Abstract
Purpose
Transoral resection of the odontoid has been accepted as a standard procedure to decompress the cervicomedullary junction during the past several decades. The endoscopic transnasal odontoidectomy is emerging as a feasible surgical alternative to conventional microscopic transoral approach. In this article, we describe several operative nuances and pearls from our experience about this approach, which provided successful decompression.
Methods
From September 2009 to April 2010, three consecutive patients with basilar invagination, of which the etiology was congenital osseous malformations, underwent endoscopic transnasal odontoidectomy. All patients presented with myelopathy. The last two cases also received occipitocervical fixation and bone fusion during the same surgical episode to ensure stability.
Results
All the patients were extubated after recovery from anesthesia and allowed oral food intake the next day. Cerebrospinal fluid rhinorrhea was found in the second case and cured by continuous lumber drainage of cerebrospinal fluid. No infection was noted. The average follow-up time was more than 24 months. Remarkable neurological recovery was observed postoperative in all patients.
Conclusion
The endoscopic transnasal odontoidectomy is a feasible approach for anterior decompression of pathology at the cervicomedullary junction. The advantages over the standard transoral odontoidectomy include elimination of risk of tongue swelling and teeth damaging, improvement of visualization, alleviation of prolonged intubation, reduction of need for enteral tube feeding and less risk of affecting phonation. The minimally invasive access and faster recovery associated with this technique make it a valid alternative for decompression of the ventral side of the cervicomedullary junction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Basilar invagination is a developmental anomaly of the craniovertebral junction (CVJ) due to several etiologies, in which the brainstem and/or the cervicomedullary junction are compressed from the ventral side by the odontoid process [1, 2]. The surgical treatment remains challenging because of the complex anatomic and biomechanical characteristics of this region [3, 4].
During the past several decades, transoral resection of the odontoid followed by posterior fixation procedures has been accepted as a standard procedure [3–7]. Despite the fact that such an approach provides a direct route to the odontoid process, it presents several disadvantages, including the deepness of the surgical corridor, the risk of contamination by bacterial flora due to traversing the oral cavity, the risk of tongue and teeth damage, prolonged postoperative intubation, the need for nasogastric tube feeding of the patient after surgery and possible impacts on phonation as the result of soft palate splitting or hard palate resection in some cases [8–11].
In recent years, with the rapid development of endoscope technology, pure endoscopic transnasal odontoidectomy could be performed successfully to treat cervicomedullary compression with basilar invagination [11–21]. At present, there are only a limited number of patients having been operated on in a few specialized centers. The possibilities, safety, and limits of this approach are still under investigation. We want to present our experiences about three patients with basilar invagination successfully treated by pure endoscopic transnasal odontoidectomy in our department. The purpose of this report is to validate the feasibility of the approach and describe several operative nuances and pearls based on our experiences.
Illustrative cases
Case 1
A 53-year-old man had stiff neck for 5 years and unsteady gait for 1 year. On admission, the patient had grade 4 of 5 motor strength with increased tone in all extremities. Sensory examination was normal except right hand numbness. He had bilateral positive Hoffmann and Babinski signs.
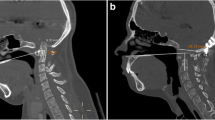
His MRI demonstrated basilar invagination with subsequent compression at the ventral aspect of the lower medulla (Fig. 1a). His cervical reconstruction CT scans revealed basilar invagination, atlas assimilation and C2/C3 interbody fusion (Klippel–Feil syndrome) (Fig. 1b). His cervical dynamic radiographs demonstrated there was no change of AADI (anterior atlantodental interval) on flexion/extension films.
