]. In contrast, Fabreguet et al. [6] showed that in osteoporotic men, the lumbar spine degeneration prevalence is also high. Another study indicated that oestrogen deficiency may accelerate disc degeneration in postmenopausal women [7]. Our previous studies revealed the positive association between oestrogen deficiency-induced osteopenia and disc degeneration in ovariectomized (OVX) rat, the most widely used animal model mimicking the postmenopausal osteoporosis in women, and intervention with alendronate or salmon calcitonin could not only prevent bone loss but also inhibit intervertebral disc degeneration [8,9,10]. These contradictive results indicate that any change in bone metabolism that impacts bone mass and micro-structure may destroy the micro-environment, thus inducing degeneration of the intervertebral disc.
These previous studies indicate that an effective intervention would not only prevent decreased bone mass but also inhibit disc degeneration induced by oestrogen deficiency. Madiraju et al. recently discovered that PTH(1–34), as a drug-treated osteoporosis [11], could protect the intervertebral disc from degeneration by stimulating collagen II synthesis and suppressing calcification markers (alkaline phosphatase (ALP), Ca2+, and inorganic phosphate (Pi)) in vitro in degenerated disc cells via both PKA and MAPK signaling pathways [12]. However, it remains unclear whether PTH(1–34) could prevent intervertebral disc degeneration in vivo in OVX rats.
Based on these considerations, we hypothesize that hPTH(1–34) might not only stimulate bone formation in vertebrae but also retard intervertebral disc degeneration in OVX rats. We therefore performed the present study, to test this hypothesis by detecting the bone mass, micro-structure, and biomechanical properties of the vertebrae using BMD, micro-computed tomography (micro-CT), and compression testing and on intervertebral disc degeneration by histology and immunohistochemistry (IHC) analysis in OVX rats.
Materials and methods
Experimental design
Thirty female three month-old Sprague-Dawley (SD) rats, with an average weight of 264 ± 12 g, were housed at the Experimental Animal Center of North China University of Science and Technology in a 12-hour light/dark cycle, the temperature was 22 ± 2 °C. All the rats were healthy throughout the study. All experimental procedures were reviewed and approved by the Institutional Animal Care and Use Committee.
Rats were randomly assigned to three groups of ten rats: Sham group (ablated a piece of fat around the ovary), OVX + NS and OVX + PTH group received bilateral ovariectomy. Twelve weeks post-operation, the OVX rats in the OVX + PTH group were treated for 12 weeks with the subcutaneous injection of 30 μg/kg/day of hPTH(1–34) (Sigma Chemical Co., USA) for 12 consecutive weeks. Based on previous studies [13, 14], the dose selected was effectively preventing bone loss in OVX rats. Normal saline as a placebo was given to rats of the OVX + NS group. According to the body weight, the total treatment dose was adjusted weekly.
Bone mineral measurements
Bone mineral content (BMC) and bone mineral density of L3–4 and L5–6 were measured by dual energy X-ray absorptiometry (QDR Discovery, Hologic, Bedford, MA, USA). The equipment manufacturer supplied specialized software for small animals.
Micro-CT measurements
Bone mass and micro-architecture of the L3 vertebral bodies were detected by using SkyScan 1076micro-CT (SkyScan, Aartselaar, Belgium), with a resolution of 18 μm per voxel. The intensity and energy are equal to 140 μA and 70 kVp, respectively. The volume of interest (VOI) was restricted to an inner cylinder with 3-mm length and 1.5-mm diameter, excluding the cortex. From the binarized images, the 3D morphometric parameters for the bone mass and micro-structure, such as relative bone volume (Bone volume over total volume (BV/TV)), trabecular number (The inverse of the mean distance between the mid-axes of the structure, Tb.N), thickness (Tb.Th), and separation (The average separation between the mid-axes is calculated, Tb.Sp) and the structural model index (For an ideal plate and rod structure, the structure model index (SMI) value is 0 and 3, respectively, independent of the physical dimensions. For a structure with both plates and rods of equal thickness, the value lies between 0 and 3, depending on the volume ratio of rods and plates, SMI) were calculated.
