Abstract
Purpose
To evaluate the clinical efficacy and radiological outcomes of anterior cervical discectomy and fusion (ACDF) using self-locking polyetheretherketone (PEEK) cages for treatment of three-level cervical degenerative spondylopathy.
Methods
Twenty-eight patients underwent three-level ACDF using self-locking stand-alone PEEK cages (group A), and 26 patients underwent three-level ACDF using cages and plate fixation (group B) were reviewed retrospectively. Clinical efficacy was evaluated by pre- and post-operative Japanese Orthopedic Association (JOA) scores and Neck Disability Index (NDI). The operation time, blood loss, surgical results according to Odom’s criteria and post-operative dysphagia status were also recorded. Radiological outcomes including fusion, cervical Cobb’s lordosis, fused segment angle, disc height, and cage subsidence were assessed.
Results
Clinical outcome measures such as dysphagia and fusion rate and the results of surgery evaluated according to Odom’s criteria were not statistically significant (P > 0.05) between groups. The operation time was shorter and blood loss was less in group A (P < 0.05). The NDI and JOA scores showed significant improvements in both groups after surgery at each time point (P < 0.05) with no significant difference between groups (P > 0.05). Post-operative cage subsidence, the loss of disc height, cervical lordosis and the fused segment angle were relatively higher in group A than group B (P < 0.05).
Conclusions
ACDF using self-locking stand-alone cages showed similar clinical results as compared to ACDF using cages and plate fixation for the treatment of three-level cervical degenerative spondylopathy. However, potential long-term problems such as cage subsidence, loss of cervical lordosis and fused segment angle post-operatively were shown to be associated with patients who underwent ACDF using self-locking stand-alone cages.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The surgical procedure for multilevel cervical spondylopathy aims to decompress the spinal cord or spinal nerves so as to relieve the symptoms of neck stiffness and pain, motor and sensory dysfunction, or gait disorders. Anterior cervical decompression and fusion (ACDF) has been practiced for over 50 years since it was first described by Smith and Robinson [1]. With anterior plate fixation, immediate stability of cervical spine can be achieved and the risk of pseudarthrosis reduced considerably [2, 3]. Studies have demonstrated safety and efficacy of three-level ACDF with cages and plate fixation [3, 4]. However, complications associated with plate fixation such as breakage, loosening of screws, screw penetration to endplate, triangle fracture, trachea-esophageal or neurovascular structural injuries have been reported, especially in multilevel ACDF [2, 5].
To overcome these limitations of anterior plating, stand-alone cages have been developed. However, there is disagreement regarding the use of stand-alone cages with respect to subsidence, cage migration, loss of cervical lordosis and fused segment angle, and relatively low fusion rate [6]. Recently, a new type of stand-alone polyetheretherketone (PEEK) cage has been designed with self-locking anchoring clips impacted through the cage into the vertebral bodies of the adjacent segments. The function of anchoring clips is considered to be similar to a plate and screws, offering immediate stabilization after surgery [7]. Studies have also shown that this kind of cages can effectively restore cervical lordosis, and obviate the plate-related complications, as compared to ACDF using cages and plate fixation for single or double-level cervical spondylopathy [7–9]. Further, a non-comparative study has reported satisfactory clinical efficacy and radiological outcomes with the three-level ACDF using this kind of PEEK cages [10]. The objective of this study was to evaluate the clinical and radiological outcomes of ACDF using self-locking stand-alone PEEK cages for treatment of three-level cervical spondylopathy compared with ACDF using cages with plate fixation.