Case 1: a Preoperative magnetic resonance imaging (MRI) revealing basilar invagination, resulting in compression at the cervicomedullary junction from the ventral aspect. b Preoperative sagittal computed tomographic (CT) scans revealing the tip of the odontoid extended above the Chamberlain line 11.6 mm. Atlanto-occipital assimilation and C2/C3 interbody fusion (Klippel–Feil syndrome). c, d: Five days postoperative, MRI and sagittal CT scans demonstrated that the odontoid had been drilled off. e 30 months postoperative, MRI showed the ventral cervicomedullary compression was completely relieved, and the sphenoid sinus was left intact. f, g 30 months postoperative, dynamic cervical X film demonstrated good stability. h, i The right and left lateral atlantoaxial articulations(LAA) were flat without listhesis of the inferior and superior facets (red arrow). j Three-dimensional reconstruction CT scans showing that the superior surfaces of AAF were generally flat
Case 2
A 42-year-old woman had neck pain more than 10 years and progressive declined muscle strength of all limbs for 3 years. She also had difficulty in walking and had bladder urgency for 1 year. On admission, short neck with low hairline and restricted neck movements were observed. Sensory examination disclosed the impaired senses of pain and thermal in her right side. The patient had grade 4+ of 5 motor strength in her left limbs and 4 of 5 in right limbs with increased tone in all limbs. She had bilateral positive Hoffmann and Babinski signs.
Her MRI demonstrated basilar invagination with subsequent compression at the ventral aspect of the lower medulla. From C2 to C6, the spinal cord swelled (Fig. 2a). Her cervical reconstruction CT scans revealed basilar invagination, partial atlas assimilation. The odontoid displaced to the left and prolapsed into the foramen magnum (Fig. 2b).
Case 2: a Preoperative magnetic resonance imaging (MRI) revealing basilar invagination, resulting in compression at the cervicomedullary junction from the ventral aspect. The spinal cord swelled from C2 to C6. b Preoperative sagittal computed tomographic (CT) scans revealing the tip of the odontoid extended above the Chamberlain line 17 mm atlanto-occipital assimilation. c Lateral fluoroscopy showed that the probe just above the dura after the odontoid was totally removed. d, e Lateral fluoroscopy and photo during operation showed the occiput-C3–C4 fixation and bone fusion. f Sagittal CT demonstrated that the odontoid had been drilled off 1 month postoperative. g One month postoperative, MRI demonstrated that the ventral cervicomedullary compression was completely relieved and the spinal cord swelling decreased
Case 3
A 59-year-old woman had stiff neck for more than 7 years and progressive bilateral upper extremities numbness for 5 years, especially in her hands. On admission, short neck with low hairline was observed. Sensory examination disclosed the impaired senses of pain and thermal in her left up extremity.
Her MRI demonstrated basilar invagination with subsequent compression at the ventral aspect of the lower medulla (Fig. 3a). Her cervical reconstruction CT scans revealed basilar invagination, atlas assimilation (Fig. 3b).
Case 3: a Preoperative magnetic resonance imaging (MRI) revealing basilar invagination, resulting in compression at the cervicomedullary junction from the ventral aspect. b Preoperative sagittal computed tomographic (CT) scans revealing the tip of the odontoid extended above the Chamberlain line 17.2 mm. c Two weeks postoperative, MRI showed the ventral cervicomedullary compression was completely relieved. d Two days postoperative, sagittal computed tomographic (CT) scans revealing that the odontoid had been drilled off
The clinical symptoms of the three patients were evaluated using the Japanese Orthopaedic Association (JOA) score for the evaluation of cervical myelopathy [22]. The clinical characteristics of patients undergoing endoscopic transnasal odontoidectomy for basilar invagination are shown in Table 1.
Methods
Surgical preparations
Before surgery, all the three patients were started on halo traction several days and proven to be irreducible type. They underwent preoperative thin-cut CT and 3-mm sliced MRI, which are used for frameless stereotactic image guidance system during the procedure. After fiberoptic oral intubation, the patient was placed in supine position on a standard operating table with the head fixed with Mayfield headholder. The operating table was tilted 15° to the right to facilitate the right hand surgeon to operate. The setup of the operating room is illustrated in Fig. 4. We used rigid-rod endoscopes 4 mm in diameter with lengths of 18 cm and lens angles of 0° and 30°, mounted to a digital video camera system (Karl Storz GmbH & Co., Tuttlingen, Germany).
