Abstract
Posterior pedicle screw fixation is now the standard treatment for surgical correction of idiopathic scoliosis and has largely replaced anterior techniques, but there have been reports describing a lordogenic effect of segmental pedicle screw instrumentation in the thoracic spine. This clinical study compared anterior dual rod instrumentation with posterior pedicle screw fixation for idiopathic thoracic lordoscoliosis, including 42 patients (7 male, 35 female; average age 16 years, range 12–34) who underwent posterior pedicle screw fixation (n = 20) or anterior dual rod instrumentation (n = 22) at two centers. The average follow-up period was 33 months (24–108 months). Inclusion criteria were a diagnosis of adolescent idiopathic scoliosis with a structural thoracic curve (Lenke 1–3) and thoracic hypokyphosis (T4–T12 < 20°). The main thoracic curve magnitude and sagittal profile on standing radiographs were evaluated. Thoracic kyphosis was significantly restored from preoperatively 10.2° to 23.4° postoperatively in the anterior group and from 7.6° to 12.9° in the posterior group (P < 0.005). Kyphosis improved significantly better in the anterior group than in the posterior group (P < 0.005). The preoperative and postoperative main thoracic curve values were 63° (48–80°) and 25.2° in the anterior group and 60.6° (50–88°) and 23.6° in the posterior group, with no significant differences between the groups. No neurological or other severe complications were observed. Anterior dual rod instrumentation in patients with thoracic lordoscoliosis allows significantly better restoration of thoracic kyphosis than posterior pedicle screw instrumentation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The aim of surgical treatment in patients with scoliosis is three-dimensional correction of the deformity. It is important to take into account not only frontal correction but also sagittal correction, to prevent progressive pathologic curvature in the unfused spine. Sagittal-plane parameters have become increasingly important in maintaining the long-term health of the spine [1, 2]. For example, segmentally flat lumbar fusions and distraction forces in the lumbar spine are associated with the development of fixed sagittal imbalance syndromes [3, 4]. Restoring sufficient thoracic kyphosis should prevent posterior sagittal imbalance and thus reduce the risk of progressive junctional kyphosis [5]. In addition, thoracic hypokyphosis may be associated with respiratory dysfunction [6–8].
Currently, anterior or posterior instrumentation can be used in the treatment of idiopathic scoliosis. Several reports have demonstrated that pedicle screws are superior for correcting scoliosis, in terms of the mean absolute degrees and percentage of curve correction, in comparison with posterior hook-and-wire or hybrid constructs [9–11]. Among the several surgical techniques available, pedicle screw instrumentation is considered to be reliable and safe [12–14], but clinical trials have reported a lordogenic effect with this form of posterior instrumentation [15–17].
Anterior fusion is still considered to be a good option and is even preferred for some types of adolescent idiopathic scoliosis curve associated with thoracic hypokyphosis. In addition, anterior fusion provides better curve correction and can save fusion levels distally [4, 18]. However, some studies have reported a postoperative decrease in pulmonary function [19, 20].
The purpose of this study was to compare anterior dual rod instrumentation with posterior pedicle screw fixation in relation to sagittal-plane parameters in patients with adolescent idiopathic scoliosis (AIS).
Methods
A total of 42 patients (7 male, 35 female) with idiopathic thoracic lordoscoliosis who underwent surgery between 2003 and 2008 in two centers were included (Tables 1, 2); retrospective and prospective data were evaluated. Twenty patients underwent posterior pedicle screw fixation using a 5.5-mm titanium rod (Expedium; DePuy Spine, Leeds, England) and 22 patients received anterior dual rod instrumentation (Halm-Liljenqvist Instrumentation; DePuy Spine) via a standard open thoracotomy. The average follow-up period was 33 months (24–108 months); the patients’ average age at surgery was 16.7 years (12–34 years). The inclusion criteria were a diagnosis of AIS with a structural thoracic curve (Lenke 1, 2 or 3) and thoracic hypokyphosis (T4–T12 < 20°). The operations were carried out by two spinal surgeons at two different institutions.
The choice of surgical approach was at the discretion of the attending surgeon, on the basis of the clinical examination and radiographs (standing anteroposterior and lateral, supine anteroposterior bending). For objective assessment of the patients’ postoperative quality of life, a validated German-language version of the SRS-22 questionnaire was completed at the last follow-up consultation [21].