Materials and methods
Patient population and indications
Between January 2012 and January 2013, a total of 54 patients, aged 38–64 years, who received three-level ACDF from the Department of Spinal Surgery of The Second Xiangya Hospital, Central South University, China, took part in the study. The inclusion criteria were: (1) signs and symptoms of cervical radiculopathy or cervical spondylotic myelopathy not responsive to conservative treatment, (2) age between 18 and 65, (3) disc herniation confirmed by computed tomography (CT) or magnetic resonance imaging with nerve root or spinal cord compression, (4) three contiguous disc levels between C3 and C7 involved. The exclusion criteria were: (1) continuous or combined ossification of the posterior longitudinal ligament (OPLL), (2) developmental stenosis, (3) pre-operative dysphagia (4) severe cervical malformation, (5) active rheumatoid arthritis, (6) history of invasive malignancy, (7) known allergy to the constituent materials used in the device, (8) history of cervical spine trauma and/or cervical spine surgery, (9) evidence of systemic or local infection. Informed consent was obtained from all individual participants included in the study. Patients included were divided into two groups: Group A comprising 28 patients (18 male, 10 female) with age 54.1 ± 8.8 years (range 41–64) underwent ACDF using self-locking stand-alone PEEK cage; and Group B comprising 26 patients (15 male, 11 female) with age 54.7 ± 12.1 years (range 38–63) underwent ACDF using cage and plate fixation. The mean follow-up time in group A was 28.8 ± 9.7 months and in group B was 29.6 ± 8.3 months. None of the patients were lost to follow-up. There was no significant difference in any of the demographic variables between the two groups (Table 1).
Surgical procedure
All the surgical procedures were performed by the same senior surgeon (Lü) using standard Smith-Robinson approach [1]. The cartilaginous disc endplate was carefully removed and care was taken to avoid excessive damage to bony endplate. The posterior osteophytes were removed by curettes and Kerrison rongeurs. After complete decompression of the spine cord and nerve roots, the ideal sizes of cages were selected by radiographic assisted trials. The width of the cage was determined by the distance between the two Luschka’s joints, and the height of the cage was determined by different trails under radiography, when trails are tightly fitted in the disc space without over-distraction of the disc space or facet joints. Porous bioceramic artificial bone (Dragonbio®, Hubei, China) was used to fill in the cage in all patients.
In group A, proper sized devices (ROI-C® or ROI-MC+®, LDR, France) were inserted and the anchorage systems were inserted in the vertebral bodies under the fluoroscopic guidance.
In group B, cages (Cervios™, Synthes Inc., Raynham, MA, USA) were inserted under the guidance of fluoroscopy along with anterior cervical plate (CSLP™, Synthes Inc., Raynham, MA, USA).
Outcome assessment
Clinical outcomes
The operation time and blood loss during surgeries were recorded. The neck disability index (NDI), Japanese orthopedic association (JOA) were measured pre-operatively, and post-operative recordings were taken at 2 weeks, and 3, 6, 12 and 24 months. The patient’s dysphagia status was recorded pre-operatively, and post-operatively after 48 h, 2 weeks, 3, 6, 12 and 24 months and were rated as: none (no episodes of swallowing problems), mild (rare episodes of dysphagia), moderate (occasional swallowing difficulty with specific food), or severe (frequent swallowing difficulty with majority of food) [11]. The result of the surgeries, which were graded by Odom’s criteria [12] listed in Table 2, were evaluated by two independent researchers. Discordant opinion was resolved by discussion with another independent expert (Kuang) and reaching a consensus.
Radiological outcomes
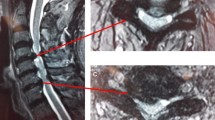
Nonunion means the presence of more than 2° range of motion on flexion–extension lateral radiographs or the presence of a radiolucent gap between the graft and the end plate on radiographs or CT scans in at least one operated level at the last follow-up [10]. The other radiological outcomes were measured pre-operatively and at 2 weeks, 3, 6, 12 and 24 months post-operatively. Cervical lordosis was defined as the angle formed by the inferior end plate of C2 and C7 in neutral position on a plain lateral film (Fig. 1a) [13]. Fused segment angle was defined as the angle formed by the upper endplate of the superior vertebrae body and the lower endplate of the inferior vertebrae body, in neutral position (Fig. 1b). The disc height was defined as the mean value of the anterior disc height (ADH) and the posterior disc height (PDH) (Fig. 1c). The loss of disc height (cervical lordosis or fused segment angle) was defined as the decrease of the disc height at 24 months post-operation compared with the measurement taken 2 weeks after surgery. Subsidence was defined as the loss of the disc height more than 3 mm at each time point compared to the measurement taken 2 weeks after surgery [6]. Two independent researchers assessed the radiographs (Li and Wang). Discordant opinion about the fusion healing was resolved by discussion with another independent expert (Kuang) and reaching a consensus.