Artist’s illustration of operating room setup. The patient was placed in supine position with his head slight flexion and a mild tilt toward the operator. The operators stood on the right side of the patient. The scrub nurse was positioned cephalad to the patient. C-arm fluoroscope was set up for a lateral view of the region of interest and was kept available throughout the procedure. Endoscopic and navigation monitors were both placed cephalad to the patient (A operator, B assistant, C scrub nurse, D anesthetist, ① navigation monitor, ② endoscopic monitor)
Surgical techniques
All the surgeries were performed via two nostrils endoscopic techniques. The bilateral middle turbinates, inferior turbinates and the sphenoid sinus anterior wall were not resected. The bilateral inferior turbinates were lateralized and the posterior 1 cm of the nasal septum was removed (Fig. 5b) to enlarge the choana for a wider exposure and to facilitate bilateral application of instrumentations without continuously pushing the septum into the endoscope and compromising visualization. The surgical trajectory could be confirmed by the steep downward angle to the lower clivus and was rechecked with neuronavigation. Then, the fascia of the posterior nasopharynx was opened with an inverted U incision (Fig. 5c), with the superior extent at the clivus, the lateral margins just medial to the Eustachian tubes and its base at the level of the C2 vertebral body. The flap was elevated and reflected caudally to the level of the soft palate. The longus colli and capitis muscles were reflected laterally. The ventral portion of the foramen magnum (low part clivus and assimilated C1) was visualized and removed with the use of high-speed pneumatic drills (Medtronic Midas Rex Legend, USA) and Kerrison rongeurs. The underlying angled odontoid process now could be followed. After the odontoid process was cored out centrally with 3 mm diamond high-speed pneumatic drill bit, the remaining cortical shell was removed by the drill and Kerrison punches in turn along the vertical margins (Fig. 5d). After the final piece of the odontoid shell cap was taken out, decompression was confirmed by a re-expanded dural sac with pulsation. Also, lateral fluoroscopy could be applied to evaluate the extent of surgical decompression by placing a probe just above the dura (Fig. 2c). The operative cavity was covered with gelatin foam and the muscle-mucosal flap was replaced and fixed with fibrin glue, closing the surgical field. The bilateral nasal cavities were packed with expansion sponge.
a The choana was enlarged although the bilateral middle turbinates, inferior turbinates and the sphenoid sinus anterior wall were not resected. b The posterior 1 cm of the nasal septum was removed to enlarge the choana to facilitate bilateral application of instrumentation. c The fascia of the posterior nasopharynx was opened with an inverted U incision. The superior extent is at the clivus and the lateral margins just medial to the Eustachian tubes. d The ligaments and dura were seen after most of the odontoid was removed (ET Eustachian tube, iwsphs inferior wall of the sphenoid sinus, NS Nasal septum, RPhx rhinopharynx, sp soft plate, Od odontoid, Lig ligaments, S suction, P punche)
For case 2, there was CSF leakage during the surgery because the adhesion between the odontoid shell cap and the dura mater was too tight (Fig. 6). Some autologous fat graft harvested from the abdominal wall was taken into the cavity fixed with fibrin glue to repair the dural defect (Fig. 7). The mucosal flap created at the beginning of the operation was replaced in its original site at the end of the procedure and fibrin glue could be used to seal the edges.
For case 1, the patient refused the occipitocervical fixation and only received the anterior decompression not combined with any posterior procedure. For cases 2 and 3, both the patients received occipitocervical fixation and bone fusion during the same surgical episode (Fig. 2e).
