Abstract
Purpose
The relationship between biomechanical instability and degenerative changes in the lumbar spine in chronic low back pain (CLBP) patients remains controversial. The main objective of this retrospective radiographical study was to evaluate changes in kinematics at different lumbar levels (in particular the L5–S1 level) with progressive grades of disc degeneration and facet joint osteoarthritis in CLBP patients.
Methods
Using standing neutral and dynamic flexion/extension (Fx/Ex) radiographs of the lumbar spine, in vivo segmental kinematics at L1–L2 through L5–S1 were evaluated in 72 consecutive CLBP patients. Disc degeneration was quantified using changes in signal intensity and central disc height on mid-sagittal T2-weighted magnetic resonance (MR) scans. Additionally, the presence or absence of facet joint osteoarthritis was noted on T2-weighted axial MR scans.
Results
Disc degeneration and facet joint osteoarthritis occurred independent of each other at the L5–S1 level (p = 0.188), but an association was observed between the two at L4–L5 (p < 0.001) and L3–L4 (p < 0.05) levels. In the absence of facet joint osteoarthritis, the L5–S1 segment showed a greater range of motion (ROM) in Ex (3.3° ± 3.6°) and a smaller ROM in Fx (0.6° ± 4.2°) compared with the upper lumbar levels (p < 0.05), but the differences diminished in the presence of it. In the absence of facet joint osteoarthritis, no change in L5–S1 kinematics was observed with progressive disc degeneration, but in its presence, restabilisation of the L5–S1 segment was observed between mild and severe disc degeneration states.
Conclusion
The L5–S1 motion segment exhibited unique degenerative and kinematic characteristics compared with the upper lumbar motion segments. Disc degeneration and facet joint osteoarthritis occurred independent of each other at the L5–S1 level, but not at the other lumbar levels. Severe disc degeneration in the presence of facet joint osteoarthritis biomechanically restabilised the L5–S1 motion segment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Biomechanical instability following degenerative changes in the lumbar spine may manifest as chronic low back pain (CLBP) [1]. In clinical praxis, radiographical assessment of bending motions of the lumbar spine is important as it may help in identifying the presence or absence of biomechanical instability in patients suffering from CLBP and help guide the course of clinical treatment.
However, the relationship between biomechanical instability and degree of degenerative changes in the lumbar spine in CLBP patients is controversial [1]. Some studies have reported that biomechanical instability tends to increase during early stages of degeneration, and stabilisation of motion segments occurs spontaneously in the advanced stages [2, 3]. Others have reported a monotonous increase in biomechanical stability with increasing disc degeneration in flexion/extension and lateral bending motions, but not in axial rotation [4, 5]. These contradictory findings could partly be attributed to the lack of consensus in defining and measuring degeneration and lumbar spinal instability [6]. Even with measuring angulatory motions on conventional flexion–extension radiographs of asymptomatic and symptomatic subjects, a large range of values exists for different lumbar levels, making it difficult to precisely define the norms of angulatory motion [7, 8]. Furthermore, pooling different lumbar levels together when there are apparent anatomical and functional differences between them could be an important reason behind the variation in results reported in previous studies.
Using 2D lateral static or dynamic radiographs, in vivo kinematics of lumbar spine in asymptomatic and symptomatic subjects have been studied in physiological bending conditions [8,9,10,11,12,13,14,15,16]. Pearcey et al. examined flexion (Fx) and extension (Ex) motions at different lumbar levels in 11 asymptomatic males and found more movement in Fx than in Ex at all lumbar levels except for the L5–S1 joint which showed no consistent pattern [8]. In a study of 14 healthy participants, Aiyangar et al. evaluated intervertebral contributions to L2–S1 extension during a dynamic lifting task [13]. The authors concluded that the contributions of middle segments (L3–L4 and L4–L5) were greater compared with the segments at cephalic and caudal ends, with the L4–L5 segment being the largest contributor throughout the range of motion [13]. Using cineradiographic techniques, Kanayama et al. analysed lower lumbar (L3–S1) segmental motions in eight healthy male volunteers during Fx and Ex motions and observed that Fx motion initiated at the L3–L4 segment and proceeded to lower lumbar segments after a phase lag, while the Ex motion occurred predominantly at the L5–S1 segment [9].
