Abstract
Introduction
Surgery for correction of sagittal imbalance has frequent adverse events and complications. The most frequent cause of failure is inadequate correction of imbalance. The aim of this study is to verify the accuracy of three published methods (exact method by Ondra, FBI method by Le Huec and spinofemoral angle method by Lamartina) to preoperatively calculate the needed correction.
Design
This is a retrospective cohort study.
Methods
Fifteen patients treated for correction of sagittal imbalance, with preoperative and postoperative lateral standing whole spine radiographs, were identified. Preoperative calculation of the amount of needed correction has been done using these methods. In postoperative X-rays, the amount of correction obtained with and the degree of correction of sagittal imbalance have been measured.
Results and discussion
The FBI and SFA methods obtain equivalent calculations of the amount of needed correction. The estimated correction angle with both methods is higher than that calculated with the exact trigonometric method. The difference between the latter and the former methods is equivalent to the observed excess of pelvic tilt.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In a normal, asymptomatic state, pelvis and spine are in balance. This term was first introduced by Vaz [1] as a correlation between the pelvis and the spine. Sagittal imbalance is a complex multifactorial entity that affects the patient when this balance is lost. Back pain, gait disturbance and disability are the most important symptoms referred by patients; all the daily activities are heavily impaired by this pathological status. In these patients surgical correction is needed to restore a correct balance of the spine, leading to a better quality of life [2]. Pedicle Subtraction Osteotomy (PSO), Smith-Petersen Osteotomy and Ponte Osteotomy are the most common procedures to achieve a better lumbar lordosis. In this kind of surgery the calculation of the amount of correction needed to obtain a good sagittal balance is a fundamental aspect of the surgical planning in order to choose the correct procedure to improve lordosis of the right number of degrees. Many scientific papers proposed different procedures of calculation, with different results in terms of correction angle of lordosis and of clinical results. This paper aims to compare three different techniques in calculating the amount of correction needed to achieve a correct sagittal balance.
Design
Current concepts review. Retrospective analysis.
Methods
We compared the results of three different techniques in calculating the amount of correction needed in patients affected with sagittal imbalance. These three methods propose different formulas to calculate the degrees of correction that must be achieved to obtain a good sagittal balance. These formulas are the one proposed by Lamartina et al. [3], one proposed by Ondra et al. [4] and the last defined by Le Huec et al. [5]. Fifteen patients that had been surgically treated in our Division for a sagittal imbalance were enrolled in this study. Preoperative and postoperative standing full spine X-rays in AP and lateral views of each patient were analyzed. On these X-rays, pelvic parameters, femoral flexion, sagittal vertical axis (SVA) and lumbar lordosis were measured (Table 1). We then calculated on the postoperative X-rays the predicted surgical correction in each patient using the three methods, Lamartina’s spinofemoral angle (SFA), Le Huec’s FBI and Ondra’s exact method. We then compared the results in terms of predicted values of correction (Table 2).
Results
Definition of sagittal balance and imbalance
Sagittal balance is the situation in which the subject is capable of maintaining the standing position with or without minimal muscular work. This event is the result of the interaction of different factors, as bone morphology, ligament tension, disc status, and many others. Radiographically, a subject can be considered in a state of sagittal balance when the vertical line passing from the center of the body of C7 (C7 plumb line) crosses the posterior upper corner of the S1 endplate. Anterior imbalance occurs as the plumb line of the 7th cervical vertebra passes in front of the femoral heads [5, 6]; posterior sagittal imbalance occurs as the C7 plumb line passes on the back of the S1 endplate. Sagittal imbalance is an important cause of morbidity in adults and elderly, and its surgical correction improved clinical outcomes and health-related quality of life [2] (Fig. 1a, b).