Surgical techniques
Anterior correction and dual rod instrumentation was performed via double thoracotomy as described by Liljenqvist et al. [22]. After thorough disc release the lid plates and screws are placed and correction is performed with intersegmental compression routinely using the more posteriorly placed smooth 4 mm rod (in the early series 4 mm threaded Zielke rod). The segmental derotation is achieved by bringing the individually and according to the vertebral rotation displaced screw heads into one line by inserting the posterior rod. Prior to curve correction the endplates are prepared and the disc spaces are filled with morselized bone chips from the resected rib. Finally, the solid rod is bent according to the residual frontal curve and to the aimed thoracic kyphosis and is inserted into the lid-plates. Additionally either slight segmental compression (to increase kyphosis) or distraction (to decrease kyphosis) can be administered.
For the posterior approach, patients were placed in the prone position. The posterior elements of the spinal fusion levels previously decided on were exposed using subperiosteal paraspinal muscle stripping. Segmental pedicle screw fixation using polyaxial and monoaxial screws was carried out using the Weinstein approach [23]. Curve correction was achieved using the rod-rotation maneuver with over bended concave sided rod and a contoured convex rod, using the principles established by Cotrel et al. [24, 25], followed by slight convex compression and concave distraction. Finally, the frame construct was completed by spinal arthrodesis with bone graft substitute. In the posterior group, rib hump resection was performed in 12 patients.
Measurements were made on coronal and lateral radiographs of the spine with the patient standing. Curve flexibility was determined on preoperative supine side-bending films. All of the radiographic measurements were made manually by one author, independent of the surgical team.
Standing anteroposterior and lateral radiographs from the preoperative, postoperative, and final follow-up (after a minimum of 2 years) examinations were analyzed using the Cobb method on the coronal and sagittal planes [26]. The Stagnara angle for thoracic kyphosis and the posterior tangent method for cervical measurement were also used [27]. Sagittal measurements included cervical lordosis (tangents drawn at the posterior body margins of C2 and C7); thoracic kyphosis (T4–T12); thoracolumbar junction (T10–L2); lumbar lordosis (T12–L5); C7 plumbline (horizontal distance from the center of the C7 body to the posterosuperior corner of the S1 body); proximal junctional measurement (Cobb angle between the most proximal instrumented vertebra and the segment two levels cranial); distal junctional measurement (Cobb angle between the most distal instrumented vertebra and the segment two levels caudal). Positive values were used to denote kyphosis and negative values to indicate lordosis. Radiographs were also analyzed for evidence of instrumentation failure (e.g., broken implants, pullout). Pseudarthroses were identified radiographically, or their presence was inferred from failed instrumentation or progression of curvature over the instrumented levels.
Data were analyzed using SPSS version 10.0 (SAS Institute Inc., Cary, North Carolina, USA). Distributions of variables are given as means, standard deviation, and ranges. The Wilcoxon rank-sum test and Mann–Whitney test were used to compare the groups and postoperative changes between the two groups.
Results
No neurological or other severe complications were observed. One patient developed respiratory insufficiency 1 day postoperatively and underwent bronchoscopy. Two patients with anterior instrumentation experienced implant failures, with broken threaded rods (after 1 and 8 years, respectively) without significant loss of correction or clinical or radiological signs of pseudarthrosis. An adding-on phenomenon without clinical relevance occurred in one patient who underwent posterior instrumentation.
On the coronal plane, the main thoracic curve in the anterior group measured 62.2° (48–80°) preoperatively, 24.4° postoperatively, and 26.9° at final follow-up—a curve correction rate of 55% (Table 1). The main thoracic curve in the posterior group measured 60.6° (50–88°) preoperatively, 23.6° postoperatively, and 25.0° at final follow-up—a curve correction rate of 58% (Table 2). There were no significant differences between the groups.
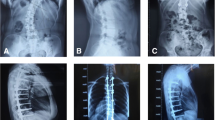
Both groups were hypokyphotic preoperatively, with no significant differences. In the anterior group, thoracic kyphosis was significantly restored from +10.2° preoperatively to +23.4° postoperatively (P < 0.005) and reached approximately normal values, with a mean of +25.0°, at final follow-up. By contrast, the patients in the posterior group were still hypokyphotic, with a mean of +16.8° at final follow-up. However, thoracic kyphosis was also significantly restored in the posterior group, from +7.6° preoperatively to +12.9° postoperatively (P < 0.005). Thoracic kyphosis improved significantly better in the anterior group than in the posterior group (P < 0.005) (Fig. 1).
