Abstract
Introduction
This study aimed to compare patients undergoing deep extensor muscle-preserving laminoplasty and conventional open-door laminoplasty for the treatment of cervical spondylotic myelopathy (CSM). We specifically assessed axial pain, cervical spine function, and quality of life (QOL) with a minimum follow-up period of 3 years.
Patients and methods
Ninety patients were divided into two groups and underwent either conventional open-door laminoplasty (CL group) or laminoplasty using the deep extensor muscle-preserving approach (MP group). The latter approach was undertaken by preserving the multifidus and semispinalis cervicis attachments followed by open-door laminoplasty and resuturing of the bisected spinous processes at each decompression level. The mean follow-up period was 7.7 years (range, 36–128 months). Preoperative and follow-up evaluations included the Japanese Orthopaedic Association (JOA) score, a tentative version of the JOA Cervical Myelopathy Evaluation Questionnaire (JOACMEQ) including cervical spine function and QOL, and a visual analog scale (VAS) for axial pain. Radiological analyses included cervical lordosis and flexion–extension range of motion (C2–7), as well as deep extensor muscle areas on axial magnetic resonance imaging (MRI).
Results
The mean number of decompressed laminae was 3.9 and 3.3 in CL and MP groups, respectively, which was statistically equivalent. Japanese Orthopaedic Association recovery was statistically equivalent between the two groups. The MP group demonstrated a superior QOL score (57 vs. 46 %) compared with the CL group at final follow-up (p < 0.05). Mean VAS scores at final follow-up were 2.2 and 4.3 in MP and CL groups, respectively (p < 0.05). Cervical lordosis and flexion–extension range of motion were statistically equivalent. The percentage deep muscle area on MRI was significantly lesser in the CL group compared with the MP group (58 vs. 102 %; p < 0.01).
Conclusion
We demonstrated the superiority of deep extensor muscle-preserving laminoplasty in terms of postoperative axial pain, QOL, and prevention of atrophy of the deep extensor muscles over conventional open-door laminoplasty for the treatment of CSM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Posterior cervical decompression surgery is a common surgical modality to gain a stable neurological improvement in patients with cervical spinal cord compression [3, 6, 9, 12, 13]. This has evolved from extensive laminectomy to extensive or selective laminoplasty for the prevention of kyphotic deformity and postlaminectomy membrane formation [12]. Several laminoplasty techniques have been introduced, but there was no relationship between the type of laminoplasty and neurological recovery, changes in spinal alignment, and cervical range of motion [12].
The axial pain explained by persistent neck and shoulder girdle pain is a notable postoperative complication after posterior cervical spine surgery [5, 8, 12, 21]. The overall incidence of such axial pain varied markedly from 6 to 60 % [5, 8, 12, 21]. Several authors have clinically evaluated the incidence of axial pain, radiological alignment, range of motion, and neurological outcome in patients who underwent laminoplasty [1, 5, 8, 19–21, 23, 24]. Nevertheless, the relationship between axial pain and those parameters is incompletely understood.
To decrease axial pain and preserve cervical mobility and spinal curvature, a surgical approach preserving the deep extensor muscles was developed and applied by Shiraishi et al. [14] in 2002. This surgical technique included preservation of the multifidus and semispinalis muscle attachments to spinous processes using an interlaminar approach [14]. We have applied this surgical approach for conventional open-door laminoplasty since 2003. Our previous retrospective cohort study compared the minimum 2-year outcome of this muscle-preserving technique with conventional open-door laminoplasty in a combined population of patients with ossification of posterior longitudinal ligament (OPLL) and cervical spondylotic myelopathy (CSM) [10]. That study concluded that in patients with a minimum follow-up period of 2 years, those undergoing extensor muscle-preserving laminoplasty demonstrated statistically superior cervical spine function and quality of life (QOL) compared with those undergoing conventional laminoplasty. That study also demonstrated less axial pain and prevention of atrophy of deep extensor muscles in patients undergoing extensor muscle-preserving laminoplasty. However, there was a major study limitation of the combined patient background of OPLL and CSM. These disorders were basically different; therefore, they should be separately analyzed. Additionally, the decompression range of muscle-preserving group in that study was shorter than that of the conventional laminoplasty group (mean laminae, 3.7 vs. 5.4); hence, the invasiveness of laminoplasty was less than that in the latter group. Further study is necessitated with a specific group of CSM patients with a longer follow-up period.