Ondra’s method
Ondra et al. [7] defined a method to estimate preoperatively the amount of correction needed to restore the sagittal balance of the patient. This was considered as the displacement of the C7 plumb line over the postero-superior corner of S1 endplate. This method did not consider pelvic parameters and the level of correction. A second work of Ondra in the same year (submitted secondly but published before the other) proposed a second “exact” method [4]. The apex of the estimated angle of correction was placed on the anterior wall of the vertebra chosen for pedicle subtraction osteotomy (PSO). A line was drawn from this point to the midpoint of the preoperative position of the C7 body. A vertical line crossing the sacrum was drawn. Performing the osteotomy, C7 will rotate along an arc centered on the apex of the PSO until it meets the sacral vertical line. The angle subtended by this arc is the one suggested by Ondra that has to be considered as the amount of correction needed during the surgery to obtain a sagittally balanced patient (Fig. 2).
The Ondra method applied in Fig. 1 case. “a” is the calculated angle of correction
FBI method
Le Huec’s method [5] builds the entity of correction on the sum of three different angles. The first is the so-called “angle of C7 translation (C7TA)”, based on two different lines. The first line is drawn from C7 to the anterior wall of L4, the second from the translation of C7 on the vertical line of S1 to L4. This angle is C7TA. The second angle is the “angle of femur obliquity (FOA)”, that represents femoral inclination in respect to a vertical line. The last angle is the “angle of tilt compensation (PTCA)” based on the difference from the pelvic tilt (PT) of the patient and its theoretical value based on Roussouly’s classification and Legaye’s rule [9]. The FBI angle of correction equals to C7TA + FOA + PTCA (Fig. 3).
The FBI method applied in Fig. 1 case. The sum of “a”, “c”, and the difference of “b” with the theoretical PT of the patient is the calculated angle of correction
SFA method
Lamartina et al. [3] proposed the spinofemoral angle (SFA) to calculate the amount of correction needed in sagittal imbalance surgery. This method is based on a single angle, formed by the femoral axis and the line drawn from the center of C7 to the point where the vertical line from the posterior end of S1 plate intersects the level of planned osteotomy. SFA equals the sum of femoral flexion angle plus the angle of C7 translation, with an error <3° (Fig. 4).
The SFA method applied in Fig. 1 case. “a” is the calculated angle of correction
To increase the accuracy of this method, it is possible to add two parameters: hip extension reserve and thoracic hypokyphosis. SFA angle is a very simple way to calculate the amount of correction needed; it avoids lack of accuracy of the other methods while keeping its simplicity.
Results analysis
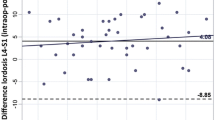
Preoperative values of pelvic tilt showed a mean of 34.5°, while its postoperative value was of 21.9° (p > 0.05). Femoral tilt had a mean of 13.1° preoperatively, while after surgery this value decreased to 7.5° (p > 0.05). Lumbar lordosis increased from 21 to 38.7° (p > 0.05), while the sagittal vertical axis (SVA) decreased from 83.6 to 37.6 mm (p > 0.05). Each preoperative, full spine standing X-ray was analyzed and the angle of correction was measured using the three different methods. With Ondra’s exact method the mean entity of the correction angle was of 13.1°. With Le Huec’s FBI method the mean of planned correction angles was of 35.4°. Lamartina’s SFA method calculated a mean of 36.7° of correction.
Discussion
Vertebral osteotomies are a group of surgical techniques capable of restoring the sagittal balance of the spine, translating the C7 plumb line posteriorly. The most used vertebral osteotomies are the pedicle subtraction osteotomy (PSO), Smith–Petersen osteotomy (SPO) and Ponte osteotomy (PO). With these techniques a spinal surgeon can gain, respectively, 30°, 10° and 5° of lordosis in the treated area. These osteotomies can be combined to obtain a higher correction. The exact degrees of correction must be planned preoperatively to define which of these techniques should be used. It is then important to have the correct amount of degrees to plan the surgery to obtain a correct sagittal balance, with a C7 plumb line that crosses the posterior upper corner of S1. As seen in the results, the exact method of Ondra tends to give a lower amount of needed correction than FBI and SFA methods. This can produce an inadequate correction of the lumbar spine, leading to a postoperative status of imbalance and consequently to back pain and surgical failure.
