Abstract
A variety of bone graft substitutes, interbody cages, and anterior plates have been used in cervical interbody fusion, but no controlled study was conducted on the clinical performance of β-tricalcium phosphate (β-TCP) and the effect of supplemented anterior plate fixation. The objective of this prospective, randomized clinical study was to evaluate the effectiveness of implanting interbody fusion cage containing β-TCP for the treatment of cervical radiculopathy and/or myelopathy, and the fusion rates and outcomes in patients with or without randomly assigned plate fixation. Sixty-two patients with cervical radiculopathy and/or myelopathy due to soft disc herniation or spondylosis were treated with one- or two-level discectomy and fusion with interbody cages containing β-TCP. They were randomly assigned to receive supplemented anterior plate (n = 33) or not (n = 29). The patients were followed up for 2 years postoperatively. The radiological and clinical outcomes were assessed during a 2-year follow-up. The results showed that the fusion rate (75.0%) 3 months after surgery in patients treated without anterior cervical plating was significantly lower than that (97.9%) with plate fixation (P < 0.05), but successful bone fusion was achieved in all patients of both groups at 6-month follow-up assessment. Patients treated without anterior plate fixation had 11 of 52 (19.2%) cage subsidence at last follow-up. No difference (P > 0.05) was found regarding improvement in spinal curvature as well as neck and arm pain, and recovery rate of JOA score at all time intervals between the two groups. Based on the findings of this study, interbody fusion cage containing β-TCP following one- or two-level discectomy proved to be an effective treatment for cervical spondylotic radiculopathy and/or myelopathy. Supplemented anterior plate fixation can promote interbody fusion and prevent cage subsidence but do not improve the 2-year outcome when compared with those treated without anterior plate fixation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cervical discectomy and fusion is considered to be the gold standard for the treatment of symptomatic degenerative disc disease. Different interbody fusion techniques have been proposed in order to restore the physiological height of the intervertebral space and lordosis of the cervical spine after removal of the offending disc and osteophytes [8, 21]. The autograft is the most commonly used fusion material [4, 18].
Interbody fusion cages have been developed to avoid the complications related to bone harvesting from the donor site while increasing immediate stability of the cervical spine after decompression and promoting bony fusion [3, 12, 17] Some authors [1, 6] recommended the use of anterior cervical fusion with cage containing bone substitutes. Satisfactory results were obtained regarding the fusion rates although fusion was delayed as compared with that in a cage containing autograft [6].
The present study was undertaken to evaluate prospectively the effectiveness of implanting interbody fusion cages containing β-tricalcium phosphate (β-TCP) for the treatment of cervical radiculopathy and/or myelopathy. Another purpose of this study was to evaluate the fusion rates and outcomes in patients with or without randomly assigned plate fixation.
Materials and methods
Patient population
This prospective study was approved by the Institutional Review Board of our institution. Between January 2001 and December 2004, a consecutive series of 62 patients participated in the study. These patients with progressive upper extremity radicular symptoms and/or myelopathy resulting from cervical degenerative disc disease underwent one- to two-level discectomy at contiguous levels from C3–4 to C6–7 for soft disc herniation or spondylosis. The exclusion criteria were that the patient had more than two level developmental stenosis of the cervical spine, continuous or combined ossification of the posterior longitudinal ligament, prior cervical spine surgery, and significant comorbidities associated with poor general health.
There were 40 men and 22 women, with an average age of 45.3 years (range 29–65 years). In all patients, the diagnostic work-up included clinical examination, conventional and lateral flexion/extension plain radiography of the cervical spine, and magnetic resonance imaging (MRI). All these patients had disease duration of at least 1 month, with the similar average in both groups (11.4 ± 8.2 months vs. 10.7 ± 10.0 months). After informed consent was obtained, the patients were randomized to receive interbody fusion cage augmented with or without anterior plate fixation. Patient characteristics are summarized in Table 1.
Surgical technique
General inhalation anesthesia was used in all patients. All operations were performed by either of the two authors. After a standard right-sided anterior approach to the cervical spine was performed as described by Smith and Robinson, the disc space was opened and distraction was applied using a Caspar distractor. A discectomy was performed with or without posterior osteophytectomy as needed but the subchondral bone was preserved carefully. The posterior longitudinal ligament was opened and the neural structure decompressed with the dura, and the origin of the nerve roots visualized in all cases.
