Abstract
Purpose
The aim of this study is to understand how many anchor sites are necessary to obtain maximum posterior correction of idiopathic scoliotic curve and if the alloy of instrumentation, stainless steel or titanium, may have a role in the percent of scoliosis correction.
Methods
We reviewed 143 consecutive patients, affected by AIS (Lenke 1–2), who underwent a posterior spinal fusion with pedicle screw-only instrumentation between 2002 and 2005. According to the implant density and alloy used we divided the cohort in four groups.
Results
All 143 patients were reviewed at an average follow-up of 7, 2 years, the overall final main thoracic curve correction averaged 61.4%, whereas the implant density within the major curve averaged 71%. A significant correlation was observed between final% MT correction and preoperative MT flexibility and implant density.
Conclusions
When stainless steel instrumentation is used non-segmental pedicle screw constructs seem to be equally effective as segmental instrumentations in obtaining satisfactory results in patients with main thoracic AIS. When the implant alloy used is titanium one, an implant density of ≥60% should be guaranteed to achieve similar results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since its introduction by Suk [1], the use of thoracic pedicle screw has increasingly become widespread in the treatment of the adolescent idiopathic scoliosis (AIS) and had led to a significant improvement in deformity correction [2–6].
Recently, the relevance of adopting a higher pedicle screw density in scoliosis surgery is object of discussion. Clements et al. [7] introduced the concept of “implant density”, defined as the number of fixation anchors placed for available anchor sites, so it is the % of pedicle used for the implants: they concluded that there was a significant correlation between pedicle screw density and the percentage of curve correction. Quan et al. [8] instead concluded that bilateral segmental pedicle screw fixation do not improve curve correction compared with unilateral and segmental fixation. Similarly, Gebhart et al. [9] found no correlation between increasing pedicle screw density and main thoracic curve correction. However, there is agreement concerning the effect of implant density on sagittal profile: sagittal contour of thoracic spine resulted in a less kyphosis than higher the implant density was [7, 8].
The aim of this study is to understand how the percentage of pedicle screws used for the instrumentation can allow the better correction and its effect on sagittal profile. Another aspect considered in this series is the influence of the instrumentation alloy (titanium vs stainless steel) and its possible correlation with overall correction rate.
Materials and methods
Patient evaluation
A retrospective review, based on a database search, was performed to identify all AIS patients who had undergone posterior spinal fusion with pedicle screw-only instrumentation between 2002 and 2007 at the reference center. The inclusion criteria were: (1) diagnosis of adolescent idiopathic scoliosis; (2) main thoracic or thoracolumbar curve (Lenke type 1, 2); (3) posterior fusion using pedicle screw-only construct; (4) a minimum clinical and radiographic follow-up of 5 years.
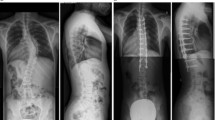
An independent spine surgeon reviewed all the medical records and X-rays of the patients considered. Inpatient and outpatient charts were used for collecting demographic data, peri-operative treatment, and annotation of any medical and surgical-related complications, including revision surgeries. Radiographic evaluation included standing posterior-anterior and lateral films on long-cassettes (90 × 30 cm), before and after surgery and at the latest follow-up. The Lenke classification of AIS was used to describe curve patterns. Cobb measurements of the major thoracic (MT) curves were obtained, and the lateral films were evaluated for thoracic kyphosis (T5–T12). MRI of the spine, including cervical, thoracic and lumbar segments, was performed preoperatively to exclude congenital intramedullary anomalies.
A total of 143 consecutive patients (one single institution, three different surgeons) fulfilled our inclusion criteria, who had undergone a posterior spinal fusion with pedicle screw-only instrumentation. According to the implant density (number of fixation anchors placed per available anchors sites; segmental ≥60%, non-segmental <40%) and implant alloy used (Ti: titanium vs SS: stainless steel) we divided the aforementioned cohort in four groups, titanium segmental (48 patients) and non-segmental (34), stainless steel segmental (35) and non-segmental (26).
Operative procedures
Intraoperative monitoring of spinal cord function was provided in all patients of each group by recording Somatosensory evoked potentials (SEPs) and Transcranial Electric Stimulation-Motor evoked potentials (TES-MEPs). A neurophysiological change was defined relevant when it consisted of a persistent unilateral or bilateral reduction in amplitude ≥50% for SEPs and ≥65% for TES-MEPs compared with baseline.