Lumbar compression test
The mechanical property of the lumbar vertebra (L4) was measured by compression test, by using a mechanical analyzer (AG-IS, Shimadzu, Japan). Before the test, soft tissues and intervertebral discs were carefully removed, and the vertebral body was shaped as a cylinder with the heights of approximately 5 mm, and the vertebral cross-sectional area was also calculated by the ratio of vertebral volume/vertebral height. The compression tests were performed in the displacement-control mode at a crosshead speed of 0.5 mm/min. The 3D biomechanical parameters of the vertebral bodies, such as maximum load, maximum stress, yield load, and yield stress, were obtained from compression tests. Yield stress and maximum stress were obtained as the division of yield load and maximum load by the cross-sectional area of the vertebrae, respectively. Elastic modulus was calculated by the formula KL/A based on the data of stiffness (K, the slope of load-deformation curve in elastic region), length (L, the height of vertebral body test specimen), and area (A) of the vertebrae.
Histology and immunohistochemistry
The paravertebral muscles and the posterior columns of the L5–6 segments were completely removed. Then, fixed with neutral-buffered 10% formalin for 24 hours, and decalcified for three to four weeks, the tissues were embedded in paraffin and mid-sagittally sectioned (5 μm). Finally, the sections were stained with van Gieson (VG). The histological characters of the intervertebral disc from each group animals were observed and scored independently by an individual blind to the experimental protocol according to the scoring system for the disc degeneration evaluation [8].
The level and distribution of protein expression such as aggrecan, collagen I (Col-I), and collagen II (Col-II) were performed by immunohistochemical staining. Sections were incubated 12 hours at 4 °C with either anti-rat aggrecan (1:100; ANBO Biotechnology Co., Ltd., SF, USA), Col-I, or Col-II (1:100; all from Bioss Inc., Beijing, China). According to the test kit (SA1066 SABC-FITC, Boster Corporation, Wuhan, China), the subsequently procedures were performed and the color (brown) was developed by incubation in DAB (ZSGB-BIO Corporation. Beijing, China) and finally counter-stained with haematoxylin.
Statistical analysis
All data were analyzed by using the SPSS 15.0 software and expressed as the mean ± standard deviation (SD). A one-way ANOVA and a post hoc test Fisher’s protected least were performed to compare the statistical difference between groups. P values less than 0.05 was considered to be statistically significant difference.
Results
Body weight and BMD measurements
The body weights had no significant difference at baseline and increased over time in all groups, but body weights in the OVX + NS and OVX + PTH groups increased significantly throughout the study compared with the Sham group (P < 0.05), with no markedly difference between the OVX + NS and the OVX + PTH groups. Notably, hPTH (1–34) did not affect the body weight of rats during the 12 weeks of treatment (Fig. 1).
Twelve weeks after commencing treatment, the BMD and BMC of the L3–4 and L5–6 segments in the OVX + NS group were significantly decreased compared with the Sham group (P < 0.05) (Table 1), and the those of the OVX + PTH group were markedly higher compared with the OVX + NS group (P < 0.05). It is worth noting that hPTH (1–34) significantly increased the BMD and BMC of the lumbar vertebrae compared with the Sham group (P < 0.05).
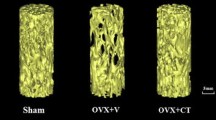
Micro-computed tomography parameters of the lumbar vertebral body
The 3D trabecular micro-architecture of the L3 lumbar vertebra of each group was analyzed by micro-CT. Figure 2 shows representative 3D-reconstructed images of the volume of interest (VOI) of the vertebral trabecular bone from each group. The quantification of 3D trabecular structures revealed that, compared with the Sham group, bone volume density (BV/TV) and trabecular number (Tb.N) were significantly decreased, and trabecular spacing (Tb.Sp) was higher in the OVX + NS group (P < 0.05) (Table 2). The BV/TV, trabecular thickness (Tb.Th), and Tb.N in the OVX + PTH group were significantly higher compared with those in the OVX + NS group (P < 0.05). Meanwhile, the Tb.Sp and SMI were significantly lower in the OVX + PTH group than in the OVX + NS group (P < 0.05).
