Abstract
Purpose
Little information is available on the relationship between cervical sagittal alignment and health-related quality of life (HRQOL) in adolescent idiopathic scoliosis (AIS) patients. The aim of this study was to identify relationships between postoperative cervical sagittal alignment and HRQOL in AIS.
Methods
The study and control groups comprised 67 AIS patients (51 girls and 16 boys). All underwent anteroposterior and lateral plain radiography and completed clinical questionnaires. The radiographic parameters investigated were pre- and postoperative C2–C7 lordosis, C2–C7 sagittal vertical axis (SVA), T1 slope, T1 slope minus C2–C7 lordosis (TS-CL), thoracic kyphosis (TK), lumbar lordosis (LL), pelvic tilt (PT), sacral slope (SS), and pelvic incidence (PI). The Korean version of the SRS-22 questionnaire and the previously validated Short Form-36 (SF-36) outcome questionnaire were administered to evaluate HRQOL at last follow-up visits. Statistical analysis was performed to determine the significances of differences between preoperative and last follow-up radiological findings. In addition, correlations between radiological parameters and clinical questionnaire scores were sought.
Results
Radiological sagittal parameters were found to be significantly increased after surgical correction in terms of C2–C7 lordosis (3.5 ± 11.4), C2–C7 SVA (1.5 ± 6.0), T1 slope (3.5 ± 6.1), and TK (6.0 ± 8.1). However, no significant difference was observed for TS-CL, LL, PT, SS, and PI (P > 0.05). Correlation analysis revealed significant relationships between radiographic parameters and questionnaire scores. Multiple regression analysis was performed to identify predictors of HRQOL, and the results obtained revealed that postoperative T1 slope significantly predicted SRS, PCS, and MCS scores and that postoperative C2–C7 SVA predicted SRS scores.
Conclusions
Changes in cervical sagittal parameters were significant after deformity correction in AIS patients. Correlation analysis revealed significant relationships between postoperative radiographic parameters and HRQOL. In particular, T1 slope and C2–C7 SVA were found to be significant predictors of HRQOL in AIS patient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Scoliosis is a three-dimensional deformity of the spine and idiopathic cases of scoliosis usually exhibit a flattening of the sagittal profile. Coronal and sagittal plane correction is critical to the long-term success of scoliosis surgery. However, the sagittal profile often deteriorates when the Harrington technique is used, and its consequences include a flat back, an angular increase in lumbar lordosis below the fusion level, and low back pain [3, 16, 26].
The restoration of normal coronal and sagittal balances is an important goal for the surgical treatment of adolescent idiopathic scoliosis (AIS). The concave derotation technique involving rod prebending is able to restore thoracic kyphosis in hypokyphotic patients and maintains or regains normal lumbar lordosis in a considerable percentage of patients [1, 2, 6, 12]. Studies on the effects of scoliosis surgery on sagittal alignment of the cervical spine are scarce and it is possible that scoliotic patients treated surgically have a greater incidence of cervicodorsal pain than normal subjects [4, 12]. Furthermore, recent publications have shown regional cervical sagittal alignment is correlated with health-related quality of life (HRQOL) and reciprocally affected by changes in global sagittal alignment [10, 19, 20, 27].
Therefore, we considered that knowledge of correlations between cervical sagittal alignment and HRQOL would provide valuable information for treatment decision making and planning in AIS. However, the specific impact of cervical sagittal alignment on general health status has not been studied in AIS patients. Accordingly, the aim of this study was to identify relationships between postoperative cervical sagittal parameters and HRQOL in AIS patients. In addition, we attempted to identify cervical sagittal parameters that predict HRQOL.
Materials and methods
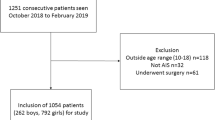
Sixty-seven consecutive patients with AIS that underwent spinal fusion were retrospectively reviewed. The study inclusion criteria were age below 16 years at time of surgery, a Lenke Type 1 curve, and at least 2 years of radiographic follow-up with adequate visualization of the cervical spine on preoperative and postoperative films. The surgeries were performed between March 2005 and August 2011. Curve correction was performed in all patients using all pedicle screw constructs, and deformity correction by concave rod derotation and additional intraoperative rod bending. Pedicle screws were inserted at every segment on both sides if possible. The precontoured titanium rod (6.5 mm) was rotated on the concave side subsequently bended more using intraoperative bending device for further sagittal and coronal correction. After completely locking the concave rod to each screw, another precontoured rod was attached to the convex.
Demographic characteristics and clinical assessment scores obtained using Korean version of Scoliosis Research Society-22 (SRS-22) [18] questionnaire and the Short-Form 36 (SF-36) questionnaire (MCS; mental component score and PCS; physical component score) [7] were analyzed. Sixty-seven subjects underwent whole spine radiographs preoperatively and at last follow-up. The study was approved by the Clinical Research Ethics Committee of our institution.
