Abstract
A prospective observational study was conducted on patients undergoing posterior lumbar spine surgery for degenerative spinal disorders. The study purpose was to evaluate the effect of wait time to surgery on patient derived generic and disease specific functional outcome following surgery. A prolonged wait to surgery may adversely affect surgical outcome. Although there is literature on the effect of wait time to surgery in surgical fields such as oncology, cardiac, opthamologic, and total joint arthroplasty, little is known regarding the effect of wait time to surgery as it pertains to the spinal surgical population. Consecutive patients undergoing elective posterior lumbar spinal surgery for degenerative disorders were recruited. Short-Form 36 and Oswestry disability questionnaires were administered (pre-operatively, and at 6 weeks, 6 months, and 1 year post-operatively). Patients completed a questionnaire regarding their experience with the wait time to surgery. The study cohort consisted of 70 patients with follow-up in 53/70 (76%). Time intervals from the onset of patient symptoms to initial consultation by family physician through investigations, spinal surgical consultation and surgery were quantified. Time intervals were compared to patient specific improvements in reported outcome following surgery using Cox Regression analysis. The effect of patient and surgical parameters on wait time was evaluated using the median time as a reference for those patients who had either a longer or shorter wait. Significant improvements in patient derived outcome were observed comparing post-operative to pre-operative baseline scores. The greatest improvements were observed in aspects relating to physical function and pain. A longer wait to surgery was associated with less improvement in outcome following surgery (SF-36 domains of BP, GH, RP, VT). A longer wait time to surgery negatively influences the results of posterior lumbar spinal surgery for degenerative conditions as quantified by patient derived functional outcome measures. The parameters of pain severity and physical aspects of function appear to be the most significantly affected.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lumbar spine surgery for degenerative conditions is a common aspect of many surgical practices. In carefully selected patients, surgery can provide significant pain relief and positively impact quality of life and physical function [9, 10]. The effect of a prolonged wait to surgery can have detrimental effects on patient perceived function and quality of life not only while waiting for surgery but also in negatively impacting surgical outcome [8, 14, 16, 18]. Little is known regarding the impact of wait time to surgery on outcome in spinal surgery [13].
The reported literature on the impact of wait time to surgery on surgical outcome for elective procedures includes joint arthroplasty for arthritis [8, 11, 14, 16]. Garbuz et al. [8] reported in 221 patients with osteoarthritis on the waiting list for primary total hip arthroplasty (THR) that the odds of achieving better than expected post-operative patient reported functional outcome decreased by 8% for each month on the waiting list with a wait longer than 6 months resulting in a 50% reduction in the odds of achieving a better than expected outcome. Ostendorf et al. [16] demonstrated in 161 patients waiting for THR that patient reported disease-specific functional outcome measures deteriorated while on the waiting list for surgery. Of the limited literature in spinal surgery, a retrospective study by Lofvendahl [13] et al. focused upon 1,336 surgical patients who underwent surgery for hip arthroplasty, lumbar surgery, and arthroscopic knee surgery. The authors observed in the 321 patients that underwent lumbar surgery that non-working patients and those that had a longer delay before first contact with health services spent a longer time on the waiting list [13]. Sixty-four percent of patients thought that their surgical wait time was acceptable. Patients who underwent lumbar surgery in a community-hospital setting had a shorter wait than those undergoing surgery in a tertiary/university-based hospital [13]. Patients who were either dissatisfied with the overall results of their operation or had their surgical date changed during the course of their care were more likely to consider that their surgical wait was unacceptable (Odd’s ratio 3.43 and 2.55, respectively) [13].
The primary study purpose was to evaluate the effect of wait time on surgical outcome in elective posterior lumbar spinal surgery as quantified by patient derived generic and disease specific functional outcome measures. Secondarily, the authors aimed to determine patients’ perception on their experience with wait times through the course of their medical and surgical treatment.