Instrumentation
The interbody fusion was performed with carbon fiber (43 levels in 27 patients) or PEEK (56 levels in 35 patients) cages containing granulated β-TCP under fluoroscopy. After the cage was implanted, anterior plate fixation was either added or not as randomly assigned before surgery. The correct position was checked by anteroposterior and lateral views of plain radiography before wound closure. After the surgery, all patients were immobilized with a rigid cervical collar for 4–6 weeks.
Outcome measurements
Radiographic evaluation
An independent observer evaluated the preoperative and postoperative radiographs including standard and flexion–extension views before, immediately, and 3, 6, 12, and 24 months after surgery. Subsidence or immigration as defined by Gercek et al. [11] was assessed on the lateral radiographs. Fine-cut computed tomography scan was done 3 months after surgery and then at the 3-month interval months until fusion was complete, with the fusion defined as the presence of continuous trabeculae within the cage in combination with the disappearance of the bone borders around the cages and motion upon the cage and/or plate on flexion–extension radiographs. The overall and segmental lordosis or kyphosis at the surgical level was measured with Cobb method on the lateral radiographs.
Clinical evaluation
The neurological outcomes, both preoperatively and at discharge, 3, 6, 12, and 24 months after surgery, in both groups were measured according to their Japanese Orthopedic Association (JOA) score [13] (Table 2). The recovery rate of JOA score was calculated according to the formula: recovery rate (%) = postoperative score − preoperative score/17 − preoperative score × 100. A 10-point visual analogue scale (VAS) with endpoint anchors of “no pain (0)” and “worst possible pain (10)” was used to rate the neck or arm pain before surgery and at each follow-up visit.
Statistical analysis
The unpaired Student’s t test or Chi-square test was used for comparison of the results between the two groups, and paired t test or repeated measures ANOVA followed by Newman–Keuls–Student test for comparison of the results between time points. Significance was set at the level of P < 0.05.
Results
The average operative time was 49 min (range 40–67 min) for one-level and 93 min (range 85–100 min) for two-level procedures. Patients treated with anterior cervical plating had longer operative time than those without plate fixation (77 ± 16 vs. 54 ± 18 min, P < 0.05), but no statistical significance (P > 0.05) with respect to blood loss or hospital stay was noted between the two groups. All patients were followed up for 2 years. There were no early or late implant-related complications, and no additional surgeries were required for any cause in both groups.
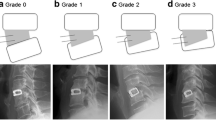
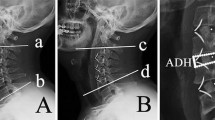
The fusion rate 3 months after surgery was 98.1% (51/52) for the 33 patients treated with anterior cervical plating (Figs. 1 and 2) and 72.3% (34/47) for the 29 patients treated without plate fixation, respectively. The difference was statistically significant (χ2 = 13.467, P < 0.05). Thereafter, successful bone fusion was achieved in all patients of both groups at 6-month follow-up assessment. Superior and/or inferior cage immigration into the endplates was demonstrated on the radiographs of 10 of 47 levels (21.2%) in 33 patients treated without anterior plating at last follow-up, but there was no case of cage immigration in any patients who received plate fixation (χ2 = 12.307, P < 0.05). Neither anterior nor posterior immigration of the cage was noted in any patients of both the groups.
The average overall and segmental lordosis before surgery was 11.7 ± 7.8° (range −8.4 to 20.5°) and 0.8 ± 2.7° (range −5.0 to 3.1°) in patients with plate fixation, and 12.4 ± 8.2° (range −7.6 to 16.3°) and 1.0 ± 3.2° (range −5.2 to 4.3°) in patients without plating, respectively. At the final follow-up, the lordosis angle was significantly (P < 0.05) improved to 15.0 ± 4.7° (range −2.5 to 21.0°) and 3.2 ± 4.6° (range −1.8 to 4.2°) in patients with plate fixation, and 14.3 ± 8.2° (range −7.6 to 16.3°) and 3.8 ± 4.8° (range −1.5 to 4.8°) in patients without plating, respectively. There were no significant differences (P > 0.05) between groups. The kyphotic deformity was corrected in 17 of 20 patients (Table 3), and no iatrogenic cervical deformity was noted in any patient at the final follow-up examination.