a The measurement method for cervical Cobb’s lordosis: the angle formed by the upper end plate of C2 and lower end plate of C7 in neutral position (line a and line b); b the measurement method of the fused segment angle: the angle formed by the upper endplate of the superior vertebrae body and the lower endplate of the inferior vertebrae body in neutral position (line c and line d); c the measurement method for disc height: the mean value of the anterior disc height and the posterior disc height
Statistical analysis
All statistical analyses were conducted using SPSS version 19.0 software (SPSS Inc., Chicago, IL, USA). Clinical and radiological outcomes between groups were analyzed using Student t test. The comparisons of pre- and post-operative parameters within group were performed using a paired-t test. Chi square test was used for analyzing the categorical variables, such as the incidence of dysphagia and the rate of subsidence. A non-parametric test (Kruskal–Wallis H test) was used to analyze the results of surgery according to Odom’s criteria. A P value of less than 0.05 was considered statistically significant. Kappa value was calculated to evaluate the inter-observer discrepancy when judging the fusion rate and the results of surgery according to Odom’s criteria, with a higher value indicating better reliability. A Kappa value less than 0.75 is considered as poor reliability, and 0.75–1 as good reliability.
Results
Clinical outcome assessments
Seventeen patients underwent C3–C6 fusion and 11 C4–C7 fusion using self-locking cages in group A, While 14 patients underwent C3–C6 fusions and 12 C4–C7 fusions using anterior plate in group B with no significant different between groups. No instances of perioperative cerebral fluid leakage, wound infection, hematoma, cage migration or plate-related complications were reported in either group. The operative time was shorter and the blood loss was less in the Group A (113.7 ± 31.5 min, 159.9 ± 38.1 ml) compared with Group B (138.2 ± 39.1 min, 187.4 ± 42.8 ml) (P < 0.05, P < 0.05) (Table 1). Sixteen patients in group A and 18 in group B complained of mild dysphagia 24 h post-surgery. Of these, nine patients in group A and eight in group B recovered at 2 weeks post-operatively with an aerosol inhalation mixture of 5 mg chymotrypsin three times daily, the other five in group A and three in group B recovered spontaneously at 3 months post-operatively. Only one patient in groups B experienced mild dysphagia at the last follow-up. The difference between groups in dysphagia rate was not significant at each time point. The difference in surgical results between group A and B did not reach statistical significance as per Odom’s criteria (Kappa value = 0.863) (Table 2). Both groups demonstrated significant improvements in the NDI and JOA scores after surgery but without significant difference at each time point (Fig. 2).