Results
All the three patients were extubated and allowed oral food intake the next day. The expansion sponge packed in the nasal cavities was removed the third day. Remarkable neurofunction recovery was observed during the follow-up. The JOA score of each patient was elevated from preoperative 12, 8, 15 to postoperative 17, 16, 17. CSF rhinorrhea was found in case 2 and she received lumbar puncture and continuous drainage of cerebrospinal fluid for 10 days. No infection was noted during the CSF drainage. The postoperative reconstruction CT scans demonstrated that the odontoid had been drilled off (Figs. 1d, 2f, 3d) and the postoperative MRI showed that the ventral cervicomedullary compression was completely relieved (Figs. 1c, e, 2g, 3c).
Discussion
During the past several decades, the transoral approach has been widely accepted as the standard approach for the resection of odontoid to decompress the ventral side of cervicomedullary junction [3–7]. Since Kassam et al. [12] firstly reported the endoscopic transnasal odontoidectomy in 2005, there have been several case reports demonstrating the feasibility and effectiveness of this new approach [11–20]. We acknowledged the excellent work in cadavers and the prior cases in the literature, in which the authors described the endoscopic transnasal approach and detailed the technical nuances [10, 23–25]. In addition we would like to describe several pearls from our own experience to date. (1) We did not open the sphenoid sinus, preserved the integrity of the middle turbinate, which was different from Kassam [12] and Leng’s [16] reports and made the operation even less invasive. We found that it could obtain adequate operative space because the inverted U-shaped incision sits below the sphenoid sinus. Preservation of both middle turbinates can help to keep the nasal cavities moist, restore normal laminar flow of air through the nose and minimize postoperative crusting [15]. (2) All the surgeries were performed via two nostrils endoscopic techniques, the endoscope and suction in one nasal cavity and a dissecting instrument or drill in the other, which was different from Wu’s [11] report. Two nostrils techniques can make the instruments move smoothly to facilitate maneuver. Wu et al. used one nostril for the approach and placed a nasal speculum between the middle turbinate and the bony part of the nasal septum. We think that was the reason why the author drew the conclusion that endonasal endoscopic approach was narrow. We summarized the reported cases that underwent endoscopic transnasal odontoidectomy in the previous literatures and made a comparative study of the surgical methods, techniques, results and complications in Table 2. (3) We had one case encountered with CSF leakage. The potential for CSF leakage with the endoscopic transnasal approach for odontoid resection is quite low. It is shown in Table 2 that only 1 out of 21 cases encountered intraoperative minor cerebrospinal fluid leakage. And the leakage could be repaired with fat graft and tissue glue. No postoperative cerebrospinal fluid leak was further observed, and no intra- or postoperative lumbar drainage was applied [11]. Regarding our case, there were two reasons for CSF leakage: ① The severe compression from odontoid process led to the dura and ligaments behind the tip of odontoid becoming very thin. ② The improper manipulation of the last piece of bony elements of odontoid when it was free-floating. Sharp dissection with rotatable scissors was better than pulling out with Kerrison punches based on our experiences. The latter might cause tear of the thin dura. It was our belief that the CSF leakage during the operation was not a disaster, although suturing the dura and the nasopharynx mucosa with conventional tools through the nose was very difficult [12]. We had experiences on endoscopic CSF-leakage repairing, which came from lots of cases we had performed, in which the endoscopic expanded transnasal approach was used to treat other diseases, such as craniopharyngioma, clival chordoma and giant pituitary adenomas. The techniques used to deal with the CSF leakage include packing with a fat graft, use of fibrin glue, rotating a nasal mucosal or turbinate flap over the pharyngeal incision site, and placement of a lumbar drain. Case 2 verified these methods were efficacious. (4) Intraoperative C-arm fluoroscope and Frameless stereotactic navigation aided to localize the key structures, significantly contributed to a complete, accurate, and safe resection of the osseous mass [11, 12, 16].