The preoperative average JOA score was 8.1 ± 2.7 (range 7–12) points in patients with plate fixation, and 7.8 ± 2.4 (range 6–12) points in patients without plating, respectively. At final follow-up, the average JOA score improved to 14.3 ± 2.7 (range 11–17) points in patients with plate fixation and 13.8 ± 1.9 (range 9–16) points in patients without plating (Fig. 3). The average recovery rate was 70.1% in patients with plate fixation and 72.4% in patients without plating (Fig. 4). There were no significant differences (P > 0.05) when comparing the JOA scores and recovery rate between groups at all time intervals and between one-level and two-level fusion. In the two groups, the average postoperative neck or arm pain as measured by VAS showed significant relief (P < 0.05) when compared with the preoperative score (Figs. 5 and 6), but no significant difference of the VAS was observed between the two groups (P > 0.05).
Time course of JOA score preoperatively, at discharge, and at 3, 6, 12, and 24 months after interbody fusion cage containing β-TCP supplemented with or without anterior plate fixation. Values are presented as the means ± SDs. The difference between the preoperative and postoperative values was significant (P < 0.05) at all follow-up time points. There was no significant difference (P > 0.05) between both groups at all time points
Time course of the recovery rate of JOA score preoperatively, at discharge, and at 3, 6, 12, and 24 months after interbody fusion cage containing β-TCP supplemented with or without anterior plate fixation. Values are presented as the means ± SDs. The difference between the preoperative and postoperative values was significant (P < 0.05) at all follow-up time points. There was no significant difference (P > 0.05) between both groups at all time points
Time course of neck pain as assessed with VAS preoperatively, at discharge, and at 3, 6, 12, and 24 months after interbody fusion cage containing β-TCP supplemented with or without anterior plate fixation. Values are presented as the means ± SDs. The difference between the preoperative and postoperative values was significant (P < 0.05) at all follow-up time points. There was no significant difference (P > 0.05) between both groups at all time points
Time course of arm pain as assessed with VAS preoperatively, at discharge, and at 3, 6, 12, and 24 months after interbody fusion cage containing β-TCP supplemented with or without anterior plate fixation. Values are presented as the means ± SDs. The difference between the preoperative and postoperative values was significant (P < 0.05) at all follow-up time points. There was no significant difference (P > 0.05) between both groups at all time points
Discussion
Subsidence and/or immigration of stand-alone cervical interbody fusion cage have been reported in the literature [2, 11, 19] although the cortical endplates are preserved with great care. Payer et al. [19] noted secondary loss of intervertebral height (≥2 mm) due to cage subsidence in 4 of 20 (20%) patients who received anterior fusion with a cervical interbody cage, whereas Bartel et al. [2] found that nearly 30% of the cages experienced a subsidence into the vertebral body at 6 weeks postoperatively. However, no association was noted between cage subsidence and fusion rate or clinical outcome in the two series. Gercek et al. [11] identified five cage subsidence in nine patients who received cage implantation for cervical fusion, and one of them broke during the follow-up period and led to subsequent foraminal stenosis and recurrent radiculopathy.
Cage subsidence has been regarded as a result of instability created by the discectomy and the postoperative cervical motion. Wilke et al. [14, 27] investigated the effect of simulated postoperative neck movements on cage subsidence by using a cyclic testing protocol, and found that cyclic loading would lead to cage subsidence into the adjacent vertebrae and that the relation between flexibility increase and subsidence would depend upon the implant design. Shimamoto et al. [25], in an in vitro biomechanical study, evaluated the immediate stability afforded by stand-alone interbody fusion cage in the cervical spine and concluded that the cervical interbody fusion cage should be supplemented with the addition of external or internal supports. However, the role of external support remains questionable [12, 15]. Addition of anterior plate fixation at the level with interbody cage has been recommended to promote successful fusion [7, 22].
In the present study, we prospectively compared the clinical and radiological outcomes of anterior cervical fusion with interbody cage containing β-TCP following one- to two-level discectomy in the treatment of patients with radiculopathy, myelopathy, or a combination of both due to soft disc herniation or spondylosis. All patients included in this study were randomly assigned to either receive anterior plate fixation or not. The results showed that the fusion rate 3 months after surgery was significantly higher in patients treated with anterior cervical plating than those treated without plate fixation, thus suggesting supplemented anterior plate fixation would promote interbody fusion in one- and two-level anterior cervical discectomy and fusion with interbody cages containing β-TCP by providing more stability immediately after surgery. The difference of fusion rate between the two groups was observed only at 3-month follow-up after surgery. However, at 6-month follow-up assessment, all patients of both groups achieved interbody fusion.