The objective of the present study was to compare deep extensor muscle-preserving laminoplasty with conventional open-door laminoplasty in the treatment of CSM alone, by specifically assessing axial pain, cervical spine function, and QOL.
Materials and methods
Patient demographics
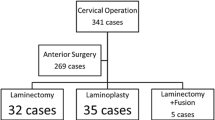
Between August 2000 and July 2008, 90 patients with CSM underwent cervical laminoplasty either using the conventional open-door technique (CL group, 27 patients) or using the deep extensor muscle-preserving technique (MP group, 63 patients). The latter procedure was performed according to the method of Shiraishi et al. [10, 14–17] i.e., preserving the multifidus and semispinalis cervicis muscles. Patients were allocated into two groups by date of surgery: 2000–2002 for the CL group and 2003–2008 for the MP group. The mean follow-up periods were 104 (range, 54–128) and 66 (range, 36–95) months in the CL and MP groups, respectively. There were 67 males and 23 females [mean age at surgery, 64 years (range, 38–87 years)]. No patients had segmental instability or kyphosis. Most patients had a developmental narrow spinal canal, and decompressive laminae were distributed from C2 to T1 levels. The number of decompressed lamina was 3.9 ± 1.2 in the CL group, and 3.3 ± 0.8 in the MP group, and this difference was not significant. The number of patients in whom C2 was included in the decompression area was three in the CL group and one in the MP group. Additionally, the number of patients in whom C7 or T1 levels were included was six in the CL group and seven in the MP group. There were no statistical differences between the two groups in terms of C2 and C7 (or T1) inclusions (Fisher’s exact test). Typical decompression patterns were C3–C6/C7 in the CL group and C4–6 in the MP group. The preoperative background data of the two surgical groups are demonstrated in Table 1.
Surgical procedures
The method of conventional open-door laminoplasty performed in this study has been reported [10]. Briefly, the laminae were cut at the midline using a surgical burr, and lateral gutters created at the medial border of the facet joints bilaterally. Then, the right and left halves of the laminae were lifted and bilaterally opened leaving the sutures joining the ligamentum flavum to the lateral muscles. A bone graft was not performed at the lateral gutters. In this group, the deep extensor muscles were not repaired and only the superficial ligamentum nuchae was repaired. The laminoplasty in the MP group was performed using a deep extensor muscle-preserving approach in addition to a previously described technique for open-door laminoplasty [10]. After incision of the nuchal ligament to expose the spinous processes along the midline, consecutive laminae were exposed while preserving the multifidus and semispinalis muscles [10, 14] (Fig. 1). The spinous processes were vertically divided using a surgical burr or osteotome with the preservation of extensor muscle attachments, and were transversely osteotomized at the base of spinous processes. Stay sutures were placed through the bone and extensor muscles, which were retracted laterally. After the open-door laminoplasty was completed, reconstruction of extensor muscles was performed with tight suturing of the bisected spinous processes. In CL and MP groups, self-retaining retractors were used to an equal extent during the decompression procedure. The mean operation time was approximately 75 min in the CL group, with the additional muscle-preserving procedure taking an additional 5–10 min. Postoperatively, patients did not apply a collar and mobilized their necks freely. Isometric cervical muscle exercises were started 3 days after surgery.