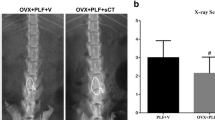
Mechanical testing of the lumbar vertebral body
The L4 of each rat was also analyzed for strength by determining the maximal compressive load in Newton’s (N) that each bone could sustain before structural failure. Figure 3 shows the bone mechanical properties obtained from lumbar compression. The values of maximum load and yield load were significantly decreased in the OVX + V group than in the Sham group (P < 0.05); however, the values of maximum load, maximum stress, yield load, and yield stress were significantly higher in the OVX + PTH group than in the OVX + NS group (P < 0.05), suggesting that hPTH (1–34) could effectively increase the biomechanical strength of the vertebrae.
Histological findings
To examine the effect of hPTH (1–34) on the disc matrix, discs were subjected to histology using van Gieson stain. The Sham group displayed normal-looking discs, an intact annulus fibrosus (AF) with a normal pattern of fibrocartilage lamellas, a well-defined border between the nucleus pulposus (NP) and the AF, and preserved proteoglycan content (Fig. 4). In the OVX + NS group, the histological sections showed signs of severe degeneration, whereas the NP appeared reduced in size relative to Sham group, and there comprised, numerous clustered, doublets of chondrocyte-like cells were present, and mucoid degeneration were also be seen. In the OVX + PTH group, the nucleus pulposus also showed degenerative changes, which consisted of abundant doublets of chondrocyte-like cells, but a few of notochordal cells could be observed remaining in the nucleus pulposus (Fig. 4).
The histological score of the discs in the OVX + NS group was markedly higher than the Sham group (P < 0.05) (Fig. 5); however, there was no significant change in the OVX + PTH group compared with the OVX + NS group (P > 0.05).
Immunohistochemical analysis
In the Sham group, immunohistochemistry study of the nucleus pulposus revealed strong immunostaining for aggrecan and Col-II (Fig. 6). Because abundant chondrocyte-like cells replaced the notochordal cells in the OVX + NS group, the density of aggrecan and Col-II staining was markedly decreased compared with the Sham group. However, there were no significant differences in immunostaining for aggrecan and Col-II between the OVX + PTH and the OVX + NS groups.
Additionally, immunostaining showed significantly higher levels Col-I and lower levels of Col-II in the AF in the OVX + PTH group compared with the Sham group (Fig. 7).
Immunohistochemistry assay for type I collagen and type II collagen in the annulus fibrosus among the three groups (×200). Type I collagen and type II collagen-positive staining in the annulus fibrosus were weaker and stronger in the Sham group than in the OVX + NS and OVX + PTH groups, respectively
Discussion
While many previous studies have reported the effects of hPTH (1–34) on the osteoporotic bone, there is little information available on its involvement in the control of disc degeneration. The present study is the first to evaluate the effect of hPTH (1–34) on intervertebral disc degeneration in OVX rats. Our data demonstrated that hPTH (1–34) may reconstruct the micro-architecture and preserve the biomechanical properties of the vertebrae with excessive enhanced bone mass and strength; however, no significant effect was observed on the inhibition of disc degeneration in OVX rats.
PTH peptides have been used clinically as osteoanabolic therapies for osteoporosis and fracture prevention. PTH inhibits the apoptosis of osteoblasts and increases osteoblast production rate, thereby increase mass, as well as improve bone micro-architecture and enhance bone strength [15]. Consistently, our results demonstrated that hPTH (1–34) effectively inhibited vertebral bone loss of OVX rats by BMD assays, and the micro-architecture of the vertebrae was also further confirmed by micro-CT. In accordance with the structural characteristics, the hPTH (1–34) administration provided better biomechanical performance of adjacent vertebral bodies than what occurred in the OVX + NS group. hPTH (1–34) also induced an almost threefold increase in maximal load compared with the OVX + NS group. The increases observed in Tb.V, Tb.Th, and Tb.N and the decrease in Tb.Sp were remarkable in the OVX + PTH group compared with the other groups. As an anabolic agent, hPTH(1–34) can effectively improve trabecular micro-architecture, which can induce greater bone formation than its effects on bone resorption. Previous studies also reported that hPTH(1–34) can noticeably improve bone micro-architecture as measured by micro-CT, including those in humans [16, 17].