Standing anteroposterior and lateral radiography was taken in a comfortable upright position by one technician at a distance of 72 inches using a standard technique and the same machine. Also the standing lateral radiograph was taken with the upper extremities positioned gently flexed anterior to the body and with a horizontal gaze (Fig. 1). Radiographic parameters examined included C2–C7 lordosis, C2–C7 sagittal vertical axis (SVA), T1 slope, T1 slope minus C2–C7 lordosis (TS-CL), thoracic kyphosis (TK), lumbar lordosis (LL), pelvic tilt (PT), sacral slope (SS), and pelvic incidence (PI) (Fig. 2). C2–C7 SVA was defined as the distance between C2 and C7 sagittal plumb lines. The C2 sagittal plumb line was drawn as a lateral gravity line from the center of C2. The center of C2 was defined as the point of intersection of crossing diagonals of the vertebral body of C2 on a lateral radiograph. The C7 sagittal plumb line was defined as the lateral gravity plumb line from the center of C7. Anterior displacement of the sagittal plumb line was defined as positive. T1 slope was defined as the angle formed between the T1 upper end plate and the horizontal plane. All measurements were performed twice independently by three spine surgeons with an interval of 2 weeks between the two measurements to decrease intraobserver (Pearson correlation coefficient = 0.945, range 0.909–0.964) and interobserver errors (Pearson correlation coefficient = 0.939, range 0.902–0.959).
Statistical analysis was performed using SPSS Ver. 11.5 for Windows (SPSS, Chicago, IL, USA). Results are expressed as means ± standard deviations. Changes from pre-operative to post-operative alignment were compared using paired t test, and correlation analysis was performed using Pearson’s correlation to explore relationships between variables. Multiple regression analysis was used to identify parameters that predicted HRQOL. P values of <0.05 were deemed statistically significant.
Results
Measurements of radiological sagittal parameters
Table 1 summarizes the preoperative and postoperative (as determined at last follow-up visits) sagittal parameters of the 67 AIS patients. Radiological sagittal parameters were found to be significantly increased after surgical correction in terms of C2–C7 lordosis (3.5 ± 11.4), C2–C7 SVA (1.5 ± 6.0), T1 slope (3.5 ± 6.1), and TK (6.0 ± 8.1). However, no significant intergroup difference was observed for TS-CL, LL, PT, SS, or PI (P > 0.05).
Correlation between cervical sagittal parameters
Table 2 summarizes correlations between cervical sagittal parameters. Statistically significant correlations were observed between the following variables (Fig. 3): C2–C7 lordosis and T1 slope (r = 0.392, P = 0.001), C2–C7 lordosis and TS-CL (r = −0.751, P < 0.001), C2–C7 lordosis and TK (r = 0.405, P = 0.0007), and T1 slope and TS-CL (r = 0.312, P = 0.01), and T1 slope and TK (r = 0.864, P = <0.0001). C2–C7 SVA was only correlated with LL (r = 0.437, P = 0.0002).
Correlation between cervical sagittal parameters and HRQOL
Postoperative C2–C7 lordosis and T1 slope were found to be significantly correlated with HRQOL by correlation analysis (Table 3). However, postoperative C2–C7 lordosis and TS-CL were not found to be correlated with any of the three HRQOL scores (SRS, PCS, and MCS scores).
Multiple regression analysis was performed to identify predictors of QOL and showed postoperative T1 slope significantly predicted SRS, PCS, and MCS scores and that postoperative C2–C7 SVA significantly predicted SRS score (Table 4).
Discussion
Sagittal alignment of the thoracolumbar spine and pelvis, and long-term outcome in patients with AIS has become an increasingly important consideration in the spine field [24]. Although an abnormal spinopelvic morphology and flattened sagittal balance with loss of cervical lordosis (CL) are common in AIS patients, the relevance of cervical sagittal balance in AIS remains unclear. Earlier studies on TK and LL failed to address cervical sagittal alignment in their analyses but some authors have noted an inverse correlation between the thoracic and cervical alignment [9, 12]. Pesenti et al. [23] reported T1 slope was increased after scoliosis correction and is a good indicator of posteoperative changes for regional (cervical lordosis and thoracic kyphosis) and global parameters. However, relatively few studies have addressed relations between AIS and specific radiologic cervical parameters. Furthermore, the relationships established between cervical sagittal parameters and HRQOL in AIS are lacking.
Standing C2–C7 SVAs are closely maintained in a tight range in the normal cervical spine [8, 14, 15]. In particular, C2-S1 and C7-S1 SVAs are maintained to ensure alignment of the spine over the pelvis and femoral heads [15]. In degenerative cervical diseases, some parameters, namely C2–C7 lordosis, C2–C7 SVA, T1 slope, and TS-CL, can be used to assess cervical sagittal balance [22, 25]. Therefore, if cervical sagittal parameters are changed by disease, one could theorize that alterations in cervical sagittal alignment might affect clinical outcomes.