Radiological outcome assessments
Thirteen patients in group A and 11 in group B did not undergo CT scans during follow-up due to patient refusal or financial constraints. Four patients in group A and two in group B suffered at least one segment nonunion assessed through radiographs obtained at the last follow-up (P = 0.736, Kappa value = 0.813). The post-operative cervical lordosis, fused segment angle, and disc height in both groups differed from their respective pre-operative values at each time point (Fig. 3). Concerning Cervical Cobb’s lordosis, the pre-operative, 2 weeks, 3, 6, 12 and 24 months post-operative value was 12.2 ± 6.6°, 19.9 ± 9.7°, 16.5 ± 6.4°, 16.1 ± 7°, 16.2 ± 7.6°, 16.0 ± 6.7° in the group A, respectively, and 12.5 ± 7.1°, 21.1 ± 11.9°, 20.1 ± 7.7°, 19.8 ± 8.3°, 19.3 ± 8.6°, 19.1 ± 7.9° in the group B, respectively. Concerning Fused segment angle, the pre-operative, 2 weeks, 3, 6, 12 and 24 months post-operative value was 5.0 ± 7.5°, 13.9 ± 6.1°, 12.3 ± 6.3°, 12.0 ± 6.4°, 11.1 ± 6.8°, 10.8 ± 6.5° in the group A, respectively, and 6.4 ± 8.6°, 13.1 ± 6.6°, 12.6 ± 7.1°, 12.4 ± 7.4°, 11.5 ± 7.2°, 11.4 ± 7.5° in the group B, respectively. The disc height was 5.1 ± 1.1, 8.6 ± 1.8, 6.8 ± 0.7, 6.6 ± 0.9, 6.5 ± 0.9, 6.5 ± 0.8 mm, pre-operatively, 2 weeks, 3, 6, 12 and 24 months post-operatively in the group A and 5.0 ± 0.9, 8.1 ± 1.4, 7.2 ± 1.1, 7.0 ± 1.1, 6.8 ± 1.2, 6.7 ± 1.0 mm in the group B, respectively. Loss of cervical lordosis was more pronounced in group A (3.9 ± 3.7°) than group B (2.0 ± 1.0°) at 24 months post-operatively (P = 0.014). The loss in the fused segment angle was significantly greater in group A (3.1 ± 2.7°) than group B (1.7 ± 2.1°) (P = 0.039). The loss of disc height was higher in group A (2.1 ± 1.4 mm) than group B (1.4 ± 0.8 mm) at the last follow-up (P = 0.030). Cage subsidence at 3 months occurred in 11/84 segments in group A and 4/78 segments in group B (P = 0.08). Another two segments in group A and another one segment in group B subsided at 6 months postoperatively. Only one segment in group A subsided at 12 months postoperatively with no additional subsidence at 24 months. 78.9 % (15/19) of cage subsidence altogether happened at 3 months after surgery. The subsidence rate showed significant difference between groups (P = 0.043) at the last-follow-up.
Discussion
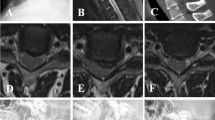
Anterior cervical discectomy and fusion is considered to be the gold standard in the treatment of the cervical spondylopathy which can remove all the compressing structures such as protruded discs and osteophytes, and restore the cervical curvature simultaneously [4]. Besides, the anterior cervical plating enhances the stability of cervical spine and may avoid the risk of pseudarthrosis [2, 3]. However, the plate-related complications are of significant concern. The rate of plate-related complications has been shown to rise in direct proportion to the number of fused segments [2, 5]. The self-anchored stand-alone cages, which have zero profile, have been developed to avoid plate-related complications and shorten the operation time. Besides, the anchored micro-plates claim to offer a comparable immediate stability to that obtained with the use of anterior plates and screws [9] (Fig. 4).
A 58-year-old patient who underwent three-level ACDF using stand-alone cages showing good position of cage at C4/5, C5/6, C6/7 levels and satisfactory alignment of the cervical spine at each time point of follow-up: a pre-operatively; b 2 weeks post-operatively; c 3 months post-operatively; d 6 months post-operatively; e 24 months post-operatively
The success of the ACDF relies on a thorough decompression and achievement of solid intervertebral fusion. Biomechanical studies have revealed that the self-locking stand-alone cage provides less stiffness of cervical spine as locking plate does in 2 or 3-level instrumentation [14, 15]. But high fusion rate can be achieved using these kinds of cages for the treatment of single-level, double-level, and even three-level cervical spondylopathy (Table 3) [7–10, 16–18]. In our study, the nonunion rate was not statistically significant between groups [4.3 % (4/28) vs 7.7 % (2/26)] (P = 0.736). Patients experienced at least one pseudarthrosis were all asymptomatic without requiring revision surgery. This demonstrated that ACDF using self-locking cages can achieve a similar fusion rate as the PEEK cage and plate system. However, the potential measurement error must be taken into consideration. Since it is challenging to precisely assess the bone bridge formation and measure the motion on the flexion–extension lateral radiographs, we must acknowledge that routine use of CT scans may not be possible in resource-restricted settings [19]. Additionally, meticulous preparation of the endplate is necessary to avoid pseudarthrosis with ACDF, as exposure of the subchondral bone could lead to an increase in the fusion rate.