All of the patients had cervical kyphosis preoperatively (+5.9° in the anterior group and +6.5° in the posterior group), with no significant differences between the groups. Both anterior and posterior instrumentation produced lordogenic effects (anterior: +5.9° preoperatively to +2.3° postoperatively and +1.5° at final follow-up; posterior: +6.5° preoperatively to +6.9° postoperatively and −0.9° at final follow-up).
Patients in both groups had a lordotic thoracolumbar junction preoperatively (anterior: −7.5°, posterior: −4.5°). No significant changes were noted in either group postoperatively or at final follow-up (anterior: −3.9° and −3.2° at final follow-up; posterior: −4.5° postoperatively and −2.2° at final follow-up; ns).
Anterior instrumentation led to the largest positive displacement in the C7 sagittal plumbline, from +13 mm preoperatively to +29 mm postoperatively (P < 0.005). Posterior instrumentation also produced positive displacement in the plumbline, from +19 mm preoperatively to +29 mm postoperatively. At the last follow-up, the displacement had decreased to +23 mm in the anterior group and +18 mm in the posterior group (Table 3).
Anterior thoracic instrumentation led to a significant increase in the proximal junctional measurement (PJM), from +3.8° preoperatively to +7.4° at final follow-up. There was also a kyphogenic trend in the posterior group (+4.6° preoperatively, +7.1° postoperatively, and +6.6° at final follow-up). There were no significant differences between the groups (Table 3).
No significant changes in the distal junctional measurement (DJM) were observed in either group between the preoperative findings and the final follow-up. However, the DJM decreased (with a more lordotic effect) after anterior and posterior instrumentation (anterior: −1.4 preoperatively, −1.9 postoperatively, −2.4 at last follow-up; posterior: −7.4 preoperatively, −9.9 postoperatively, −11.2 at last follow-up). Patients who underwent posterior instrumentation had a more lordotic DJM postoperatively (Table 3).
Lumbar lordosis increased slightly postoperatively and at final follow-up in both groups (anterior: −35.2° preoperatively, 36.2° postoperatively, −40.9° at final follow-up; posterior: −27.3° preoperatively, −24.9° postoperatively, −30.8° at final follow-up) (Table 3).
The average operating times were 195 min (120–330 min) in the anterior group and 260 min (140–320 min) in the posterior group (P = 0.001). Intraoperative blood losses were 483 mL (150–1500 mL) in the anterior group and 1,023 mL (230–2,300 mL) in the posterior group (P = 0.001).
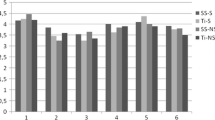
Analysis of the questionnaire responses showed that there were no significant differences between the two groups, with similar scores for pain (68 vs. 67%), general self-image (82 vs. 81%), general function (88 vs. 86%), mental health (83 vs. 83%) and patient satisfaction (89 vs. 93%) (Fig. 2).
Discussion
One of the primary goals of surgery in patients with AIS is to achieve the maximum coronal plane correction while maintaining sagittal balance. Thoracic curves often show hypokyphosis (0–20°), and it is generally agreed that the aim in surgery for idiopathic thoracic scoliosis should be to improve sagittal-plane deformities, restoring thoracic kyphosis to normal values (20–40°), as defined by Bernhardt and Bridwell [28], and maintaining lumbar lordosis and good overall sagittal balance.
Different approaches and instrumentation methods can affect postoperative sagittal-plane parameters. In a retrospective multicenter study, Sucato et al. [29] demonstrated that anterior instrumentation is the best method for restoring thoracic kyphosis in comparison with posterior techniques. Similarly, Betz et al. [4] reported that anterior instrumentation corrects hypokyphosis better than posterior techniques. This is consistent with the results presented by Potter et al. [30], who compared anterior and posterior spinal fusion in patients with Lenke 1 curves and showed that the anterior group had a significantly greater increase in thoracic kyphosis (5.7° vs. 4.4°; P = 0.004).
Vora et al. [17] observed a lordosing effect in the thoracic spine with posterior pedicle screw instrumentations. Quan et al. [15] also documented a significant correlation between reduced sagittal kyphosis and the magnitude of coronal Cobb angle correction in 49 consecutive patients with Lenke 1 main thoracic AIS who underwent single-stage posterior correction and instrumented spinal fusion with pedicle screw fixation. In contrast, Clement et al. [31] documented a mean gain of 14° of thoracic kyphosis with pedicle screw instrumentation in patients with severe preoperative hypokyphosis.