As a general rule, basilar invagination treated with transoral odontoidectomy usually is followed by posterior occipitocervical stabilization [3, 4, 26–28]. Neither the transoral approach nor the endoscopic transnasal approach will alter the indication for posterior procedures [11]. Goel et al. studied 190 surgically treated patients with basilar invagination. In his opinion, simultaneous dorsal fixation following a transoral decompression is not mandatory and in some patients fixation is required but can safely be staged [3]. However, if the patient with basilar invagination due to congenital osseous malformations presents stability preoperatively, the risks of creating craniovertebral instability with odontoidectomy have never been fully delineated. Dickman et al. [29] studied the influence of transoral odontoid resection on stability of the craniovertebral junction. Patients with congenital osseous malformations were more likely to maintain occipitocervical stability after odontoidectomy. Our first case refused to receive occipitocervical fixation during the same surgical episode. Interestingly, the patient remained stable without any complaint of neck pain during the 30 months follow-up. Yin et al. [30] studied the 3D configuration and morphometric data of obliquity of the lateral atlantoaxial articulations (LAA) in congenital anomaly with occipitalization of atlas. The LAA were the weight-bearing positions in normal individuals. They believed that instability at the C1–C2 junction in congenital anomaly with atlas assimilation was a direct result of the anteversion of AAF. Variations in the anatomy of the LAA could logically account for the C1–C2 instability. For case 1, the lateral masses and the superior surfaces of AAF were generally flat without listhesis of the inferior and superior facets (Fig. 1h, i, j), it might be the reason why the patient was stable after odontoidectomy. This case also gave us a hint that some patients may not need to undergo posterior fixation [19]. A larger number of cases with more detailed clinical and radiographic data are needed to validate the idea. Of course, the patient not receiving fixation should be followed up carefully. Excessive pain and spasm of the neck muscles and suboccipital radicular pain may form the primary indication for fixation in these patients [3, 19, 25].
Compared to our previous transoral surgery [31], the endoscopic transnasal odontoidectomy has the following advantages: (1) The property of endoscopy is to provide a wider view of the surgical field and a more close-up multi-angled vision, thus improving visualization in deep surgical corridors [10, 12, 13, 16]. (2) The use of mouth retractors is no longer necessary, which eliminates the risk of tongue swelling and teeth damaging [10, 11, 15, 18]. (3) The transnasal approach decreases the risk of tongue and posterior oropharyngeal wall swelling, ameliorates the need for nasogastric tube feeding and prolonged extubation or tracheostomy [11, 12, 21, 31]. Our patients were all extubated after recovery from anesthesia and allowed oral food intake the next day. This led to an expeditious recovery and hospital discharge. (4) The incision is above the oropharynx. This may reduce the infection risk, as the wound is not constantly bathed in saliva [11, 12]. (5) The endoscopic transnasal approach does not need the soft palate splitting or the hard palate resection, thus minimising the risk of postoperative dysphonia or velopharyngeal insufficiency (VPI) [15, 16, 31].
In recent years, more aggressive posterior reduction including decompression, instrumentation, realignment and fusion has been used to treat basilar invagination, which reduced the need of anterior decompression [32–36]. We believe that the value of the anterior approach decompression can never be underestimated, although some patients may benefit from the posterior reduction. In the future, endoscopic anterior decompression and posterior reduction will be the two directions of development to treat basilar invagination.
Conclusion
The endoscopic endonasal odontoidectomy is a feasible approach for anterior decompression of pathology at the cervicomedullary junction. This approach provides an excellent surgical route, with many advantages compared to the conventional trans-oral approach, potentially avoids serious intra-operative and postoperative complications. The minimally invasive access and the fewer complications associated with this technique make it a valid alternative for decompression of the ventral side of the craniovertebral junction.