Surgical procedure of deep extensor muscle-preserving laminoplasty (bottom of figure signifies the cephalad direction of the patient). a On exposure of the spinous processes in the midline, the consecutive laminae were exposed while preserving the multifidus and semispinalis cervicis muscle. Each star signifies a spinous process. b The spinous processes were vertically bisected using a surgical burr or osteotome with the preservation of extensor muscle attachments. The stay sutures were placed through the bone for the later closure. c Open-door laminoplasty was followed by the ligamentum flavum suture to the lateral paravertebral muscles. d Reconstruction of extensor muscles with tight sutures to the bisected spinous processes (arrows)
Quantitative analyses of outcome
Preoperative and final follow-up outcome was evaluated using the Japanese Orthopaedic Association (JOA) score [7], and recovery was calculated using Hirabayashi’s method [4]. The degree of axial neck pain was evaluated using a visual analog scale (VAS; 0–10) before surgery, 6 months after surgery and at final follow-up. The mean preoperative VAS score was 5.5 ± 4.0 and 4.1 ± 3.3 in the CL and MP groups, respectively, and there was no significant difference between the two groups (p > 0.05). The cervical spine and spinal cord function, and QOL were evaluated with a tentative version of the JOA Cervical Myelopathy Evaluation Questionnaire (JOACMEQ) consisting of 24 distinct items [2, 10]. This comprised self-reported questionnaires and data expressed as a percentage of the total score (Tables 2, 3). In terms of radiographic analyses, cervical lordosis and flexion–extension range of motion (flex–ext ROM) were measured from C2 to C7 preoperatively and at final follow-up. Atrophy of the deep extensor muscles was quantified using magnetic resonance T1-weighted axial images [10]. At C4/5 and C5/6 levels, the muscle areas of the multifidus, semispinalis, and longissimus were measured as a group using Scion Image software (Scion Corporation, Frederick, MD, USA) with two image slices at each level. At each level, two measurements were averaged as the representative area data. The mean muscle areas at C4/5 and C5/6 were summed preoperatively and at follow-up, and its muscle group area at follow-up was divided by the preoperative value and expressed as the percentage to the preoperative value.
Statistical analyses
Each parameter was compared using an unpaired Student’s t test between preoperative and final follow-up data.
Results
The postoperative follow-up periods were 66 (range, 36–95) and 103 (range, 54–128) months in the MP and CL groups, respectively. The preoperative and final follow-up JOA score in the MP group was 9.3 ± 3.0 and 13.8 ± 2.0 (mean ± SD), respectively. The preoperative and final follow-up JOA score in the CL group was 9.4 ± 2.6 and 13.6 ± 2.8 (mean ± SD), respectively. The recovery of the JOA score was 60.9 % ± 19.7 and 58.0 % ± 28.2 in the MP and CL groups, respectively, and this difference was not significant (p > 0.05).
The cervical spine and spinal cord function were evaluated across 13 categories using a tentative version of JOACMEQ. These scores were 83.2 ± 12.8 and 78.7 ± 15.2 % in the MP and CL groups, respectively, at postoperative 6 months, and this difference was not significant (p > 0.05). At final follow-up, these values were 77.2 ± 22.1 and 78.1 ± 13.4 % in the MP and CL groups, respectively, which was statistically insignificant (p > 0.05). The cervical spine function comprising four items included in the respective tentative JOACMEQ was 81.9 ± 20.4 and 74.3 ± 25.2 % in the MP and CL groups, respectively, 6 months after surgery, and this difference was not significant (p > 0.05). At the final follow-up, these values were 76.8 ± 24.1 and 74.1 ± 20.1 % respectively, which was not significantly different (p > 0.05). Quality of life scores, which comprise 11 items in the tentative version of JOACMEQ, 6 months after surgery, were 57.7 ± 17.4 and 47.8 ± 18.2 % in MP and CL groups, respectively, and this difference was significant (p < 0.02). At the final follow-up, QOL scores were 57.0 ± 21.4 and 46.1 ± 18.2 % in the MP and CL groups, respectively, and this difference was significant (p < 0.05). The mean VAS scores for axial neck pain 6 months after surgery were 2.8 ± 2.5 and 4.5 ± 2.4 in the MP and CL groups, respectively. Axial pain was statistically greater in the CL group (p < 0.01). At the final follow-up, mean VAS scores were 2.2 ± 2.2 and 4.3 ± 2.4 in the MP and CL groups, respectively, which was statistically significant (p < 0.01). Complications did not occur and re-operations were not required in either group.