The same operating table was used in all patients. All cases underwent posterior instrumented fusion after a meticulous exposure of the posterior elements of the spine to the tips of the transverse processes bilaterally. For thoracic screw placement we used the free-hand procedure [10], and sometimes for apical concave screws the spatula technique [11, 12] that allowed for inspection with a spatula inside the canal of the borders of the pedicle, after excision of spinous process and ligamentum flavum. A radical posterior release was performed in every patient at each level to be fused, obtaining a Ponte osteotomy at 3–4 levels for apical vertebrae. In all cases we used monoaxial reduction screws at each level; polyaxial reduction screws were occasionally used in more severe scoliosis in periapical sites to reduce the difficulties of rod capture. Concerning instrumentation, a stainless steel one was used for a group of patients and a titanium one for the others. Arthrodesis was carried out using banked bone (obtained from femoral epiphyses) and autologous chips obtained from resected spinous processes.
Instrumentation consisted of all pedicle screws. The titanium group cases were divided into 48 segmental constructs and 34 non-segmental one; on the other hand the stainless steel group, 61 cases, into 35 segmental construct and 26 non-segmental.
In all cases the deformity correction was carried out using a combination of different corrective techniques, including rod cantilevering, translation and concave rod rotation maneuvers. The operation time averaged a mean of 320 min (range 230–350 min). Mean intraoperative bleeding was 860 ml (range 600–1200 ml, with a mean estimated blood loss of 14.4, and 12.7 cc/kg, respectively). No postoperative brace or a cast was used in any of the patients.
Questionnaires
Six self-reported, patient-based outcome tools, the Italian version of the SRS-30 were obtained by all patients during the last follow-up visit based on the self-image and satisfaction. Statistical analysis was performed using the t test (paired and unpaired), the Wilcoxon test for non-parametric paired analysis, and the Mann–Whitney test for non-parametric unpaired analysis. Results are expressed as the mean (range), with a p value of <0.05 considered as being statistically significant.
Results
The entire series of 143 cases were reviewed at an average follow-up of 7.2 years (range 5–10 years). There were no statistical differences between the four group, in terms of age, Risser’s sign, curve patterns according to Lenke’s classification, Cobb preoperative main thoracic (MT) curve magnitude and flexibility on supine side bending, offset measurements on the coronal plane and sagittal preoperative contour (Table 1).
At follow-up, the overall final main thoracic curve correction averaged 61.4% (20–89), whereas the implant density within the major curve averaged 71% (15–100). A significant correlation was observed between final % MT correction and Preop. Main Thoracic flexibility (r = 0.46, p < 0.001) and implant density (r = 0.41, p < 0.002) (Table 2).
The titanium group (n = 82 patients) was divided into 48 segmental and 34 non-segmental constructs, based on the percentage of pedicle available for the fusion used, if more or less then 60%. The Ti-segmental had a mean age at surgery of 12.1 years (11–16) and a mean Risser’s sign of 1.4 (0–3) (Table 1). The preoperative MT Cobb was of 66° (52–80), which presented on spine bending test a flexibility of 42% (22–56), and achieved a follow-up correction of 68.3% (39–72) (Tables 3, 4).
The Ti-non-segmental group had a mean age at surgery of 13.4 years (12–14), and a mean Risser’s sign of 2.4 (0–4). The preoperative MT Cobb was of 63° (50–75), which presented on spine bending test a flexibility of 40% (15–53), and its follow-up correction was 52% (15–70).
The stainless steel group (n = 61 patients) was divided into the segmental group composed by 35 patients and the non-segmental group with 26 cases; the division was based on the percentage of pedicle available for the fusion used, more or less then 60%. The SS-segmental group had a mean age at surgery of 12.8 years (11–14) and a mean Risser’s sign of 2.5 (0–4). This group showed a mean preoperative Cobb of 69° (59–85), with a flexibility on bending test of 39% (22–49), see in Table 1. The overall correction was 75% (45–100) for the coronal plane (Tables 3, 4).
The SS-non-segmental group had a mean age at surgery of 14.2 years (12–14) and a mean Risser’s sign of 1.8 (0–3). The SS-NS group showed a preoperative Cobb of 62° (53–78), with flexibility on bending test of 41% (23–58) as in Table 1. The final correction was 62.3% (35–71), as in Tables 3 and 4.
In conclusion, when the four distinct groups were compared, the Ti-NS group showed a statistically significant inferior percent MT correction, i.e., 52% with a range from 15 to 70% (Table 3), and no statistically significant differences between SS-S vs Ti-S vs SS-NS was seen (Table 4).