References
Klimo P Jr, Rao G, Brockmeyer D (2007) Congenital anomalies of the cervical spine. Neurosurg Clin N Am 18(3):463–478
Menezes AH (2008) Craniocervical developmental anatomy and its implications. Childs Nerv Syst 24(10):1109–1122
Goel A, Bhatjiwale M, Desai K (1998) Basilar invagination: a study based on 190 surgically treated patients. J Neurosurg 88(6):962–968
Menezes AH, VanGilder JC (1988) Transoral-transpharyngeal approach to the anterior craniocervical junction: ten-year experience with 72 patients. J Neurosurg 69(6):895–903
Crockard HA (1993) Transoral approach to intra/extradural tumors. In: Sekhar LN, Janecka I (eds) Surgery of cranial base tumors. Raven Press, New York, pp 225–234
Dickman CA, Spetzler RF, Sonntag VK (1998) Surgery of the craniovertebral junction. Thieme, New York
Sawin PD, Menezes AH (1997) Basilar invagination in osteogenesis imperfecta and related osteochondrodysplasias: medical and surgical management. J Neurosurg 86(6):950–960
Crockard HA (1995) Transoral surgery: some lessons learned. Br J Neurosurg 9:283–293
Di Lorenzo N, Fortuna A, Guidetti B (1982) Craniovertebral junction malformations. Clinicoradiological findings, long-term results, and surgical indications in 63 cases. J Neurosurg 57:603–608
Messina A, Bruno MC, Decq P, Coste A, Cavallo LM, Divittis ED, Cappabianca P, Tschabitscher M (2007) Pure endoscopic endonasal odontoidectomy: anatomical study. Neurosurg Rev 30:189–194
Wu JC, Huang WC, Cheng H, Liang ML, Hou CY, Wong TT, Shih YH, Yen YS (2008) Endoscopic transnasal transclival odontoidectomy: a new approach to decompression: technical case report. Neurosurgery 63:(ons suppl 1) onse94–96
Kassam AB, Snyderman C, Gardner P, Carrau R, Spiro R (2005) The expanded endonasal approach: a fully endoscopic transnasal approach and resection of the odontoid process: technical case report. Neurosurgery 57:E213 (discussion E213)
Kassam AB, Abla A, Snyderman C, Carrau R, Spiro R (2005) An endoscopic transnasal odontoidectomy to treat cervicomedullary compression with basilar invagination. Neurosurgery 8(4):198–204
Nayak JV, Gardner PA, Vescan AD, Carrau R, Kassam AB, Snyderman C (2007) Experience with the expanded endonasal approach for resection of the odontoid process in rheumatoid disease. Am J Rhinol 21:601–606
Laufer I, Greenfield JP, Anand VK, Hartl R, Schwartz TH (2008) Endonasal endoscopic resection of the odontoid in a non-achondroplastic dwarf with juvenile rheumatoid arthritis, feasibility of the approach and utility of intraoperative iso-C 3D navigation. J Neurosurg Spine 8:366–370
Leng LZ, Anand VK, Hartl R, Schwartz TH (2009) Endonasal endoscopic resection of an Os Odontoideum to decompress the cervicomedullary junction: a minimal access surgical technique. Spine 34(4):E139–E143
Gempt J, Lehmberg J, Meyer B, Stoffel M (2010) Endoscopic transnasal resection of the odontoid in a patient with severe brainstem compression. Acta Neurochir 152:559–560
Hankingson TC, Grunstein E, Gardner P, Spinks TJ (2010) Transnasal odontoid resection followed by posterior decompression and occipitocervical fusion in children with Chiari malformation Type I and ventral brainstem compression. J Neurosurg Pediatr 5:549–553
Scholtes F, Signorelli F, McLaughlin N, Lavigne F, Bojanowski MW (2011) Endoscopic endonasal resection of the odontoid process as a standalone decompressive procedure for basilar invagination in Chiari type I malformation. Minim Invasive Neurosurg 54(4):179–182
Cornelius JF, Kania R, Bostelmann R, Herman P, George B (2011) Transnasal endoscopic odontoidectomy after occipito-cervical fusion during the same operative setting-technical note. Neurosurg Rev 34(1):115–121