With respect to radiographic analyses, cervical lordosis measured from C2 to C7 levels on lateral radiographs at final follow-up was 12.8 ± 10.7° and 15.2 ± 16.8° in the MP and CL groups, respectively, which was not statistically significant (p > 0.05). Comparison of the lordosis angles before surgery and at final follow-up revealed that they were not significantly different in the MP and CL groups. The flex–ext ROM, which was normalized to the preoperative level (percentage to preoperative values), at final follow-up was 89.3 ± 69.3 and 84.3 ± 40.7 in the MP and CL groups, respectively, which was not significantly different (p > 0.05). The flex–ext ROM in the decompression range at final follow-up was 107.8 ± 77.4 and 122.5 ± 35.5 % in the MP and CL groups, respectively, and this difference was not significant.
The normalized deep extensor muscle area (percentage at follow-up/preoperative value) at final follow-up was 102.4 ± 15.2 and 57.5 ± 15.9 % in the MP and CL groups, respectively, which was significantly different (p < 0.01). This finding meant that the MP group showed less atrophy in the extensor muscles than seen in the CL group.
Representative case studies
Case 1 A 67-year-old male presented with severe cervical myelopathy due to cervical spondylosis (Fig. 2). Conventional laminoplasty from C3 to C6 levels was performed. Six years postoperatively, improvement in cervical myelopathy was maintained with a JOA score of 9–15.5 points. However, the VAS score for axial neck pain increased significantly from 2 to 8 at final follow-up. Significant atrophy of the deep extensor muscles was demonstrated on MRI with a 41 % reduction in muscle area at final follow-up.
Case 2 A 72-year-old male with CSM underwent muscle-preserving laminoplasty from C4 to C6 levels (Fig. 3). Three years postoperatively, the JOA score improved from 8.5 to 14.5, and the VAS score for axial neck pain decreased from 6 to 0. Axial MRI demonstrated preservation of deep muscle volume of approximately 91 %.
a–e A 72-year-old male received deep extensor muscle-preserving laminoplasty from C4 to C6 levels. Box arrows signify the reattached spinous processes with deep extensor muscles (c). Axial MRI demonstrates preservation of the deep extensor muscles: comparison between preoperative and follow-up scenarios (d and e, respectively)
Discussion
The present study was designed to compare the deep extensor muscle-preserving laminoplasty with conventional open-door laminoplasty in the treatment of CSM alone, by specifically assessing axial pain, cervical spine function, and QOL. In this non-randomized study setting, the background data comparison of two surgical groups demonstrated no statistical difference in terms of gender, age, preoperative JOA score, VAS of neck pain, cervical lordosis, and C2–7 radiologic range of motion (Table 1). Additionally, the number of decompressed lamina was statistically equivalent, and C2 or C7(T1) inclusion for the decompression area was not statistically different. In this controlled comparison, there was no significant difference between MP and CL groups in terms of the following: recovery of JOA score, cervical spine and spinal cord function score, and cervical spine function only. However, the QOL score of the MP group was significantly better than that of the CL group 6 months after surgery and at final follow-up. The VAS score for neck pain was significantly lower in the MP group than in the CL group. In addition, the deep extensor muscle area in the MP group was significantly greater than that in the CL group. In this controlled comparison between MP and CL groups, the MP group effectively decreased postoperative axial pain, improved QOL, and prevented atrophy in the deep extensor muscles.
There are many anatomical structures influencing the axial pain and cervical spine function: a nuchal ligament attached to C7 spinous process, deep muscles attached to C2 spinous process, and deep extensor muscles at other spinal levels. In the present study, the decompression of C2 and C7 was performed in a dome-like fashion, while preserving the muscular and ligament attachment to C2 and C7 spinous processes. The numbers of C2 and C7 (or T1) inclusion for the decompression range were statistically equivalent between two surgical groups. In this controlled setting, we postulated that the preservation of deep extensor muscles would reduce the axial pain, improve the cervical spine function and QOL, and prevent the atrophy of deep extensor muscles. The study results partially supported this hypothesis except the cervical spine function.
We speculate the reason why the deep extensor muscle repair decreases the axial pain as follows. The repair of muscular attachment to the part of the spinous process helps to maintain the blood supply to the deep extensor muscles. This positively affects the preservation of the deep extensor muscle volume, which decreases other superficial muscle stresses. Consequently, the decrease of whole muscle stress reduces the axial pain. In turn, the detachment and elevation of deep extensor muscle leads to the increase the stress of superficial muscles, resulting in the persistent axial pain.