Segmental contribution to the overall lumbar motion is altered due to degenerative changes in the lumbar spine. Pearcey et al. examined Fx and Ex motions at different lumbar levels in CLBP patients with and without nerve tension signs and compared them with a normal control group [17]. The authors found that in Fx, patients with nerve tension signs were restricted at all lumbar level, while those without it were only restricted at lower lumbar levels [17]. In a study of 10 symptomatic subjects with discogenic pain due to L4–L5 and L5–S1 disc degeneration, hypermobility was reported at the L3–L4 and hypomobility at the L5–S1 segments, when compared with a control group of asymptomatic subjects [12]. Bali and Kumar [10] in their prospective cohort study of symptomatic (n = 67) and asymptomatic (n = 52) Asian subjects found significant differences between symptomatic and asymptomatic cohorts in the upper (L1–L4) and lower (L4–S1) lumbar flexion–extension kinematics.
Commonly occurring spine pathologies such as lumbar disc herniation and degenerative spondylolisthesis have their origins predominantly in the lower lumbar spine (L4–L5 and L5–S1) [18,19,20]. Of the lower lumbar levels, the L5–S1 level is unique because of the presence of iliolumbar and lumbosacral ligaments, coronally oriented facets and laminae, wedge-shaped disc and its junctional location, and therefore necessitates separate attention. To the best of our knowledge, no study has compared segmental motion across all lumbar levels (between L1 and S1) in CLBP patients, accounting for disc degeneration and facet joint osteoarthritis. With this in mind, we conducted a retrospective study of CLBP patients to evaluate segmental kinematics (using dynamic flexion–extension radiographs) at all lumbar levels from L1–L2 through L5–S1 and also quantified disc degeneration and facet joint osteoarthritis [on T2-weighted magnetic resonance (MR) scans] at all of these levels. We hypothesised that in CLBP patients, the L5–S1 motion segment regardless of the progressive degeneration of the disc and facet joints demonstrates different motion patterns compared with the upper lumbar motion segments.
Materials and methods
With prior approval from University of New South Wales, Human Research Ethics Advisory Panel (NRR-HC 16825), a retrospective study of CLBP patients who presented at Spine Service clinics (St. George Private Hospital, Sydney) between January 2010 and January 2013 was conducted. CLBP was defined as pain existing in the lower back for the duration of 12 weeks or more.
Patient inclusion and exclusion criteria
Inclusion criteria
Patients in the age group of 18–70 years with CLBP; with or without lower limb pain; and no indication for spinal surgery based on clinical, radiographical and T2-weighted MRI assessments were considered for the purposes of this study.
Exclusion criteria
Patients with generalised body pain; metabolic causes of pain such as osteoporosis, spine infections and spine tumours; history of spinal trauma, prior lumbar spine surgery, inflammatory arthritis, spinal deformity (scoliosis and/or kyphosis Cobb angle > 10°); severe medical illness due to causes unrelated to spine; mental health issues; and intellectual disability were excluded from this study.
Patient demography
Deidentified data from 72 CLBP patients (51 males, 21 females) who met the eligibility criteria were considered for the purposes of this study. Patient demography data are presented in Table 1.
Assessment of radiographs
Angular measurements, to the nearest degree, were recorded on digital images of upright anteroposterior (AP), lateral (LR), dynamic Fx and Ex radiographs of the lumbosacral spine (L1–S1) using commercially available software Surgimap (vers. 1.2.1.82, Nemaris Inc., New York, USA). Scoliosis on the AP radiograph was measured as the angle between the superior endplate of L1 and a line intersecting inferior-most points of the pedicles of L5 (Fig. 1). Global lordosis (in neutral, Fx and Ex positions) was measured on the LR radiograph as the angle between the superior endplate of L1 and the superior endplate of S1 using the Cobb angle method (Fig. 1) [21].