Grammatica A, Bonali M, Ruscitti F, Marchioni D, Pinna G, Cunsolo EM, Presutti L (2011) Transnasal endoscopic removal of malformation of the odontoid process in a patient with type I Arnold-Chiari malformation: a case report. Acta Otorhinolaryngol Ital 31:248–252
Japanese Orthopaedic Association (1994) Scoring system for cervical myelopathy. J Jpn Orthop Assoc 68:490–503 (in Japanese)
Alfieri A, Jho HD, Tschabitscher M (2002) Endoscopic endonasal approach to the ventral cranio-cervical junction: anatomical study. Acta Neurochir (Wien) 144:219–225 (discussion 225)
Cavallo LM, Cappabianca P, Messina A, Esposito F, Stella L, de Divitiis E, Tshabitscher M (2007) The extended endoscopic endonasal approach to the clivus and cranio-vertebral junction: anatomical study. Childs Nerv Syst 23:665–671
Baird CJ, Conway JE, Sciubba DM, Prevedello DM, Quinones-Hinojosa A, Kassam AB (2009) Radiographic and anatomic basis of endoscopic anterior craniocervical decompression: a comparison of endonasal, transoral, and transcervical approaches. Neurosurgery. 65(6 Suppl):158–163 (discussion 63–64)
Menezes AH (2008) Surgical approaches: postoperative care and complications “transoral-transpalatopharyngeal approach to the craniocervical junction. Childs NervSyst. 24(10):1187–1193
Hwang SW, Heilman CB, Riesenburger RI, Kryzanski J (2008) C1–C2 arthrodesis after transoral odontoidectomy and suboccipital craniectomy for ventral brain stem compression in Chiari I patients. Eur Spine J 17(9):1211–1217
Zileli M, Cagli S (2002) Combined anterior and posterior approach for managing basilar invagination associated with type I Chiari malformation. J Spinal Disord Tech 15(4):284–289
Dickman CA, Locantro J, Fessler RG (1992) The influence of transoral odontoid resection on stability of the craniovertebral junction. J Neurosurg 77(10):525–530
Yin YH, Yu XG, Zhou DB, Wang P, Zhang YZ, Ma XD, Bu B (2012) Three-dimensional configuration and morphometric analysis of the lateral atlantoaxial articulation in congenital anomaly with occipitalization of the atlas. Spine 37(3):E170–E173
Ye G, Xiaobiao Z, Wensheng L, Xiaoxin J, Yong Y, Fan H, Wenlong X (2009) Microsurgical transoral odontoidectomy combined with neuronavigation. Chin J Microsurg 32(6):516–517
Wu JC, Mummaneni P, EI-Sayed IH (2011) Diseases of the odontoid and craniovertebral junction with management by endoscopic approaches. Otolaryngol Clin N Am 44:1029–1042
Goel A (2004) Treatment of basilar invagination by atlantoaxial joint distraction and direct lateral mass fixation. J Neurosurg Spine 1(3):281–286
Abumi K, Takada T, Shono Y, Kaneda K, Fujiya M (1999) Posterior occipitocervical reconstruction using cervical pedicle screws and plate-rod systems. Spine (Phila Pa 1976) 24(14):1425–1434
Jian FZ, Chen Z, Wrede KH, Samii M, Ling F (2010) Direct posterior reduction and fixation for the treatment of basilar invagination with atlantoaxial dislocation. Neurosurgery 66(4):678–687 (discussion 687)
Hsu W, Zaidi HA, Suk I, Gokaslan ZL, Wolinsky JP (2010) A new technique for intraoperative reduction of occipitocervical instability. Neurosurgery 66(6 Suppl Operative):319–323 (discussion 323–324)
Acknowledgments
The authors thank Dr. He Yi-zhou for his help in drawing the illustrations for this paper.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yu, Y., Wang, X., Zhang, X. et al. Endoscopic transnasal odontoidectomy to treat basilar invagination with congenital osseous malformations. Eur Spine J 22, 1127–1136 (2013). https://doi.org/10.1007/s00586-012-2605-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-012-2605-4