Several minimally invasive surgical techniques have been reported for the treatment of CSM [11, 18, 22, 24]. Yukawa et al. [24] prospectively compared open-door laminoplasty (C3–C6) with skip laminectomy of C4 and C6 in terms of axial pain and cervical ROM. Although the decrease in cervical ROM and VAS score for neck pain tended to be less in skip laminectomy than that in conventional open-door laminoplasty, the difference between the two groups was not significant. Sivaraman et al. [18] also compared skip laminectomy (C4 and C6) and open-door laminoplasty (C3–C6) in terms of cervical ROM and axial pain. Skip laminectomy significantly preserved ROM in 84 % compared with 46 % in open-door laminoplasty, but the axial pain measured by the SF-12 questionnaire did not demonstrate a significant difference between the two groups. Otani et al. [11] reported upon the effectiveness of segmental partial laminectomy comprising resection of the ligamentum flavum and cephalad part of the lamina at multiple cervical segments compared with expansive open-door laminoplasty at C3–C7 levels. Both groups demonstrated statistically equivalent recovery of JOA scores, but the segmental partial laminectomy group had significantly preserved ROM in 67 % (percentage postoperative/preoperative) compared with 40 % in the expansive open-door laminoplasty group. The tendency of less axial pain and preservation of spinal alignment was demonstrated in segmental partial laminectomy, but the difference was not significant. Yabuki et al. [22] reported a small case series of endoscopic partial laminectomy at one or two spinal levels. Although a long operation time and significant learning curve were reported, the VAS score for neck pain showed low values of 2.8 and 0.8 at postoperative days 1 and 3, respectively. There were no surgical complications in ten cases in that series. According to several reports mentioned above, minimally invasive laminoplasty or partial laminectomy, in general, prevents a decrease in ROM, but there are wide variations in levels of postoperative axial pain. There are very few reports comparing minimally invasive procedures and conventional laminoplasty procedures for the treatment of CSM. The present study serves as the largest comparative study, demonstrating the superiority of deep extensor muscle-preserving laminoplasty in terms of postoperative axial pain, QOL and prevention of atrophy of the deep extensor muscles.
There were several limitations in the present study. First, patients were not randomized, but instead assigned into two groups according to operation date 2000–2002 for the CL group and 2003–2008 for the MP group. Although a randomized study design is ideal, we changed the surgical procedure from 2003 completely because of observation of less axial pain in the MP group. In spite of a non-randomized study setting, the background data comparison showed no significant difference preoperatively (Table 1). Second, the decompressive ranges in the two groups were not strictly controlled. The numbers of decompressed laminae were considered in each case on the basis of spinal levels of cord compression and degree of cervical lordosis. Consequently, the number of decompressed laminae was statistically equivalent between the two groups.
Conclusion
The two surgical cohorts of conventional open-door laminoplasty and laminoplasty using deep extensor muscle-preservation technique were compared for the treatment of CSM. The study demonstrated the superiority of deep extensor muscle-preserving laminoplasty in terms of postoperative axial pain, QOL, and prevention of atrophy of the deep extensor muscles over conventional open-door laminoplasty.