Malalignment of the cervical spine following anterior cervical surgery affects the development of clinical adjacent segment pathology [5, 22] and overall cervical sagittal alignments in postoperative radiographs were more kyphotic in patients with radiographically adjacent level degeneration [13]. Although few studies have addressed the topic, we felt that similar relations might be found between cervical sagittal parameters and HRQOL in AIS.
In the present study, cervical sagittal parameters were significantly changed by surgical correction in AIS patients and were related to each other. Although no correlations between cervical sagittal parameters and the development of spinal disorders have been confirmed in AIS, differences and relationships between sagittal radiological parameters can provide clues when cervical spinal deformities are examined in AIS. In the present study, AIS patients exhibited higher levels of C2–C7 lordosis, C2–C7 SVA, T1 slope, and TK after surgical correction, which suggests that cervical sagittal orientation is closely related to thoracolumbar deformity changes in AIS. Higher levels of C2–C7 lordosis might have occurred to compensate for increased TK, T1 Slope, and C2–C7 SVA of AIS patients. Thus, it appears that cervical sagittal parameters might be used as tools to predict HRQOL in AIS patients.
Furthermore, few studies have addressed relationships between HRQOL instrument scores and cervical sagittal measurements. However, these cervical parameters could be significantly correlated with HRQOL measures, and thus, could be important when analyzing radiographic alignment. In the present study, HRQOL scores were found to be significantly correlated with postoperative C2–C7 SVA and T1 slope. In fact, multiple regression analysis showed postoperative T1 slope (defined as the angle formed between the T1 upper end plate and the horizontal plane) was significantly related to HRQOL and a significant predictor of HRQOL. These findings indicate changes in spinal sagittal alignments are closely related to HRQOL and suggest that spinal alignment be considered by surgeons when treating AIS.
This study has several limitations that require consideration. First, the number of subjects tested was relatively small and no control group used, which diminished the statistical power of the study and its ability to detect correlations. Second, other radiological measurements (e.g., global sagittal balance) that could affect HRQOL were not included. Third, because no control group was enrolled, the incidence of cervicodorsal pain and muscle spasm and HRQOL differences between fused patients and unfused patients were not determined. According to some previous reports on normal subjects, T1 slope is a key factor determining cervical sagittal balance, and measurements of cervicothoracic junctional structures were identified as important predictors of chronic neck pain. So T1 slope is inferred to be a relevant factor on HRQOL of normal subjects too [17, 21]. Fourth, because children are notably more sensitive to the carcinogenic effects of ionizing radiation, judicious use of imaging methods and a search for newer technologies remain necessary [11]. These issues also require further investigation.
Nonetheless, this study shows significant relationships exist between cervical sagittal parameters in AIS patients and that significant changes in cervical sagittal parameters occur after surgical correction. Furthermore, correlation analysis revealed significant relationships between postoperative cervical sagittal parameters and HRQOL scores. In particular, a high T1 slope was found to negatively affect HRQOL scores. These findings should be taken into consideration when recommending the surgical correction of AIS.
References
Bridwell KH, Betz R, Capelli AM, Huss G, Harvey C (1990) Sagittal plane analysis in idiopathic scoliosis patients treated with Cotrel–Dubousset instrumentation. Spine 15:644–649
Canavese F, Turcot K, De Rosa V, de Coulon G, Kaelin A (2011) Cervical spine sagittal alignment variations following posterior spinal fusion and instrumentation for adolescent idiopathic scoliosis. Eur Spine J 20:1141–1148
Dickson RA, Lawton JO, Archer IA, Butt WP (1984) The pathogenesis of idiopathic scoliosis: biplanar spinal asymmetry. J Bone Joint Surg 66:8–15
Edgar MA, Mehta MH (1988) Long-term follow-up of fused and unfused idiopathic scoliosis. J Bone Joint Surg 70:712–716
Faldini C, Pagkrati S, Leonetti D, Miscione MT, Giannini S (2011) Sagittal segmental alignment as predictor of adjacent-level degeneration after a Cloward procedure. Clin Orthop Relat Res 469:674–681