The disruption of disc nutrition may contribute majorly to disc degeneration [18]. Previous study proved that disc cells may fail to survive with limited nutrient availability [19]. Deteriorated disc cells have decreased capacity for the synthesis of extracellular matrix including aggrecan and collagen II, which leads to dehydration of NP with subsequent degeneration [20]. It was found that vertebral body bone marrow perfusion also decreased as vertebral BMD decreased in elderly subjects [21, 22]. Because the disc partially obtains nutrients from the endplate by diffusion, it is feasible that decreased blood perfusion of vertebral body in postmenopausal women, to a great extent, contributes to decreased diffusion and nutrient supply to the intervertebral disc nucleus. It is possible that there is a balance between the vertebral bone mass and the vertebral body bone marrow perfusion. Once the balance is disturbed, the nutrient supply to the disc may decrease, followed by an increase or decrease in bone mass.
It is interesting to note that hPTH (1–34)-treated rats showed significant higher bone mass and strength than both OVX + NS and Sham rats. Although the relationship between osteopenia and disc degeneration is still debatable, there are a number of hypotheses. OVX has been proposed to induce bone loss resulting in intervertebral disc degeneration. Furthermore, as BMD of the vertebrae is positively related to disc degeneration, higher BMD of the vertebral body is associated with more severe adjacent disc degeneration, and lower lumbar spine BMD is associated with less severe disc degeneration [23, 24]. Therefore, we deduced that excessive increased vertebral body bone mass and strength could lead to decreased perfusion of the vertebral body bone marrow, with a subsequent decrease in nutrient supply to the disc. In turn, this could prevent hPTH (1–34) from inhibiting disc degeneration, although further investigation is required to confirm this hypothesis. In our previous study, PTH(1–34), using same dosage as the present study, but a shorten period (8 weeks), effectively improved lumbar fusion and alleviated adjacent segment disc degeneration in OVX lumbar fusion rats [25]. Therefore, the dosage and intervention period are promised to be the key points that decide whether the PTH(1–34) could act dual roles of promoting bone formation and ameliorating disc degeneration.
Interveterbral disc obtains many types of collagen which form a fibrous network that holds proteoglycans and cells in the matrix. The major collagen in the disc is collagen II, which content is crucial for proper disc function. Aggrecan is a large proteoglycan and functionally important component of the intervertebral disc [26]. In this study, immunohistological analyses demonstrated that the amount of aggrecan and collagen II in the NP were higher in the Sham group than in the OVX + NS and OVX + PTH groups after three months of treatment. These findings indicate that hPTH (1–34) could not reconstitute the content of collagen II and aggrecan, resulting in no significant differences between the OVX + PTH and the OVX + NS group.
There are several limitations in this study. First, the NP of rats are different from human NP, in which is not populated with the notochordal cells; however, the rat disc degeneration model has been widely used in several animal studies. In particular, rat models of disc degeneration have been used to examine how the mechanics of the intervertebral disc are affected by this condition [27,28,29,30]. Previous studies showed that annulus injury could drive a series of molecular and biochemical changes in the intervertebral disc of murine [31, 32]. These studies imply that the rat model of intervertebral disc degeneration established by annulus puncture shares some similarities with disc degeneration in human. Second, as spine biomechanics is different in quadrupeds compared to bipeds, the rat discs are less affected by weight bearing, the induction of disc degeneration in this study is not physiological. However, OVX is a simple and technically easy method of inducing not only high bone turnover and thereby bone loss like postmenopausal osteoporosis in women but also intervertebral disc degeneration. This method is frequently used in many studies and can lead to intervertebral disc degeneration [8,9,10]. Consequently, the estrogen deficiency applied to the rat intervertebral disc produced biochemical, morphological, and structural changes that representative of mild degeneration.