The present study compared anterior dual rod instrumentation with posterior pedicle screw fixation in the surgical treatment of idiopathic thoracic lordoscoliosis. The two groups were comparable with regard to the preoperative magnitude of the coronal Cobb angle (62.2° vs. 60.6°; n.s.) and preoperative flexibility (bending 35.7° vs. 32.9°; n.s.). A mean correction of more than 55% of the main curve was achieved with both techniques. In the literature, pedicle screw instrumentation achieves corrections as great as 75%, but at the expense of the sagittal contour, with a significant postoperative decrease in thoracic kyphosis [10, 32].
No significant loss of coronal correction was observed in either group during the follow-up period. Relative to the sagittal plane, the results show that both anterior and posterior instrumentation with the techniques described can be used to restore thoracic kyphosis (Figs. 3, 4). However, thoracic kyphosis improved significantly better in the anterior group than in the posterior group, from +10.2° preoperatively to +23.4° postoperatively (P < 0.005), reaching approximately normal values with a mean of +25.0° at final follow-up. In a previous study [33], our group documented a kyphogenic trend when an anterior dual rod instrumentation system was used to treat thoracic scoliosis in 23 patients. The better restoration provided by anterior dual rod instrumentation is probably due to using a second solid rod, allowing individual contour adjustment.
In this study the authors regularly used monoaxial and polyaxial top-loading screws and a 5.5 mm titanium rod in the posterior instrumentation. To achieve hypokyphosis correction intraoperatively prebending of the rod and re-in situ-bending of the concave sided rod after rotation maneuver were steps to improve the operative technique.
The results of this study demonstrate an improvement of the sagittal profile in the posterior group but not the desired physiological kyphosis of the thoracic spine. Therefore, we have modified the posterior technique for improved restoration of kyphosis with two tools. First, we use reduction screws with dual-innie mechanism for segmental derotation. Secondly due to the fact that the flattening of the pre-bended concave titanium rod during the rotation maneuver was identified as further reason for insufficient restoration of thoracic kyphosis we have replaced the concave rod with a more rigid 5.5 mm cobalt chrome rod in hypokyphotic patients.
In both groups, the C7 plumbline value was positive preoperatively and remained so at final follow-up. The positive displacement of the C7 plumbline up to the normal value (+2 cm) observed immediately postoperatively can be explained by postoperative pain. At the last follow-up in nine patients in the anterior group and seven in the posterior group, the C7 plumbline was still more than +2 cm, with no sign of decompensation of thoracic kyphosis or lumbar lordosis.
Anterior thoracic instrumentation led to a significant increase in the PJM from +3.8° preoperatively to +7.4° at final follow-up. An abnormal proximal junctional kyphosis was recorded if the proximal junction Cobb angle was ≥10° and the angle for the corresponding two-level spinal segment was at least 10° greater than the preoperative measurement. Both criteria were required for to establish abnormality, as some proximal junctional kyphoses were lordotic preoperatively [34]. Although a significant increase in the PJM was documented, there were no abnormal PJMs on this basis.
Two cases of fracture of the threaded rod, without relevant loss of correction, were observed. Rod fractures have been reported in the literature in up to 31% of cases, as well as a pseudarthrosis rate of up to 6% [2, 4, 35]. We now routinely use a 4-mm smooth rod to prevent this.
Limitations of this study include its retrospective nature and lack of randomization. Pulmonary function was also not examined. Several studies have reported a postoperative decrease in pulmonary function, which may persist for as long as 2 years [19, 20, 36]. However, any procedure in which the rib cage is opened—e.g., for rib hump resection in posterior instrumentation—can lead to similar negative effects.
Conclusions
Posterior pedicle screw instrumentation and anterior dual rod instrumentation allow restoration of thoracic kyphosis, with comparable coronal plane correction. In patients who have hypokyphotic thoracic curves preoperatively, however, better restoration of thoracic kyphosis can be achieved with anterior instrumentation in contrast to posterior pedicle screw instrumentation.