Cage subsidence has been one of the most important complications since the stand-alone cage entered clinical use. Earlier studies have reported varied incidence of subsidence ranging from 0 to 61 % with ACDF with stand-alone cages similar to that used in this study (Table 3) [8, 10, 16, 17]. Wang et al. [16] had reviewed 16 patients with 32 noncontiguous levels who underwent skip-level ACDF with self-locking stand-alone PEEK cages. Their results showed three cages (3/32) in two patients (2/16) suffered from subsidence. A retrospective study by Zhou et al. [10] evaluated the efficacy and outcomes in 15 patients treated with a 3-level ACDF using self-locking stand-alone cages. Four inserted cages in three patients subsided in their study. The subsidence rate per level was similar in these two studies, but the subsidence rate per patient increased with the increased number of fused segments. Besides, all three patients who experienced subsidence in the study by Zhou et al. were all older women, which supports the hypothesis that a lower bone mineral density of the vertebral body could be a key reason for subsidence. Furthermore, damage of the endplate, over-distraction of the index segment, or usage of oversized cages were thought to have contributed to the observed subsidence [17, 20]. Researchers found that cage subsidence often occurs within 3 months after surgery [13, 21], for the formation of bone fusion at 3 months after surgery may restrain the further progress of subsidence. In our study, 78.9 % (15/19) of cage subsidence was detected at 3 months after surgery which supports the above hypothesis (Fig. 5). The observation that loss of disc height was higher in group A (14/84) than group B (5/78) also suggests a vital role of anterior plate in preventing the subsidence. One explanation can be that the force was conducted through anterior plate with less contact stress at graft/bone interfaces hence the subsidence was reduced.
A 63-year-old patient with segmental kyphosis, who underwent three-level ACDF using stand-alone cages, showing cage subsidence at C5/6 levels at 3 months post-operatively which associated with loss of cervical Cobb’s lordosis and fused segment angle: a pre-operatively; b 2 weeks post-operatively; c 3 months post-operatively; d 6 months post-operatively; e 24 months post-operatively
Maintenance of cervical disc height after surgery is crucial, as it was reported that the disc height collapse may result in kyphosis formation and accelerate the adjacent segment degeneration in the long-term [6, 17, 19, 21]. In our study, patients in both groups showed a significant improvement in cervical lordosis and fused segment angle compared to pre-operation status at each time point. These results are consistent with earlier studies [7–10, 17, 20]. However, we found that the loss of cervical lordosis and the fusion segment angle in group A were more significant at the last follow-up. This may be attributed to the different speeds of disc height loss between groups. The plate curve helps to preserve the loss of global cervical lordosis and the fusion segment angle with the prevention of the cage subsidence during the process of fusion [22].
As for clinical results, Zajonz et al. reviewed 18 studies (published between 1999 and 2013) that included a total of 1468 subsidence cases following ACDF and found that clinical outcomes at about 24 months after surgery were unaffected by subsidence [23]. Our findings are consistent with the previous studies that reported post-operative clinical improvement in both groups as assessed by NDI and JOA scores. The scores were not significantly different between groups at each time point [9, 10]. No significant difference was found according to Odom’s criteria in surgical results between groups. Nevertheless, the potential long-term drawbacks associated with subsidence should always be considered.