Whether the delay in interbody fusion for the cases without anterior plate fixation was related to clinical and radiological outcome was also evaluated in this study. As the results show, we did not identify any difference of improvement in spinal curvature or neck and arm pain, or recovery rate of JOA score between the two groups. These findings indicate that supplemented anterior plate fixation might be not necessary in one- and two-level anterior cervical discectomy and fusion with interbody cage containing β-TCP despite cage subsidence and delayed interbody fusion. Also, use of interbody cage without supplemented anterior plate fixation would be cost-effective.
Bone substitutes, such as calcium phosphate ceramics, have been used as alternatives to autogenous bone graft in spinal fusion surgery. The possibility of using these biomaterials in cervical interbody fusion has been investigated in animal models and in clinical practice [9, 20, 26], but there is a lack of literature regarding the use of β-TCP for cervical interbody fusion. Being more degradable and bioresorbable in vivo than hydroxyapatite, β-TCP might be replaced faster by the new bone but weak in mechanical strength when load-bearing capacity is regarded. Xie et al. [28] reported a failed case of anterior cervical interbody fusion with a stand-alone dense β-TCP block and suggested special design for the bioceramic to assure bone ingrowth and meet the mechanical requirements in cervical interbody fusion. In the current series, interbody cages were used to contain granulated β-TCP. The advantage would be that they could provide immediate stability and share the load on bone substitutes to prevent collapse. The results were comparable with those reported by some authors [1, 6, 16] who used other calcium phosphate ceramics. Additionally, the ample blood supply might be another reason for successful interbody fusion.
The current study had limitations: no comparison was made with autograft that was regarded as the gold standard for interbody fusion. However, another study of ours [10] has shown that use of β-TCP combined with local autograft for spine fusion would result in the same radiographic fusion rates and similar improvement of clinical outcomes and life quality compared with autograft alone. Successful bone fusion was achieved in all patients of this series. The satisfactory results also suggested that the use of bone substitutes would eliminate bone grafting harvesting and the related complications. Another limitation of this study might be that two different fusion cages were used, but no impact of cage design and material was observed on the occurrence and degree of cage subsidence.
Assessment of interbody fusion remains a challenging problem. As the criteria to determine radiological fusion is not well defined and universally accepted, it is often difficult to arrive at a true assessment of fusion based on plain radiography particularly when interbody fusion cages are used. Fine-cut CT scans with reconstructions have been shown to be more reliable and sensitive for the detection of pseudarthrosis than plain radiography [5, 23, 24]. In the current study, the fusion status was assessed using fine-cut CT scans with reconstructions in addition to static and flexion–extension radiography. According to the results of this study, we suggest CT scans for the evaluation of fusion status when interbody fusion cages are used.
Conclusion
In summary, interbody fusion cage containing β-TCP following one- or two-level discectomy proved to be an effective treatment for cervical spondylotic radiculopathy and/or myelopathy. Supplemented anterior plate fixation can increase the fusion rate and prevent cage subsidence but did not improve the 2-year outcome when compared with those treated without anterior plate fixation.
References
Agrillo U, Mastronardi L, Puzzilli F (2002) Anterior cervical fusion with carbon fiber cage containing coralline hydroxyapatite: preliminary observations in 45 consecutive cases of soft-disc herniation. J Neurosurg 96(3 Suppl):273–276
Bartels RH, Donk RD, Feuth T (2006) Subsidence of stand-alone cervical carbon fiber cages. Neurosurgery 58:502–508
Bartels RH, Donk R, van Azn RD (2001) Height of cervical foramina after anterior discectomy and implantation of a carbon fiber cage. J Neurosurg 95(1 Suppl):40–42
Bishop RC, Moore KA, Hadley MN (1996) Anterior cervical interbody fusion using autogenic and allogenic bone graft substrate: a prospective comparative analysis. J Neurosurg 85:206–210
Carreon LY, Glassman SD, Djurasovic M (2007) Reliability and agreement between fine-cut CT scans and plain radiography in the evaluation of posterolateral fusions. Spine J 7:39–43