References
Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F (2005) The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 30:2024–2029. doi:00007632-200509150-00005[pii]
Betz RR, Shufflebarger H (2001) Anterior versus posterior instrumentation for the correction of thoracic idiopathic scoliosis. Spine (Phila Pa 1976) 26:1095–1100
Booth KC, Bridwell KH, Lenke LG, Baldus CR, Blanke KM (1999) Complications and predictive factors for the successful treatment of flatback deformity (fixed sagittal imbalance). Spine (Phila Pa 1976) 24:1712–1720
Betz RR, Harms J, Clements DH 3rd, Lenke LG, Lowe TG, Shufflebarger HL, Jeszenszky D, Beele B (1999) Comparison of anterior and posterior instrumentation for correction of adolescent thoracic idiopathic scoliosis. Spine (Phila Pa 1976) 24:225–239
Kim YJ, Bridwell KH, Lenke LG, Glattes CR, Rhim S, Cheh G (2008) Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up. Spine (Phila Pa 1976) 33:2179–2184. doi:10.1097/BRS.0b013e31817c042800007632-200809150-00009[pii]
Brooks WJ, Krupinski EA, Hawes MC (2009) Reversal of childhood idiopathic scoliosis in an adult, without surgery: a case report and literature review. Scoliosis 4:27. doi:10.1186/1748-7161-4-27
Chun EM, Suh SW, Modi HN, Kang EY, Hong SJ, Song HR (2008) The change in ratio of convex and concave lung volume in adolescent idiopathic scoliosis: a 3D CT scan based cross sectional study of effect of severity of curve on convex and concave lung volumes in 99 cases. Eur Spine J 17:224–229. doi:10.1007/s00586-007-0488-6
Winter RB, Lovell WW, Moe JH (1975) Excessive thoracic lordosis and loss of pulmonary function in patients with idiopathic scoliosis. J Bone Joint Surg Am 57:972–977
Dobbs MB, Lenke LG, Kim YJ, Kamath G, Peelle MW, Bridwell KH (2006) Selective posterior thoracic fusions for adolescent idiopathic scoliosis: comparison of hooks versus pedicle screws. Spine (Phila Pa 1976) 31:2400–2404. doi:10.1097/01.brs.0000240212.31241.8e
Kim YJ, Lenke LG, Cho SK, Bridwell KH, Sides B, Blanke K (2004) Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 29:2040–2048. doi:00007632-200409150-00014[pii]
Suk SI, Lee CK, Min HJ, Cho KH, Oh JH (1994) Comparison of Cotrel-Dubousset pedicle screws and hooks in the treatment of idiopathic scoliosis. Int Orthop 18:341–346
Rhee JM, Bridwell KH, Won DS, Lenke LG, Chotigavanichaya C, Hanson DS (2002) Sagittal plane analysis of adolescent idiopathic scoliosis: the effect of anterior versus posterior instrumentation. Spine (Phila Pa 1976) 27:2350–2356. doi:10.1097/01.BRS.0000030301.48250.3D
Wang J, Zhao Y, Shen B, Wang C, Li M (2010) Risk factor analysis of proximal junctional kyphosis after posterior fusion in patients with idiopathic scoliosis. Injury 41(4):415–420. doi: S0020-1383(10)00003-3[pii]10.1016/j.injury.2010.01.001
Lonner BS, Auerbach JD, Estreicher MB, Kean KE (2009) Thoracic pedicle screw instrumentation: the learning curve and evolution in technique in the treatment of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 34:2158–2164. doi:10.1097/BRS.0b013e3181b4f7e8
Quan GM, Gibson MJ (2010) Correction of main thoracic adolescent idiopathic scoliosis using pedicle screw instrumentation: does higher implant density improve correction? Spine (Phila Pa 1976) 35(5):562–567. doi:10.1097/BRS.0b013e3181b4af34
Li M, Gu S, Ni J, Fang X, Zhu X, Zhang Z (2009) Shoulder balance after surgery in patients with Lenke Type 2 scoliosis corrected with the segmental pedicle screw technique. J Neurosurg Spine 10:214–219. doi:10.3171/2008.11.SPINE08524
Vora V, Crawford A, Babekhir N, Boachie-Adjei O, Lenke L, Peskin M, Charles G, Kim Y (2007) A pedicle screw construct gives an enhanced posterior correction of adolescent idiopathic scoliosis when compared with other constructs: myth or reality. Spine (Phila Pa 1976) 32:1869–1874. doi:10.1097/BRS.0b013e318108b912
Brodner W, Mun Yue W, Moller HB, Hendricks KJ, Burd TA, Gaines RW (2003) Short segment bone-on-bone instrumentation for single curve idiopathic scoliosis. Spine (Phila Pa 1976) 28:S224–S233. doi:10.1097/01.BRS.0000096180.48662.33