Segmental lordosis at L1–L2 through L5–S1 in neutral, Fx and Ex radiographs was also measured using upright, LR and dynamic Fx/Ex radiographs. For each segmental level, lines intersecting the anterior-most and posterior-most corners of each vertebral body above and below the disc were drawn parallel to the respective endplates. The angle between these lines was defined as segmental lordosis for the corresponding level (Fig. 1).
Using the above radiographic measurements, kinematics data for global and segmental motions were calculated. Global extension to flexion range of motion (E2Fg ROM) was calculated by subtracting lordosis in extension from lordosis in flexion. Global neutral to flexion range of motion (N2Fg ROM) was calculated by subtracting lordosis in neutral position from lordosis in flexion. Global extension to neutral range of motion (E2Ng ROM) was calculated by subtracting lordosis in extension from lordosis in neutral position. Segmental kinematics (E2Fs ROM, N2Fs ROM and E2Ns ROM) at each of the lumbar levels were calculated in a similar manner.
Assessment of MR scans
A scoring system was adopted to quantify the degree of disc degeneration using changes in signal intensity and central disc height on mid-sagittal T2-weighted MR scans. Each disc was assigned weight per the following protocols:
-
1.
No points, if the disc was normal (bright homogeneous centre and normal disc height compared with adjacent level discs).
-
2.
One point when the disc was inhomogeneous (but not entirely black), and two points when the disc was entirely black.
-
3.
One point for a disc height loss of < 50% (compared with the cephalad disc height), and two points for a disc height loss of > 50%.
Points were added to give an overall grade (0–4) to each disc (Fig. 2).
Assessment of the L5–S1 disc on five different T2-weighted magnetic resonance images. Grade 0: normal disc with a bright homogeneous centre and disc height preserved; grade 1: mildly inhomogeneous disc but disc height preserved; grade 2: mildly inhomogeneous disc with a disc height loss of < 50%; grade 3: black disc with a disc height loss of < 50%; grade 4: black disc with a disc height loss of > 50%
In addition, presence (1) or absence (0) of facet joint osteoarthritis was noted on T2-weighted axial MR scans. Facet joint osteoarthritis was deemed present if the axial MR scans showed an absence of facet joint space, irregular facet joint surface, presence of osteophytes, cysts or excessive facet joint fluid. Previous studies have shown that excess facet joint fluid is an indicator of facet joint degeneration and associated instability [22,23,24]. For the purposes of this study, the presence of excess facet fluid was recognised as space > 2 millimetres between the articulating faces of the facet joint on axial MR cuts.
Statistical analyses, intra- and interobserver reliability
For data analyses, statistical package SPSS (vers. 20, IBM Corporation, Armonk, USA) was used. The level of significance was set to 5% (α = 0.05), and 95% confidence interval (CI) was reported. A normality check on kinematics data using Shapiro–Wilk test revealed non-normality in the data set; therefore, nonparametric Mann–Whitney U test and Kruskal–Wallis test were used for detecting kinematic differences between groups. Chi-square test of independence on the contingency table between different grades of disc degeneration (nil, mild, severe) and facet joint osteoarthritis (absent, present) were conducted for different lumbar levels.
Measurements on radiographs and MR scans were performed by two independent observers. Repeat measurements were performed by the first observer 3 weeks after the first measurements. For lordosis measurements, intra-class correlation coefficients for intra-observer and interobserver reliability were 0.89 (95% CI 0.65–0.95) and 0.83 (95% CI 0.67–0.92), respectively. For disc grading on MR scans, Cohen’s kappa coefficient for intra-observer and interobserver reliability was 0.95 (95% CI 0.82–1.00) and 0.73 (95% CI 0.53–0.93), respectively.
Results
The average CLBP symptom duration in our patient cohort was approximately 3 years (152 weeks), and the average patient age was ~ 43 years (Table 1). Disc degeneration and facet joint osteoarthritis were more prevalent at the lower lumbar levels (L4–L5 and L5–S1) when compared with the upper levels, with the highest prevalence observed at the L5–S1 level (79% of the discs degenerate, Table 2). The differences in kinematics (both global and segmental) between males and females were not statistically significant at any of the lumbar levels.