In conclusion, under the dosage and intervention period used in this study, no protective effect on intervertebral disc degeneration was found by hPTH (1–34) treatment in OVX rats. This effect is most probably due to, at least in part, the excessive enhanced bone mass and strength. Therefore, a reasonable dosage and intervention period should be determined when treating intervertebral disc degeneration in the estrogen deficiency model using agents that stimulate bone formation. Considering a relatively higher dose of hPTH (1–34) was used in the present study in comparison with the clinical using, and taken together with the effect of modulating extracellular matrix metabolism observed in the previous study [25], the dual roles of PTH(1–34) affecting both bone and intervertebral disc raise the possibility for clinical use of PTH(1–34) in ameliorating disc degeneration in postmenopausal osteoporosis.
References
Mwale F, Masuda K, Pichika R et al (2011) The efficacy of Link N as a mediator of repair in a rabbit model of intervertebral disc degeneration. Arthritis Res Ther 13:R120
Boden SD, Davis DO, Dina TS et al (1990) Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am 72:403–408
Jackson RD, Mysiw WJ (2014) Insights into the epidemiology of postmenopausal osteoporosis: the Women’s Health Initiative. Semin Reprod Med 32:454–462
Baccaro LF, Conde DM, Costa-Paiva L et al (2015) The epidemiology and management of postmenopausal osteoporosis: a viewpoint from Brazil. Clin Interv Aging 10:583–591
Nanjo Y, Morio Y, Nagashima H et al (2003) Correlation between bone mineral density and intervertebral disk degeneration in pre- and postmenopausal women. J Bone Miner Metab 21:22–22
Fabreguet I, Fechtenbaum J, Briot K et al (2013) Lumbar disc degeneration in osteoporotic men: prevalence and assessment of the relation with presence of vertebral fracture. J Rheumatol 40:1183–1190
Wang YX, Griffith JF (2010) Effect of menopause on lumbar disc degeneration: potential etiology. Radiology 257:318–320
Wang T, Zhang L, Huang C et al (2004) Relationship between osteopenia and lumbar intervertebral disc degeneration in ovariectomized rats. Calcif Tissue Int 75:205–213
Luo Y, Zhang L, Wang WY et al (2013) Alendronate retards the progression of lumbar intervertebral disc degeneration in ovariectomized rats. Bone 55:439–448
Tian FM, Yang K, Wang WY et al (2015) Calcitonin suppresses intervertebral disk degeneration and preserves lumbar vertebral bone mineral density and bone strength in ovariectomized rats. Osteoporos Int 26:2853–2861
Poynton AR, Lane JM (2002) Safety profile for the clinical use of bone morphogenetic proteins in the spine. Spine (Phila Pa 1976) 27:S40–S48
Madiraju P, Gawri R, Wang H et al (2013) Mechanism of parathyroid hormone-mediated suppression of calcification markers in human intervertebral disc cells. Eur Cell Mater 25:268–283
Shen V, Birchman R, Wu DD et al (2000) Skeletal effects of parathyroid hormone infusion in ovariectomized rats with or without estrogen repletion. J Bone Miner Res 15:740–746
Zhou H, Shen V, Dempster DW et al (2001) Continuous parathyroid hormone and estrogen administration increases vertebral cancellous bone volume and cortical width in the estrogen-deficient rat. J Bone Miner Res 16:1300–1307
Lyritis GP, Georgoulas T, Zafeiris CP (2010) Bone anabolic versus bone anticatabolic treatment of postmenopausal osteoporosis. Ann N Y Acad Sci 1205:277–283
Jiang Y, Zhao JJ, Mitlak BH et al (2003) Recombinant human parathyroid hormone (1-34) [teriparatide] improves both cortical and cancellous bone structure. J Bone Miner Res 18(11):1932–1941
Dempster DW, Cosman F, Kurland ES et al (2001) Effects of daily treatment with parathyroid hormone on bone microarchitecture and turnover in patients with osteoporosis: a paired biopsy study. J Bone Miner Res 16:1846–1853