References
Chiba K, Ogawa Y, Ishii K (2006) Long-term results of expansive open-door laminoplasty for cervical myelopathy—average 14-year follow-up study. Spine 31:2998–3005
Fukui M, Chiba K, Kawakami M (2007) An outcome measure for patients with cervical myelopathy: Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire (JOACMEQ): part 1. J Orthop Sci 12:227–240
Hirabayashi K, Tomita Y, Chiba K (1999) Expansive laminoplasty for myelopathy in ossification of the longitudinal ligament. Clin Orthop 359:35–48
Hirabayashi K, Toyama Y (1997) Choice of surgical procedure for cervical ossification of the posterior longitudinal ligaments. In: Yonenobu K, Sakou T, Ono K (eds) Ossification of the posterior longitudinal ligament. Springer, Tokyo, pp 135–142
Hosono N, Sakaura H, Mukai Y (2007) The source of axial pain after cervical laminoplasty—C7 is more crucial than deep extensor muscles. Spine 32:2985–2988
Itoh T, Tsuji H (1985) Technical improvements and results of laminoplasty for compressive myelopathy in the cervical spine. Spine 10:729–736
Japanese Orthopaedic Association (1994) Scoring system for cervical myelopathy. Nippon Seikeigeka Gakkai Zasshi 68:490–503 (in Japanese)
Kawaguchi Y, Kanamori M, Ishihara H (2003) Minimum 10-year follow-up after en bloc cervical laminoplasty. Clin Orthop 411:129–139
Kawai S, Sunago K, Doi K (1988) Cervical laminoplasty (Hatori’s method). Procedure and follow-up results. Spine 13:1245–1250
Kotani Y, Abumi K, Ito M, Sudo H, Takahata M, Ohshima S, Hojo Y, Minami A (2009) Minimum 2-year outcome of cervical laminoplasty with deep extensor muscle-preserving approach: impact on cervical spine function and quality of life. Eur Spine J 18:663–671
Otani K, Sato K, Yabuki S, Iwabuchi M, Kikuchi S (2009) A segmental partial laminectomy for cervical spondylotic myelopathy. Anatomical basis and clinical outcome in comparison with expansive open-door laminoplasty. Spine 34:268–273
Ratliff JK, Cooper PR (2003) Cervical laminoplasty: a critical review. J Neurosurg (Spine3) 98:230–238
Seichi A, Takeshita K, Ohnishi I (2001) Long-term results of double-door laminoplasty for cervical stenotic myelopathy. Spine 26:479–487
Shiraishi T (2002) A new technique for exposure of the cervical spine laminae. Technical note. J Neurosurg (Spine 1) 96:122–126
Shiraishi T (2002) Skip laminectomy—a new treatment for cervical spondylotic myelopathy, preserving bilateral muscular attachments to the spinous processes: a preliminary report. Spine J 2:108–115
Shiraishi T, Fukuda K, Yato Y (2003) Results of skip laminectomy—minimum 2-year follow-up study compared with open-door laminoplasty. Spine 28:2667–2672
Shiraishi T, Yato Y (2002) New double-door laminoplasty procedure for the axis to preserve all muscular attachments to the spinous process. Technical note. Neurosurg focus 12:E9
Sivaraman A, Bhadra A, Altaf F, Singh A, Rai A, Casey A, Crawford R (2010) Skip laminectomy and laminoplasty for cervical spondylotic myelopathy. A prospective study of clinical and radiographic outcomes. J Spinal Disord Tech 23:96–100
Suk KS, Kim TK, Lee JH (2007) Sagittal alignment of the cervical spine after the laminoplasty. Spine 32:E656–E660
Takeuchi K, Yokoyama T, Aburakawa S (2005) Axial symptoms after cervical laminoplasty with C3 laminectomy compared with conventional C3–7 laminoplasty. A modified laminoplasty preserving the semispinalis cervicis inserted into axis. Spine 30:2544–2549
Wada E, Suzuki S, Kanazawa A (2001) Subtotal corpectomy versus laminoplasty for multilevel cervical spondylotic myelopathy. A long-term follow-up study over 10 years. Spine 26:1443–1448
Yabuki S, Kikuchi S (2005) Endoscopic partial laminectomy for cervical myelopathy. J Neurosurg Spine 2:170–174
Yoshida M, Tamaki T, Kawakami M (2002) Does reconstruction of posterior ligamentous complex with extensor musculature decrease axial symptoms after cervical laminoplasty? Spine 27:1414–1418
Yukawa Y, Kato F, Ito K (2007) Laminoplasty and skip laminectomy for cervical compressive myelopathy. Range of motion, postoperative neck pain, and surgical outcomes in a randomized prospective study. Spine 32:1980–1985
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kotani, Y., Abumi, K., Ito, M. et al. Impact of deep extensor muscle-preserving approach on clinical outcome of laminoplasty for cervical spondylotic myelopathy: comparative cohort study. Eur Spine J 21, 1536–1544 (2012). https://doi.org/10.1007/s00586-012-2260-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-012-2260-9