Association between disc degeneration and facet joint osteoarthritis
Chi-square tests showed that at the L5–S1 level, disc degeneration and facet joint osteoarthritis occurred independent of each other (p = 0.188). At the L3–L4 and L4–L5 levels, an association was found between the occurrence of disc degeneration and facet joint osteoarthritis (p < 0.05 and p < 0.001, respectively).
Kinematics of segments with and without disc degeneration
Segmental ROM for motion segments with nil (grade = 0), mild (grade = 1, 2) and moderate-to-severe (grade = 3, 4) disc degeneration across different lumbar levels is presented in Table 3.
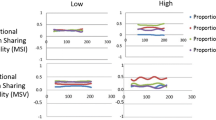
In motion segments with nil disc degeneration, there was no difference in E2Ns ROM between any two lumbar levels. However, N2Fs ROM at the L5–S1 level (0.8° ± 5.1°) was smaller compared with the L1–L2 (4.6° ± 4.1°, p < 0.05) and L2–L3 levels (4.0°± 4.3°, p < 0.05).
In motion segments with mild disc degeneration, E2Ns ROM at the L5–S1 level (3.3° ± 3.3°) was greater when compared with the L4–L5 (0.9° ± 2.3°, p < 0.05) and the L3–L4 levels (1.3° ± 2.9°, p < 0.05). No difference in N2Fs ROM between any two lumbar levels was observed.
In motion segments with moderate-to-severe disc degeneration, N2Fs ROM at the L5–S1 level (0.8° ± 2.6°) was smaller compared with the L4–L5 level (3.5° ± 3.8°, p < 0.05). Similarly, E2Fs ROM at the L5–S1 level (2.6° ± 3.4°) was smaller compared with the L4–L5 level (6.3° ± 3.4°, p < 0.05).
Kinematics of segments with and without facet joint osteoarthritis
Segmental ROM for motion segments with (Fac = 1) and without (Fac = 0) facet joint osteoarthritis across different lumbar levels is presented in Table 4.
In L5–S1 motion segments without facet joint osteoarthritis, E2NsROM (3.3° ± 3.6°) was greater and N2FsROM (0.6° ± 4.2°) was smaller compared with other lumbar levels (p < 0.05, all comparisons). In motion segments with facet joint osteoarthritis, no difference in kinematics was observed between any two lumbar levels.
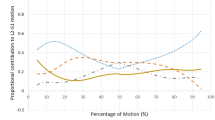
Kinematics of the L5–S1 segment with progressive grades of disc degeneration with and without facet joint osteoarthritis
Segmental ROM for the L5–S1 segment with varying grades of disc degeneration, with or without facet joint osteoarthritis, is presented in Table 5.
In L5–S1 motion segments without facet joint osteoarthritis, no difference in kinematics was observed with progressive grades of disc degeneration. In segments with facet joint osteoarthritis, severely degenerated discs had smaller N2FsROM compared with the mildly degenerated discs (0.8° ± 2.0° and 4.2° ± 5.3°, respectively, p < 0.05). Similarly, E2FsROM in severely degenerated discs was smaller compared with mildly degenerated discs (2.3° ± 3.9° and 7.2° ± 5.6°, respectively, p < 0.05).
Discussion
Previous studies on the assessment of lumbar spine kinematics in CLBP patients have mostly focused on identifying abnormal motion patterns by comparisons with a normal control group, without considering the underlying degenerative changes that may primarily be responsible for the change in kinematics [10, 17]. To our knowledge, this is the first study to compare segmental motion across all lumbar levels in CLBP patients, accounting for disc degeneration and facet joint osteoarthritis. We found that disc degeneration and facet joint osteoarthritis occurred mostly at the lower lumbar levels (L4–L5: 68% and 47%, respectively; L5–S1: 79% and 54%, respectively).