Patients and methods
A prospective prognostic study was conducted on 70 consecutive patients who underwent elective posterior lumbar spinal surgery for degenerative conditions between January 2003 and March 2005. Institutional review board approval was obtained for the study. Surgery was performed at a single university-affiliated tertiary care institution by two fellowship-trained spinal surgeons. Indications for surgery included back, buttock and/or lower extremity pain of spondylogenic origin. Patients undergoing decompression and/or lumbar fusion were included. Patients were excluded from the study if they were not capable of completing the questionnaires (e.g. cognitive or language limitations) or declined participation in the study. There was no formalized prioritization system and patients were placed on an individual surgeons’ waiting list at the discretion of the operating surgeon. Both surgeons had the same access to operating room time.
Study personnel not involved in the patient’s care and blinded to outcome status sent study patients questionnaires before surgery and at 6 weeks, 6 months and 1 year following surgery. Pre-operatively, patients completed a generic health status measure (Short-Form 36) and a disease specific questionnaire (Oswestry disability index; ODI) that the operating surgeon was blinded to. At final follow-up, patients were interviewed by an independent evaluator and were questioned to their opinion regarding aspects of their wait for assessment, investigations.
Several time interval parameters from the onset of patient symptoms to the time of surgery were recorded (Table 1). The chronicity of pre-operative symptoms was recorded as the time from the onset of patient symptoms to the time of surgery (time interval ‘A’). The time from the onset of patient symptoms to initial health services contact (i.e. an initial visit with the primary care physician) was recorded. The time of presentation to primary care physician through to the date of surgery was considered the total wait time regarding a patient seeking initial medical attention for their symptoms, through investigations, specialty referrals, conservative treatment, and spinal surgical assessment to surgery ultimately being performed for their presenting symptoms (time interval ‘B’). We also recorded the time from presentation to primary care physician to the first spinal surgical specialty visit (time interval ‘C’) and also the time from initial spinal surgical consultation through to surgery. Acknowledging that additional investigation or non-surgical therapies may be recommended following initial surgical consultation, time interval ‘D’ recorded the actual time spent on the surgical waiting list following documented surgeon-patient informed consent to proceed with surgery.
Statistical analysis was performed by a statistician using SAS9® (SAS Institute Inc., NC, USA). Surgical success was analyzed by repeated measures analysis of functional outcome measures comparing pre-operative to post-operative values. To test the relationship between wait time and patient derived surgical outcome, Cox regression analysis (Proportional-Hazards model) was performed comparing a patient’s baseline pre-operative score to their most recent follow-up score. Analysis was performed controlling for the effects of baseline covariates (age, gender, co-morbidity, and surgery type) [2]. Results are reported as a Hazard’s ratio with a 95% confidence interval. The median wait time for the time intervals evaluated was used as a reference for those patients who had either a longer or shorter wait to surgery. Patient and surgical demographics were evaluated comparing patients with either a longer or shorter wait to surgery. Statistical significance was set at P < 0.05.
Results
Fifty-three of 70 (76%) patients enrolled in the study had completed follow-up. Of those patients that did not complete follow-up, there were seven patients that moved residences out of the region and declined ongoing participation, there was one patient that did not complete the follow-up period and died from a stroke 6 months post-operatively that was opined to be un-related to the spinal surgery performed, and there were 3 patients that declined ongoing participation following surgery. Finally six patients were lost to follow-up despite attempts to locate them by telephone and correspondence to last known mailing address. Comparing those patients lost to follow-up to those who completed the study follow-up period, baseline demographics including functional outcome scores were not significantly different (P > 0.05). Of the 53 patients, the average age at surgery was 52 (range 25–85) and the male:female ratio was 0.83:1. Of the 53 spinal procedures, 12 were revision operations. Charlson co-morbidity index was zero in 44/53 (83%) patients, one in 6/53 (11%) patients, two in 2/53 (4%) patients, and three in 1/53 (2%) patients. Additional diagnostic and surgical demographics are listed in Table 2. Early surgical complications included two patients who sustained an intra-operative incidental durotomy that required repair. One patient developed a superficial wound infection following a single level lumbar decompression and instrumented fusion that required surgical irrigation and wound debridement 2 weeks following surgery. The infection resolved following a subsequent course of oral anti-microbial therapy. Late surgical complications included one patient that developed a recurrent disc herniation 10 months following index surgery that required a revision discectomy. Two additional patients reported ongoing radicular symptoms that required revision surgical decompression 1 year following their index surgeries. One patient reported ongoing symptoms relating to implant prominence following a multilevel lumbar decompression and instrumented fusion that required later staged implant removal following radiographic fusion.