Halm H, Castro WH, Jerosch J, Winkelmann W (1995) Sagittal plane correction in King-classified idiopathic scoliosis patients treated with Cotrel–Dubousset instrumentation. Acta Orthop Belg 61:294–301
Han CW, Lee EJ, Iwaya T, Kataoka H, Kohzuki M (2004) Development of the Korean version of short-form 36-item health survey: health related QOL of healthy elderly people and elderly patients in Korea. Tohoku J Exp Med 203:189–194
Hardacker JW, Shuford RF, Capicotto PN, Pryor PW (1997) Radiographic standing cervical segmental alignment in adult volunteers without neck symptoms. Spine 22:1472–1480
Hilibrand AS, Tannenbaum DA, Graziano GP, Loder RT, Hensinger RN (1995) The sagittal alignment of the cervical spine in adolescent idiopathic scoliosis. J Pediatr Orthop 15:627–632
Hwang SW, Samdani AF, Tantorski M, Cahill P, Nydick J, Fine A, Betz RR, Antonacci MD (2011) Cervical sagittal plane decompensation after surgery for adolescent idiopathic scoliosis: an effect imparted by postoperative thoracic hypokyphosis. J Neurosurg Spine 15:491–496
Ilharreborde B, Ferrero E, Alison M, Mazda K (2016) EOS microdose protocol for the radiological follow-up of adolescent idiopathic scoliosis. Eur Spine J 25:526–531
Ilharreborde B, Vidal C, Skalli W, Mazda K (2013) Sagittal alignment of the cervical spine in adolescent idiopathic scoliosis treated by posteromedial translation. Eur Spine J 22:330–337
Katsuura A, Kukuda S, Saruhashi Y, Mori K (2001) Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J 10:320–324
Knott PT, Mardjetko SM, Techy F (2010) The use of the T1 sagittal angle in predicting overall sagittal balance of the spine. Spine J 10:994–998
Kuntz C IV, Levin LS, Ondra SL, Shaffrey CI, Morgan CJ (2007) Neutral upright sagittal spinal alignment from the occiput to the pelvis in asymptomatic adults: a review and resynthesis of the literature. J Neurosurg Spine 6:104–112
Lagrone MO, Bradford DS, Moe JH, Lonstein JE, Winter RB, Ogilvie JW (1988) Treatment of symptomatic flat back after spinal fusion. J Bone Joint Surg 70:569–580
Lee JH, Park YK, Kim JH (2014) Chronic neck pain in young adults: perspectives on anatomic differences. Spine J 14:2628–2638
Lee JS, Lee DH, Suh KT, Kim JI, Lim JM, Goh TS (2011) Validation of the Korean version of the scoliosis research society-22 questionnaire. Eur Spine J 20:1751–1756
Lee JS, Suh KT, Kim JI, Lee HS, Goh TS (2013) Validation of the Korean version of the neck pain and disability scale. Asian Spine J 7:178–183
Lee JS, Youn MS, Shin JK, Goh TS, Kang SS (2015) Relationship between cervical sagittal alignment and quality of life in ankylosing spondylitis. Eur Spine J 24:1199–1203
Lee SH, Son ES, Seo EM, Suk KS, Kim KT (2015) Factors determining cervical spine sagittal balance in asymptomatic adults: correlation with spinopelvic balance and thoracic inlet alignment. Spine J 15:705–712
Park MS, Kelly MP, Lee DH, Min WK, Rahman RK, Riew KD (2014) Sagittal alignment as a predictor of clinical adjacent segment pathology requiring surgery after anterior cervical arthrodesis. Spine J 14:1228–1234
Pesenti S, Blondel B, Peltier E, Choufani E, Bollini G, Jouve JL (2016) Interest of T1 parameters for sagittal alignment evaluation of adolescent idiopathic scoliosis patients. Eur Spine J 25:424–429
Simony A, Hansen EJ, Carreon LY, Christensen SB, Andersen MO (2015) Health-related quality-of-life in adolescent idiopathic scoliosis patients 25 years after treatment. Scoliosis 10:22
Song JS, Choi BW, Song KJ (2014) Risk factors for the development of adjacent segment disease following anterior cervical arthrodesis for degenerative cervical disease: comparison between fusion methods. J Clin Neurosci 21:794–798
Upadhyay SS, Mullaji AB, Luk KD, Leong JC (1995) Relation of spinal and thoracic cage deformities and their flexibilities with altered pulmonary functions in adolescent idiopathic scoliosis. Spine 20:2415–2420
Yu M, Silvestre C, Mouton T, Rachkidi R, Zeng L, Roussouly P (2013) Analysis of the cervical spine sagittal alignment in young idiopathic scoliosis: a morphological classification of 120 cases. Eur Spine J 22:2372–2381
Acknowledgments
This study was supported by Biomedical Research Institute Grant (2015-02), Pusan National University Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any potential conflict of interest.
Additional information
Myung Soo Youn and Jong Ki Shin have contributed equally to this study.
Rights and permissions
About this article
Cite this article
Youn, M.S., Shin, J.K., Goh, T.S. et al. Relationship between cervical sagittal alignment and health-related quality of life in adolescent idiopathic scoliosis. Eur Spine J 25, 3114–3119 (2016). https://doi.org/10.1007/s00586-016-4488-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4488-2