Furthermore, we found that at the L5–S1 level, disc degeneration occurred independent of facet joint osteoarthritis. However, at the L3–L4 and L4–L5 levels, an association between the occurrence of disc degeneration and facet joint osteoarthritis was observed. Previous studies have investigated the association (or lack thereof) between disc degeneration and facet joint osteoarthritis in the lumbar spine but only for mixed lumbar levels [25,26,27]. Butler et al. investigated the relationship between the two in a cohort of 68 patients using their CT and MR scans and concluded that disc degeneration precedes facet joint osteoarthritis which may be secondary to the mechanical overloading of the facet joints [25]. Fujiwara et al. evaluated disc degeneration and facet joint osteoarthritis in MR scans of 183 consecutive patients with low back and/or leg pain symptoms and concluded that disc degeneration is more closely associated with ageing than with facet joint osteoarthritis, and that it may take up to 20 years or more to develop facet joint osteoarthritis following the onset of disc degeneration [26]. Contradictory to the above findings, Videman et al. showed that in 20% of the degenerative spines, facet joint osteoarthritis preceded disc degeneration [27].
In the present study, since disc degeneration was found to be significantly associated with facet joint osteoarthritis at the upper lumbar levels but not at the L5–S1 level, kinematics across different lumbar levels could not be isolated for levels with disc degeneration only or levels with facet joint osteoarthritis only. Therefore, segmental kinematics for levels with nil or mixed degenerative changes are reported (Tables 3 and 4). The L5–S1 segmental kinematics patterns were found to be different compared with upper lumbar levels. In segments with nil disc degeneration, N2FsROM at the L5–S1 level was lower compared with the upper lumbar levels. With mild disc degeneration, N2FsROM at L5–S1 increased and the differences with upper lumbar levels diminished below statistical significance. However, with severe disc degeneration, N2FsROM at L5–S1 decreased to a level that was not different from nil disc degeneration, and significantly lower compared with the L4–L5 level. In motion segments without facet joint osteoarthritis, E2Ns ROM was significantly greater and N2FsROM was significantly smaller at the L5–S1 level compared with the upper lumbar levels. These results suggest that in the non-degenerated state, the contribution of the L5–S1 motion segment to lumbar spine kinematics is significantly greater in extension and significantly less in flexion compared with the upper lumbar levels, which corroborates previous findings [9].
Since disc degeneration and facet joint osteoarthritis occurred independently at the L5–S1 level, kinematics patterns at this level were separately analysed by categorising the motion segments into with and without facet joint osteoarthritis groups (Table 5). In segments without facet joint osteoarthritis, no variation in kinematics was observed with progressive disc degeneration. However, in segments with facet joint osteoarthritis, severely degenerated discs had significantly lower E2FsROM and N2FsROM compared with the mildly degenerated discs. These results suggest that at the L5–S1 segment, the concurrent occurrence of severe disc degeneration and facet joint osteoarthritis significantly limits the mobility of the segment.
The L5–S1 level is different from the upper lumbar levels because of the presence of iliolumbar and lumbosacral ligaments, coronally oriented facets and laminae, wedge-shaped disc and its junctional location, and therefore necessitates separate attention. The iliolumbar ligament (ILL) is a strong ligament, which attaches the transverse processes of the L5 vertebra to the iliac crest. The anterior band of the ligament is in coronal plane and blends with the periosteum of anterior margin of the iliac crest, while posterior band runs obliquely and posteriorly to attach to the posterior margin of the crest. Luk et al. noted that the ILL is not present at birth and develops from metaplasia of muscle fibres of quadratus lumborum muscle into collagen fibres in the first two decades of life [28]. Leong et al. hypothesised that the ILL fibres act as slings of hammock, which suspend the L5 vertebra from the iliac crest and prevent the collapse of the L5–S1 segment with disc degeneration [29]. The results from the present study provide evidence in support of Leong et al. hypothesis, and the restabilisation of the L5–S1 segment in severely degenerated discs could partly be attributed to the sling effect of the ILL fibres [29]. No such restabilisation effect was observed at the L4–L5 level which became biomechanically unstable with progressive disc degeneration.