Dysphagia is common after anterior cervical spine surgery especially in the multi-level ACDF [11, 24, 25]. Although the pathogenesis of the dysphagia is yet to be precisely known, it has been reported that the zero-profile designed stand-alone cage may effectively reduce the incidence of long-term dysphagia without irritation of implants which were directly placed posterior to the esophagus [2, 24]. In addition, some authors suggest that post-operative dysphagia may be caused by direct trauma to the esophagus and its surrounding tissue during the surgery [2, 25]. The self-locking stand-alone cage can make the operative procedure simpler with less retraction of the esophageal. The study by Wang et al. [9] showed that the zero-profile stand-alone cage was associated with a significantly lower risk of dysphagia (0/30) at 3 months postoperatively compared with anterior plate (9/33). Our study showed a lower rate of dysphagia in group A compared to group B at each time point, but with no statistically significant difference. The shorter operation time and less blood loss of ACDF using self-locking stand-alone cage indicates less traction time and less damage of prevertebral soft tissues during surgery, which may contribute to the relatively low rate of dysphagia. But we have suggested that this advantage of zero-profile cage was marginal, since evidence shows that dysphagia rate significantly decreases within 6 months and only few patients experience moderate or severe symptoms beyond 6 months post-operatively even with the use of anterior plate [2, 24]. In our study, only one patient in groups B experienced mild dysphagia at the last follow-up.
There were some limitations in our study, such as the difficulty in the assessment of bone fusion with plain radiographs, and non-feasibility of assessing every patient with CT scan. Thus, the possibility of potential errors needs to be accounted for in the analysis. Besides, the relationship between the bone mineral density and cage subsidence was not analyzed in this article. Changes in the dynamics of the cervical spine after these two procedures were neither studied. Furthermore, this is a retrospective study involving a small number of patients with a relatively short period of follow-up, and robust randomized multi-center prospective studies with long-term follow-up are needed to confirm these findings.
Conclusions
ACDF using self-locking stand-alone cages can help achieve similar clinical results as that achieved by ACDF using cage and plate fixation for the treatment of three-level cervical spondylopathy. However, surgeons should be aware of the potential long-term drawbacks associated with post-operative cage subsidence and loss of cervical lordosis and fused segment angle in patients with ACDF using self-locking stand-alone cages. Further, precautions should be taken to prevent nonunion in case of multi-level lesions.
References
Smith GW, Robinson RA (1958) The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am 40:607–624
Yang L, Gu Y, Liang L, Gao R, Shi S, Shi J, Yuan W (2012) Stand-alone anchored spacer versus anterior plate for multilevel anterior cervical diskectomy and fusion. Orthopedics 35:e1503–e1510
Wang JC, McDonough PW, Kanim LE, Endow KK, Delamarter RB (2001) Increased fusion rates with cervical plating for three-level anterior cervical discectomy and fusion. Spine 26:643–646
Papadopoulos EC, Huang RC, Girardi FP, Synnott K, Cammisa FP (2006) Three-level anterior cervical discectomy and fusion with plate fixation. Spine 31:897–902
Ning X, Wen Y, Xiao-Jian Y, Bin N, De-Yu C, Jian-Ru X, Lian-Shun J (2008) Anterior cervical locking plate-related complications; prevention and treatment recommendations. Int Orthop 32:649–655
Gercek E, Arlet V, Delisle J, Marchesi D (2003) Subsidence of stand-alone cervical cages in anterior interbody fusion: warning. Eur Spine J 12:513–516
Zhou J, Xia Q, Dong J, Li X, Zhou X, Fang T, Lin H (2011) Comparison of stand-alone polyetheretherketone cages and iliac crest autografts for the treatment of cervical degenerative disc diseases. Acta Neurochir 153:115–122