Kim YJ, Lenke LG, Bridwell KH, Kim KL, Steger-May K (2005) Pulmonary function in adolescent idiopathic scoliosis relative to the surgical procedure. J Bone Joint Surg Am 87:1534–1541. doi:10.2106/JBJS.C.00978
Lenke LG, Newton PO, Marks MC, Blanke KM, Sides B, Kim YJ, Bridwell KH (2004) Prospective pulmonary function comparison of open versus endoscopic anterior fusion combined with posterior fusion in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 29:2055–2060. doi:00007632-200409150-00016[pii]
Niemeyer T, Schubert C, Halm HF, Herberts T, Leichtle C, Gesicki M (2009) Validity and reliability of an adapted German version of scoliosis research society-22 questionnaire. Spine (Phila Pa 1976) 34:818–821. doi:10.1097/BRS.0b013e31819b33be
Liljenqvist U, Lerner T, Bullmann V (2009) Selective fusion of idiopathic scoliosis with respect to the Lenke classification. Orthopade 38:189–192, 194–187. doi:10.1007/s00132-008-1363-9
Weinstein JN, Spratt KF, Spengler D, Brick C, Reid S (1988) Spinal pedicle fixation: reliability and validity of roentgenogram-based assessment and surgical factors on successful screw placement. Spine (Phila Pa 1976) 13:1012–1018
Cotrel Y, Dubousset J, Guillaumat M (1988) New universal instrumentation in spinal surgery. Clin Orthop Relat Res 227:10–23
Dubousset J, Cotrel Y (1989) CD-instrumentation in the treatment of spinal deformities. Orthopade 18:118–127
Cobb (1948) Outline for the study of scoliosis. In: Edwards JW (ed) Instructional course letters. American Academy of Orthopaedic Surgeons, Ann Arbo
DE Harrison, Harrison DD, Cailliet R, Troyanovich SJ, Janik TJ, Holland B (2000) Cobb method or Harrison posterior tangent method: which to choose for lateral cervical radiographic analysis. Spine (Phila Pa 1976) 25:2072–2078
Bernhardt M, Bridwell KH (1989) Segmental analysis of the sagittal plane alignment of the normal thoracic and lumbar spines and thoracolumbar junction. Spine (Phila Pa 1976) 14:717–721
Sucato DJ, Agrawal S, O’Brien MF, Lowe TG, Richards SB, Lenke L (2008) Restoration of thoracic kyphosis after operative treatment of adolescent idiopathic scoliosis: a multicenter comparison of three surgical approaches. Spine (Phila Pa 1976) 33:2630–2636. doi:10.1097/BRS.0b013e3181880498
Potter BK, Kuklo TR, Lenke LG (2005) Radiographic outcomes of anterior spinal fusion versus posterior spinal fusion with thoracic pedicle screws for treatment of Lenke Type I adolescent idiopathic scoliosis curves. Spine (Phila Pa 1976) 30:1859–1866. doi:00007632-200508150-00011[pii]
Clement JL, Chau E, Kimkpe C, Vallade MJ (2008) Restoration of thoracic kyphosis by posterior instrumentation in adolescent idiopathic scoliosis: comparative radiographic analysis of two methods of reduction. Spine (Phila Pa 1976) 33:1579–1587. doi:10.1097/BRS.0b013e31817886be
Winter RB, Lonstein JE, Denis F (2007) How much correction is enough? Spine (Phila Pa 1976) 32:2641–2643. doi:10.1097/BRS.0b013e31815a5207
Liljenqvist UR, Bullmann V, Schulte TL, Hackenberg L, Halm HF (2006) Anterior dual rod instrumentation in idiopathic thoracic scoliosis. Eur Spine J 15:1118–1127. doi:10.1007/s00586-005-0020-9
Glattes RC, Bridwell KH, Lenke LG, Kim YJ, Rinella A, Edwards C 2nd (2005) Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976) 30:1643–1649. doi: 00007632-200507150-00014[pii]
Sweet FA, Lenke LG, Bridwell KH, Blanke KM, Whorton J (2001) Prospective radiographic and clinical outcomes and complications of single solid rod instrumented anterior spinal fusion in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 26:1956–1965
Kim YJ, Lenke LG, Bridwell KH, Cheh G, Sides B, Whorton J (2008) Prospective pulmonary function comparison of anterior spinal fusion in adolescent idiopathic scoliosis: thoracotomy versus thoracoabdominal approach. Spine (Phila Pa 1976) 33:1055–1060. doi:10.1097/BRS.0b013e31816fc3a5
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schmidt, C., Liljenqvist, U., Lerner, T. et al. Sagittal balance of thoracic lordoscoliosis: anterior dual rod instrumentation versus posterior pedicle screw fixation. Eur Spine J 20, 1118–1126 (2011). https://doi.org/10.1007/s00586-011-1784-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-011-1784-8