Kang R, Li H, Ringgaard S et al (2014) Interference in the endplate nutritional pathway causes intervertebral disc degeneration in an immature porcine model. Int Orthop 38:1011–1077
Shen Y, Li M, Wronski TJ (1997) Calcitonin provides complete protection against cancellous bone loss in the femoral neck of ovariectomized rats. Calcif Tissue Int 60:457–461
Chung SA, Wei AQ, Connor DE et al (2007) Nucleus pulposus cellular longevity by telomerase gene therapy. Spine (Phila Pa 1976) 32:1188–1196
Griffith JF, Yeung DK, Antonio GE et al (2005) Vertebral bone mineral density, marrow perfusion, and fat content in healthy men and men with osteoporosis: dynamic contrast-enhanced MR imaging and MR spectroscopy. Radiology 236:945–951
Griffith JF, Yeung DK, Tsang PH et al (2008) Compromised bone marrow perfusion in osteoporosis. J Bone Miner Res 23:1068–1075
Wang YX, Griffith JF, Ma HT et al (2011) Relationship between gender, bone mineral density, and disc degeneration in the lumbar spine: a study in elderly subjects using an eight-level MRI-based disc degeneration grading system. Osteoporos Int 22:91–96
Wang Y, Boyd SK, Battié MC et al (2011) Is greater lumbar vertebral BMD associated with more disk degeneration? A study using μCT and discography. J Bone Miner Res 26:2785–2791
Zhou Z, Tian FM, Gou Y et al (2016) Enhancement of lumbar fusion and alleviation of adjacent segment disc degeneration by intermittent PTH(1-34) in ovariectomized rats. J Bone Miner Res 31:828–838
Sztrolovics R, Alini M, Roughley PJ et al (1997) Aggrecan degradation in human intervertebral disc and articular cartilage. Biochem J 326:235–241
Li D, Yang H, Huang Y et al (2014) Lumbar intervertebral disc puncture under C-arm fluoroscopy: a new rat model of lumbar intervertebral disc degeneration. Exp Anim 63:227–234
Park JS, Park JB, Park IJ et al (2014) Accelerated premature stress-induced senescence of young annulus fibrosus cells of rats by high glucose-induced oxidative stress. Int Orthop 38:1311–1320
Than KD, Rahman SU, Wang L et al (2014) Intradiscal injection of simvastatin results in radiologic, histologic, and genetic evidence of disc regeneration in a rat model of degenerative disc disease. Spine J 14:1017–1028
Liang CZ, Li H, Tao YQ et al (2013) Dual release of dexamethasone and TGF-beta3 from polymeric microspheres for stem cell matrix accumulation in a rat disc degeneration model. Acta Biomater 9:9423–9233
Yang F, Leung VY, Luk KD et al (2009) Injury-induced sequential transformation of notochordal nucleus pulposus to chondrogenic and fibrocartilaginous phenotype in the mouse. J Pathol 218:113–121
Hou Y, Shi G, Shi J et al (2016) Study design: in vitro and in vivo assessment of bone morphogenic protein 2 combined with platelet-rich plasma on treatment of disc degeneration. Int Orthop 40:1143–1155
Funding
This work was partly supported by the National Natural Science Foundation of China (no. 31671235), Key project of Nature Science Foundation of Hebei Province (no. H2016209176), and Natural Science Foundation of Hebei province (no. H2013209257).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there they have no conflict of interest.
Ethical approval
All experimental procedures were reviewed and approved by the Institutional Animal Care and Use Committee.
Rights and permissions
About this article
Cite this article
Luo, Y., Li, Sy., Tian, Fm. et al. Effects of human parathyroid hormone 1–34 on bone loss and lumbar intervertebral disc degeneration in ovariectomized rats. International Orthopaedics (SICOT) 42, 1183–1190 (2018). https://doi.org/10.1007/s00264-018-3821-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-3821-2