Concerning the coronal balance radiographic measurements, we observed that the thoracic kyphosis, T5–T12 angle (Table 1) was quite similar in each group before surgery, Ti-S was 35.3° (10–41), Ti-NS 30.2° (15–39), SS-S was 32.7° (18–37) and SS-NS was 28.7° (12–35). At follow-up control the absolute final thoracic kyphosis resulted similar (p > 0.05), with groups showing an equally statistical significant amelioration (p < 0.001) of the sagittal contour (Table 5), in titanium group goes to 37.4° ± 17.2° for the segmental group and to 33.4° ± 15.1° for the non-segmental one with a final correction of 42.2 ± 9.3 and 43.4 ± 12.9%, respectively. The stainless steel patients follow-up was 35.4° ± 12.2° for the segmental group and 32.4° ± 15.1° for the non-segmental, with an overall correction of kyphosis of 46.4 ± 12.9 and 47.2 ± 9.3%. At follow-up, no hypo-kyphogenic effect was observed in this cohort of 143 AIS patients. In conclusion, we found a significant correlation between absolute correction of thoracic kyphosis and implant density was observed in all groups (r = 0.39, p < 0.01) (Table 6), while the Ti-NS group showed the inferior correlation (r = 0.36, p < 0.01) between groups.
Questionnaires
Questionnaires scores were available in all patients, at the last follow-up. Preoperative to postoperative comparison of SRS scores could not be performed since the majority of patients. In all, groups had undergone surgery before an Italian version of the SRS-30 questionnaire was available. At the latest follow-up, SRS-30 findings were similar between the four groups, with mean scores shown in Fig. 1.
Discussion
In recent years, there was an increasing use of the “pedicle screw-only construct” in the posterior correction of AIS, dramatically changing how surgeons approach and treat spinal deformities [13]. Several previous reports have demonstrated superiority of pedicle screws in correction of scoliosis in terms of mean absolute degrees and percent of curve correction in comparison to posterior hook and wire or hybrid constructs [5, 6, 14].
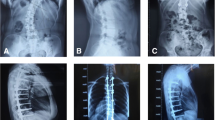
It is still object of discussion if a larger use of screws can allow a better scoliosis correction [7–9, 15, 16]. Recently different pedicle screws strategies have been compared: Wang et al. [16] considered three different pedicle screw strategies (interval, skipped and key-vertebral pedicle screw procedures) obtaining similar results. Similarly, others studies [8, 9, 15] concluded that there were no significant differences in radiographic results or clinical outcomes. On the contrary, in our series, a significant correlation was observed between final % MT correction and preoperative main thoracic flexibility (r = 0.46, p < 0.001) and implant density (r = 0.41, p < 0.002) (Table 2). In agreement with Clements et al. study [7] there was a significant correlation between implant density and % scoliosis correction: using a titanium instrumentation final main thoracic curve correction resulted higher in segmental cases (68.3 vs 52%) (Fig. 2).
The optimal rod stiffness to correct scoliotic curves has yet to be determined. In our series, considering the instrumentation alloy (titanium vs stainless steel) the curve correction resulted higher in stainless steel cases with higher density of screws (75%). When the four distinct groups were compared, the titanium non-segmental group (Ti-NS) showed a statistically significant inferior percent MT curve correction (52%) compared with titanium segmental (68.3%), stainless steel non-segmental (62.3%) (Table 3).
Recently, an improved scoliosis correction has been obtained using rods of cobalt-chromium (CoCr). Lamerain et al. [17] evaluated the results using stainless steel and cobalt-chromium rods materials for treatment of AIS: CoCr rods have the ability to produce higher correction rates in frontal plane compared to SS rods. Moreover, CoCr rods present the advantage of being compatible with magnetic resonance imaging.
Concerning the sagittal profile, after posterior AIS correction using screw-only construct, Clements et al. [7] adds that sagittal contour in the thoracic spine became less kyphotic than the higher the implant density. This is confirmed also by Quan et al. [8], in fact they concluded that pedicle screw constructs provided excellent coronal correction of thoracic idiopathic scoliosis, however, this was at the expense of sagittal contour. In our series, the thoracic kyphosis, T5–T12 angle (Table 1) was quite similar in each group before surgery. At follow-up control the absolute final thoracic kyphosis resulted similar (p > 0.05), with groups showing an equally statistical significant amelioration (p < 0.001) of the sagittal contour (Table 5). Moreover, a significant correlation between absolute correction of thoracic kyphosis and implant density was observed in all groups (r = 0.39, p < 0.01) (Table 6).
Another point of discussion is related to clinical outcomes obtained by different instrumentation constructs. In an era of focus on cost effectiveness in medicine, the increased cost of a higher screw density must be shown to correlate with measurable improvements in outcome [9]. Regardless of the implant density or the alloy used, mid-term self-assessment (by means of SRS-30) was similar in our cases showing a postoperative improvement in both self-image and satisfaction. In our results, SRS-30 findings were similar between the four groups (titanium or stainless steel, segmental or non-segmental) without significant differences between groups: it means that a more expensive construct for scoliosis correction is not always correlated with an increased satisfaction for patients. Similar clinical outcomes after different pedicle screw density are confirmed in recent studies [15, 16].