Grasso G, Giambartino F, Tomasello G, Iacopino G (2014) Anterior cervical discectomy and fusion with roi-c peek cage: cervical alignment and patient outcomes. Eur Spine J 23:650–657
Wang Z, Jiang W, Li X, Wang H, Shi J, Chen J, Meng B, Yang H (2015) The application of zero-profile anchored spacer in anterior cervical discectomy and fusion. Eur Spine J 24:148–154
Zhou J, Li X, Dong J, Zhou X, Fang T, Lin H, Ma Y (2011) Three-level anterior cervical discectomy and fusion with self-locking stand-alone polyetheretherketone cages. J Clin Neurosci 18:1505–1509
Bazaz R, Lee MJ, Yoo JU (2002) Incidence of dysphagia after anterior cervical spine surgery: a prospective study. Spine 27:2453–2458
Odom GL, Finney W, Woodhall B (1958) Cervical disk lesions. J Am Med Assoc 166:23–28
Thom C, Krauss JK, Zevgaridis D (2004) A prospective clinical comparison of rectangular titanium cages and iliac crest autografts in anterior cervical discectomy and fusion. Neurosurg Rev 27:34–41
Scholz M, Schleicher P, Pabst S, Kandziora F (2015) A zero-profile anchored spacer in multilevel cervical anterior interbody fusion. Spine 40:E375–E380
Clavenna AL, Beutler WJ, Gudipally M, Moldavsky M, Khalil S (2012) The biomechanical stability of a novel spacer with integrated plate in contiguous two-level and three-level acdf models: an in vitro cadaveric study. Spine J 12:157–163
Wang HR, Li XL, Dong J, Yuan FL, Zhou J (2013) Skip-level anterior cervical discectomy and fusion with self-locking stand-alone peek cages for the treatment of 2 noncontiguous levels of cervical spondylosis. J Spinal Disord Tech 28:E286–E292
Kim CH, Chung CK, Jahng T, Park SB, Sohn S, Lee S (2015) Segmental kyphosis after cervical interbody fusion with stand-alone polyetheretherketone (peek) cages. J Spinal Disord Tech 28:E17–E24
Hofstetter CP, Kesavabhotla K, Boockvar JA (2015) Zero-profile anchored spacer reduces rate of dysphagia compared with ACDF with anterior plating. J Spinal Disord Tech 28:E284–E290
Yang JJ, Yu CH, Chang B, Yeom JS, Lee JH, Lee C (2011) Subsidence and nonunion after anterior cervical interbody fusion using a stand-alone polyetheretherketone (peek) cage. Clin Orthop Surg 3:16
Kao T, Wu C, Chou Y, Chen H, Chen W, Tsou H (2014) Risk factors for subsidence in anterior cervical fusion with stand-alone polyetheretherketone (peek) cages: a review of 82 cases and 182 levels. Arch Orthop Traum Su 134:1343–1351
Fujibayashi S, Neo M, Nakamura T (2008) Stand-alone interbody cage versus anterior cervical plate for treatment of cervical disc herniation: sequential changes in cage subsidence. J Clin Neurosci 15:1017–1022
Chung CK, Kim CH (2012) Anterior plating is better than the stand-alone cage in the restoration of segmental kyphosis. Spine J 12:S100
Zajonz D, Franke A, von der Höh N, Voelker A, Moche M, Gulow J, Heyde C (2014) Is the radiographic subsidence of stand-alone cages associated with adverse clinical outcomes after cervical spine fusion? An observational cohort study with 2-year follow-up outcome scoring. Patient Safety Surg 8:43
Wang Z, Zhu R, Yang H, Gan M, Zhang S, Shen M, Chen C, Yuan Q (2014) The application of a zero-profile implant in anterior cervical discectomy and fusion. J Clin Neurosci 21:462–466
Son DK, Son DW, Kim HS, Sung SK, Lee SW, Song GS (2014) Comparative study of clinical and radiological outcomes of a zero-profile device concerning reduced postoperative dysphagia after single level anterior cervical discectomy and fusion. J Korean Neurosurg S 56:103
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the studies.
Rights and permissions
About this article
Cite this article
Chen, Y., Lü, G., Wang, B. et al. A comparison of anterior cervical discectomy and fusion (ACDF) using self-locking stand-alone polyetheretherketone (PEEK) cage with ACDF using cage and plate in the treatment of three-level cervical degenerative spondylopathy: a retrospective study with 2-year follow-up. Eur Spine J 25, 2255–2262 (2016). https://doi.org/10.1007/s00586-016-4391-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4391-x