The present study has certain limitations. This is a retrospective study of 72 consecutive CLBP patients with average symptom duration of approximately three years. The kinematics data were not compared with data from a case–control cohort of asymptomatic individuals without any disc degeneration and facet joint osteoarthritis. At the L1–L2 and L2–L3 levels, statistical tests could not be conducted to examine the association between disc degeneration and facet joint osteoarthritis due to inadequate sample size (less than 10 patients). Digital formatting and cursor-controlled measurement of the angles on screen might potentially introduce measurement errors. Routine MR scanning cannot detect early signs of facet joint osteoarthritis, such as minor chondral changes and synovial inflammation.
In CLBP patients, a significant decrease in segmental motion in the lumbar spine with age regardless of the diagnosis has been previously reported [7]. How much of this decrease is attributable to the degenerative changes in the passive elements and/or decrease in neuromuscular coordination with age remains to be explored. Nonetheless, the present study highlighted some unique degenerative and kinematic characteristics of the L5–S1 segment compared with the upper lumbar segments.
Conclusions
In chronic low back pain patients, no association was found between the occurrence of disc degeneration and facet joint osteoarthritis at the L5–S1 level, whereas a strong association was found between the two at the L3–L4 and L4–L5 levels. Compared with the upper lumbar levels, the L5–S1 level exhibited unique motion characteristics in the intact and degenerate states, with restabilisation of the motion segment observed with severe disc degeneration and facet joint osteoarthritis. The unique anatomical features of the L5–S1 level, especially the wedge-shaped disc and the presence of iliolumbar ligament, may have a predominant role to play in restabilising the level with severe degeneration of the disc and facet joints.
References
Kirkaldy-Willis WH, Farfan HF (1982) Instability of the lumbar spine. Clin Orthop Relat Res 165:110–123
Fujiwara A, Lim TH, An HS, Tanaka N, Jeon CH, Andersson GB, Haughton VM (2000) The effect of disc degeneration and facet joint osteoarthritis on the segmental flexibility of the lumbar spine. Spine 25:3036–3044
Tanaka N, An HS, Lim TH, Fujiwara A, Jeon CH, Haughton VM (2001) The relationship between disc degeneration and flexibility of the lumbar spine. Spine J 1:47–56
Oxland TR, Lund T, Jost B, Cripton P, Lippuner K, Jaeger P, Nolte LP (1996) The relative importance of vertebral bone density and disc degeneration in spinal flexibility and interbody implant performance. An in vitro study. Spine 21:2558–2569
Kettler A, Rohlmann F, Ring C, Mack C, Wilke HJ (2011) Do early stages of lumbar intervertebral disc degeneration really cause instability? Evaluation of an in vitro database. Eur Spine J 20:578–584
Boden SD, Wiesel SW (1990) Lumbosacral segmental motion in normal individuals. Have we been measuring instability properly? Spine 15:571–576
Hayes MA, Howard TC, Gruel CR, Kopta JA (1989) Roentgenographic evaluation of lumbar spine flexion–extension in asymptomatic individuals. Spine 14:327–331
Pearcy M, Portek I, Shepherd J (1984) Three-dimensional X-ray analysis of normal movement in the lumbar spine. Spine 9:294–297
Kanayama M, Abumi K, Kaneda K, Tadano S, Ukai T (1996) Phase lag of the intersegmental motion in flexion–extension of the lumbar and lumbosacral spine. An in vivo study. Spine 21:1416–1422
Bali T, Kumar MN (2015) Relative contribution of upper and lower lumbar spinal segments to flexion/extension: comparison between normal spines and spines with disc disease in Asian patients. Asian Spine J 9:770–775
Li G, Wang S, Passias P, Xia Q, Li G, Wood K (2009) Segmental in vivo vertebral motion during functional human lumbar spine activities. Eur Spine J 18:1013–1021