Conclusions
According to present series results, when stainless steel instrumentation is used non-segmental pedicle screw constructs seem to be equally effective as segmental instrumentations in obtaining satisfactory results in patients with main thoracic AIS. When the implant alloy used is titanium one, an implant density of ≥60% should be guaranteed so as to achieve similar results.
References
Suk SI, Lee CK, Kim WJ, Chung YJ, Park YB (1995) Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine 20(12):1399–1405
Cheng I, Kim Y, Gupta MC, Bridwell KH, Hurford RK, Lee SS, Theerajunyaporn T, Lenke LG (2005) Apical sublaminar wires versus pedicle screws—which provides better results for surgical correction of adolescent idiopathic scoliosis? Spine 30(18):2014–2112
Kim YJ, Lenke LG, Cheh G, Riew KD (2005) Evaluation of pedicle screw placement in the deformed spine using intraoperative plain radiographs: a comparison with computerized tomography. Spine 30(18):2084–2088
Kuklo TR, Potter BK, Polly DW Jr, Lenke LG (2005) Monaxial versus multiaxial thoracic pedicle screws in the correction of adolescent idiopathic scoliosis. Spine 30(18):2113–2120
Di Silvestre M, Bakaloudis G, Lolli F et al (2008) Posterior fusion only for thoracic adolescent idiopathic scoliosis of more than 80 degrees: pedicle screws versus hybrid instrumentation. Euro Spine J 17:1336–1349
Luhmann SJ, Lenke LG, Kim YJ, Bridwell KH, Schootman M (2005) Thoracic adolescent idiopathic scoliosis curves between 70 degrees and 100 degrees: is anterior release necessary? Spine 30(18):2061–2067
Clements DH, Betz RR, Newton PO, Rohmiller M, Marks MC, Bastrom T (2009) Correlation of scoliosis curve correction with the number and type of fixation anchors. Spine. 34(20):2147–2150
Quan GM, Gibson MJ (2010) Correction of main thoracic adolescent idiopathic scoliosis using pedicle screw instrumentation: does higher implant density improve correction? Spine 35(5):562–567
Gebhart S, Alton T, Bompadre V et al (2014) Do anchor density or pedicle screw density correlate with short-term outcome measures in adolescent idiopathic scoliosis surgery? Spine 39(2):pE104–pE110
Kim YJ, Lenke LG, Bridwell KH, Cho YS, Riew KD (2004) Free hand pedicle screw placement in the thoracic spine: is it safe? Spine. 29(3):333–342
Kabins MB (2004) Point of view. Spine 29:342. doi:10.1097/01.BRS.0000109984.65138.0C
Di Silvestre M, Parisini P, Lolli F, Bakaloudis G (2007) Complications of thoracic pedicle screws in scoliosis treatment. Spine 32(15):1655–1661
Mc Cormick J, Aebi M, Toby D, Arlet V (2013) Pedicle screw instrumentation and spinal deformities: have we gone too far? Eur Spine J 22(Suppl 2):S216–S224
Crostelli M, Mazza O, Mariani M, Mascello M (2013) Treatment of severe scoliosis with posterior-only approach arthrodesis and all-pedicle screw instrumentation. Eur Spine J 22(Suppl 6):S0808–S0814
Morr S, Carrer A, Alvarez-Garcia de Quesada LI, Rodriguez-Olaverri JC (2015) Skipped versus consecutive pedicle screw constructs for correction of Lenke 1 curves. Eur Spine J 24(7):1473–1480
Wang F, Xu XM, Lu Y, Wei XZ, Zhu XD, Li M (2016) Comparative analysis of interval, skipped, and key-vertebral pedicle screw strategies for correction in patients with Lenke type 1 adolescent idiopathic scoliosis. Medicine (Baltimore) 95(10):e3021
Lamerain M, Bachy M, Delpont M, Kabbaj R, Mary P, Vialle R (2014) CoCr rods provide better frontal correction of adolescent idiopathic scoliosis treated by all-pedicle screw fixation. Eur Spine J 23(6):1190–1196
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors disclose any financial and personal relationships with other people or organization that could inappropiately influence their work.
Funding
No funds were received in support of this study.
Rights and permissions
About this article
Cite this article
Di Silvestre, M., Bakaloudis, G., Ruosi, C. et al. Segmental vs non-segmental thoracic pedicle screws constructs in adolescent idiopathic scoliosis: is there any implant alloy effect?. Eur Spine J 26 (Suppl 4), 533–538 (2017). https://doi.org/10.1007/s00586-017-5046-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5046-2