Cho DY, Lee WY, Sheu PC, Chen CC (2005) Cage containing a biphasic calcium phosphate ceramic (Triosite) for the treatment of cervical spondylosis. Surg Neurol 63:497–504
Christodoulou A, Ploumis A, Terzidis I, Hantzidis P, Tapsis K, Pournaras J (2004) Combined interbody cage and anterior plating in the surgical treatment of cervical disc disease. Acta Orthop Belg 70:461–465
Cloward RB (1958) The anterior approach for ruptured cervical discs. J Neurosurg 15:602–614
Cook SD, Dalton JE, Tan EH, Tejeiro WV, Young MJ, Whitecloud TS III (1994) In vivo evaluation of anterior cervical fusions with hydroxylapatite graft material. Spine 19:1856–1866
Dai LY, Jiang LS (2008) Single-level instrumented posterolateral fusion of lumbar spine with β-tricalcium phosphate versus autograft: a prospective, randomized study with 3-year follow-up. Spine (in press)
Gercek E, Arlet V, Delisle J, Marchesi D (2003) Subsidence of stand-alone cervical cages in anterior interbody fusion: warning. Eur Spine J 12:513–516
Hacker RJ, Cauthen JC, Gilbert TJ, Griffith SL (2000) A prospective randomized multicenter clinical evaluation of an anterior cervical fusion cage. Spine 25:2646–2655
Japanese Orthopaedic Association (1994) Scoring system for cervical myelopathy. J Jpn Orthop Assoc 68:490–503
Kettler A, Wilke HJ, Claes L (2001) Effects of neck movements on stability and subsidence in cervical interbody fusion: an in vitro study. J Neurosurg 94(1 Suppl):97–107
Lind BI, Zoega B, Rosen H (2007) Autograft versus interbody fusion cage without plate fixation in the cervical spine: a randomized clinical study using radiostereometry. Eur Spine J 16: 1251–1256
Mastronardi L, Ducati A, Ferrante L (2006) Anterior cervical fusion with polyetheretherketone (PEEK) cages in the treatment of degenerative disc disease: preliminary observations in 36 consecutive cases with a minimum 12-month follow-up. Acta Neurochir 148:307–312
Matge G (1998) Anterior interbody fusion with the BAK-cage in cervical spondylosis. Acta Neurochir 140:1–8
McConnell JR, Freeman BJ, Debnath UK, Grevitt MP, Prince HG, Webb JK (2003) A prospective randomized comparison of coralline hydroxyapatite with autograft in cervical interbody fusion. Spine 28:317–323
Payer M, May D, Reverdin A, Tessitore E (2003) Implantation of an empty carbon fiber composite frame cage after single-level anterior cervical discectomy in the treatment of cervical disc herniation: preliminary results. J Neurosurg 98(2 Suppl):143–148
Pintar FA, Maiman DJ, Hollowell JP, Yoganandan N, Droese KW, Reinartz JM, Cuddy B (1994) Fusion rate and biomechanical stiffness of hydroxylapatite versus autogenous bone grafts for anterior discectomy: an in vivo animal study. Spine 19:2524–2528
Robinson RA, Smith GW (1955) Anterolateral cervical disc removal and interbody fusion for cervical disc syndrome. Bull Johns Hopkins Hosp 96:223–224
Samandouras G, Shafafy M, Hamlyn PJ (2001) A new anterior cervical instrumentation system combining an intradiscal cage with an integrated plate: an early technical report. Spine 26:1188–1192
Santos ER, Goss DG, Morcom RK, Fraser RD (2003) Radiologic assessment of interbody fusion using carbon fiber cages. Spine 28:997–1001
Shah RR, Mohammed S, Saifuddin A, Taylor BA (2003) Comparison of plain radiographs with CT scan to evaluate interbody fusion following the use of titanium interbody cages and transpedicular instrumentation. Eur Spine J 12:378–385
Shimamoto N, Cunningham BW, Dmitriev AE, Minami A, McAfee PC (2001) Biomechanical evaluation of stand-alone interbody fusion cages in the cervical spine. Spine 26:E432–E436
Suetsuna F, Yokoyama T, Kenuka E, Harata S (2001) Anterior cervical fusion using porous hydroxyapatite ceramics for cervical disc herniation: a two-year follow-up. Spine J 1:348–357
Wilke HJ, Kettler A, Goetz C, Claes L (2000) Subsidence resulting from simulated postoperative neck movements. Spine 25:2762–2770
Xie Y, Chopin D, Hardouin P, Lu J (2006) Clinical, radiological and histological study of the failure of cervical interbody fusions with bone substitutes. Eur Spine J 15:1196–1203
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was supported by Shanghai Natural Science Foundation (No. 044119626).
Rights and permissions
About this article
Cite this article
Dai, LY., Jiang, LS. Anterior cervical fusion with interbody cage containing β-tricalcium phosphate augmented with plate fixation: a prospective randomized study with 2-year follow-up. Eur Spine J 17, 698–705 (2008). https://doi.org/10.1007/s00586-008-0643-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-008-0643-8