Passias PG, Wang S, Kozanek M, Xia Q, Li W, Grottkau B, Wood KB, Li G (2011) Segmental lumbar rotation in patients with discogenic low back pain during functional weight-bearing activities. J Bone Jt Surg Am 93:29–37
Aiyangar A, Zheng L, Anderst W, Zhang X (2015) Apportionment of lumbar L2–S1 rotation across individual motion segments during a dynamic lifting task. J Biomech 48:3718–3724
Wong KWN, Leong JCY, M-k Chan, Luk KDK, Lu WW (2004) The flexion–extension profile of lumbar spine in 100 healthy volunteers. Spine 29:1636–1641
Harada M, Abumi K, Ito M, Kaneda K (2000) Cineradiographic motion analysis of normal lumbar spine during forward and backward flexion. Spine 25:1932–1937
Wong KW, Luk KD, Leong JC, Wong SF, Wong KK (2006) Continuous dynamic spinal motion analysis. Spine 31:414–419
Pearcy M, Portek I, Shepherd J (1985) The effect of low-back pain on lumbar spinal movements measured by three-dimensional X-ray analysis. Spine 10:150–153
Davis Richard A (1994) A long-term outcome analysis of 984 surgically treated herniated lumbar discs. J Neurosurg 80:415–421
Weinstein JN, Tosteson TD, Lurie JD et al (2006) Surgical vs nonoperative treatment for lumbar disk herniation: the spine patient outcomes research trial (sport): a randomized trial. JAMA 296:2441–2450
Weinstein JN, Lurie JD, Tosteson TD, Hanscom B, Tosteson ANA, Blood EA, Birkmeyer NJO, Hilibrand AS, Herkowitz H, Cammisa FP, Albert TJ, Emery SE, Lenke LG, Abdu WA, Longley M, Errico TJ, Hu SS (2007) Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. N Engl J Med 356:2257–2270
Hicks GE, George SZ, Nevitt MA, Cauley JA, Vogt MT (2006) Measurement of lumbar lordosis: inter-rater reliability, minimum detectable change and longitudinal variation. J Spinal Disord Tech 19:501–506
Rihn JA, Lee JY, Khan M, Ulibarri JA, Tannoury C, Donaldson WF 3rd, Kang JD (2007) Does lumbar facet fluid detected on magnetic resonance imaging correlate with radiographic instability in patients with degenerative lumbar disease? Spine 32:1555–1560
Schellinger D, Wener L, Ragsdale BD, Patronas NJ (1987) Facet joint disorders and their role in the production of back pain and sciatica. Radiographics 7:923–944
Caterini R, Mancini F, Bisicchia S, Maglione P, Farsetti P (2011) The correlation between exaggerated fluid in lumbar facet joints and degenerative spondylolisthesis: prospective study of 52 patients. J Orthop Traumatol 12:87–91
Butler D, Trafimow JH, Andersson GB, McNeill TW, Huckman MS (1990) Discs degenerate before facets. Spine 15:111–113
Fujiwara A, Tamai K, Yamato M, An HS, Yoshida H, Saotome K, Kurihashi A (1999) The relationship between facet joint osteoarthritis and disc degeneration of the lumbar spine: an MRI study. Eur Spine J 8:396–401
Videman T, Battie MC, Gill K, Manninen H, Gibbons LE, Fisher LD (1995) Magnetic resonance imaging findings and their relationships in the thoracic and lumbar spine. Insights into the etiopathogenesis of spinal degeneration. Spine 20:928–935
Luk K, Ho H, Leong J (1986) The iliolumbar ligament. A study of its anatomy, development and clinical significance. J Bone Jt Surg (British Volume) 68-B:197–200
Leong JCY, Luk KDK, Chow DHK, Woo CW (1987) The biomechanical functions of the iliolumbar ligament in maintaining stability of the lumbosacral junction. Spine 12:669–674
Acknowledgements
The authors thank George Assaad, Leo Ho, Ifrah Zubair and Nerida Grewal for their help with data collection. This work was supported by internal research funds from Spine Service.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest related to this work.
Rights and permissions
About this article
Cite this article
Sabnis, A.B., Chamoli, U. & Diwan, A.D. Is L5–S1 motion segment different from the rest? A radiographic kinematic assessment of 72 patients with chronic low back pain. Eur Spine J 27, 1127–1135 (2018). https://doi.org/10.1007/s00586-017-5400-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5400-4