All these three methods show limits in the analysis of the thoracic spine; the variations of this curve can affect seriously the postoperative result [6]. While the exact method and the FBI method do not consider the thoracic spine at all, in SFA method we can find a thoracic modifier that should be applied in patients with a hypokyphotic and flexible thoracic spine. The comprehension of the role of thoracic spine is anyway inadequately understood. As a general consideration, the authors suggest two different situations where to treat and consider the thoracic spine; in the case of a hyperkyphotic spine it is important to correct this curve to values similar to the angle of pelvic incidence. In the case of a hypokyphotic thoracic spine, an increase in thoracic kyphosis is very common after the surgery; for this reason it is better to overcorrect the lumbar lordosis. Obviously, the inclusion of the thoracic curve in the instrumented area will lead to more predictable results.
Conclusions
Lumbar osteotomies are good surgical techniques to improve the global sagittal balance of the spine, increasing the lumbar lordosis and decreasing the pelvic (lower pelvic tilt) and the femoral (lower femoral flexion) compensation. FBI and SFA methods obtain similar preoperative values of lordosis correction, and both of them give higher values of correction compared to Ondra’s exact method. A new prospective study is however desirable to establish which of these three methods is the most accurate in calculating the adequate amount of correction needed in sagittal imbalance surgery. It will be also important to define in a more precise way the role of the variations in the thoracic spine in the sagittal balance of the spine after thoracolumbar fixation for sagittal imbalance.
References
Vaz G, Roussouly P, Berthonnaud E, Dimnet J (2002) Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J 11:80–87
Kim KT, Lee SH, Suk KS, Lee JH, Jeong BO (2012) Outcome of pedicle subtraction osteotomies for fixed sagittal imbalance of multiple etiologies. A retrospective review of 140 patients. Spine (Phila Pa 1976) 37(19):1667–1675
Lamartina C, Berjano P, Petruzzi M, Sinigaglia A, Casero G, Cecchinato R, Damilano M, Bassani R (2012) Criteria to restore the sagittal balance in deformity and degenerative spondylolisthesis. Eur Spine J 21(Suppl 1):S27–S31
Yang BP, Ondra SL (2006) A method for calculating the exact angle required during pedicle subtraction osteotomy for fixed sagittal deformity: comparison with the trigonometric method. Operative Neurosurgery 4(59):458–463
Le Huec JC, Leijssen P, Duarte M, Aunoble S (2011) Thoracolumbar imbalance analysis for osteotomy planification using a new method: FBI technique. Eur Spine J 20(Suppl 5):S669–S680
Rose PS, Bridwell KH, Lenke LG, Cronen GA, Mulconrey DS, Buchowski JM, Kim YJ (2009) Role of pelvic incidence, thoracic kyphosis, and patient factors on sagittal plane correction following pedicle subtraction osteotomy. Spine (Phila Pa 1976) 34(8):785–791
Ondra SL, Marzouk S, Koski T, Silva F, Salehi S (2006) Mathematical calculation of pedicle subtraction osteotomy size to allow precision correction of fixed sagittal deformity. Spine (Phila Pa 1976) 31:E973–E979
Legaye J, Duval-Beaupère G, Hecquet J, Marty C (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7:99–103
Hyun SJ, Rhim SC (2010) Clinical outcomes and complications after pedicle subtraction osteotomy for fixed sagittal imbalance patients: a long-term follow-up data. J Korean Neurosurg Soc 47:95–101
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Berjano, P., Cecchinato, R., Damilano, M. et al. Preoperative calculation of the necessary correction in sagittal imbalance surgery: validation of three predictive methods. Eur Spine J 22 (Suppl 6), 847–852 (2013). https://doi.org/10.1007/s00586-013-3025-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-013-3025-9