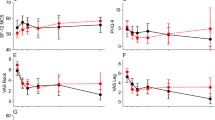
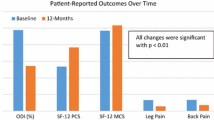
Post-operative functional outcome scores
Statistical improvements in patient reported generic and disease specific measures were observed comparing post-operative to pre-operative baseline scores (Table 3, Fig. 1). The greatest improvements were observed in parameters relating to physical aspects of function. Significant improvements were observed at 6 weeks for SF-36 domains bodily pain (P < 0.03), physical function (P < 0.01), social functioning (P < 0.03), PCS (P < 0.002), and ODI scores (P < 0.004). Further improvements were observed by 1 year for SF 36 domain scores of bodily pain (P < 0.0001), physical functioning (P < 0.0001), role emotional (P < 0.0016), role physical (P < 0.0001), social functioning (P < 0.0001), social functioning (P < 0.001), vitality (P < 0.004), PCS (P < 0.0001), and ODI scores (P < 0.0001). Using Deyo et al.’s [7] suggested clinically important difference of seven points for each domain of the SF-36, the observed statistical differences in the six of eight domains would also all be considered clinically significant differences. The mean difference between patient specific improvement comparing pre-operative to last follow-up score was 24.7 (16.6–32.8, 95% CI) for SF-36 bodily pain domain, 19.8 (10.8–28.8) physical functioning domain, 19.3 (3.8–34.9) role emotional domain, 29.0 (14.8–43.2) role physical domain, 21.3 (11.6–30.9) social functioning domain, and 9.6 (3.3–15.9) vitality domain. Mean patient specific improvement in SF-36 physical component score was 9.5 (5.8–13.3) and 3.7 (−0.9 to 8.3) for the mental component score. A reduction in disability of on average 16.6% (95% confidence interval of 11–22%) was observed in ODI over the study follow-up period.
Wait time and functional outcome scores
Wait times through the health service system for the time intervals evaluated are listed in Table 4. For those patients above the median wait time, the average time was 1,343.7 ± 1,732.5 days, 496 ± 510.2 days, 155.8 ± 101.4 days, 166.0 ± 95.0 days for time intervals A, B, C, and D, respectively. Fifteen percent of patients required additional investigations and/or consultations following their initial spinal surgical clinic visit. Four percent of patients were recommended additional conservative treatment following their initial spinal surgical consultation which was not successful and these patients ultimately underwent surgery. One patient initially declined recommended surgery following initial consultation and decided in clinical follow-up to proceed with surgery.
A longer wait to surgery was associated with a lower likelihood of improvement in some functional outcome scores following surgery over all wait time periods evaluated (Table 5). Statistically significant observations were observed in SF-36 domains of bodily pain, general health, role physical, vitality, and PCS scores. A longer surgical waiting list time resulted in less improvement in patient reported SF-36 PCS (Hazard’s ratio 3.53, P < 0.02) in addition to SF-36 general health (Hazard’s ratio 2.34, P < 0.03) and role physical domain scores (Hazard’s ratio 2.31, P = 0.03). In general there was a longer wait time for those patients who required spinal fusion when compared to those where fusion was not performed (P = 0.02 for time intervals B and C; P = 0.04 for time interval D). Patient age, gender, and co-morbidity was not associated with a longer wait time although pre-operative SF-36 PCS, role physical domain score, and ODI was worse on average in those patients that had a shorter wait to surgery when compared to the median wait time of the study cohort (Table 6). As aforementioned, surgery type was controlled for as a co-variate in the statistical model when determining the association between wait time to surgery and the extent of improvement in post-operative functional outcome scores when compared to pre-operative baselines.
In regards to patient perception regarding their wait time during the course of their spinal treatment (Table 7), 76% of patients reported being satisfied with the outcome of their surgery and 81% of patients indicated that their duration of wait to surgery was acceptable. Approximately 40% of patients believed the waiting time had a negative impact on their perceived clinical condition, physical and mental well-being. Forty-seven percent of patients reported seeking alternate forms of treatment prior to surgery and 32% of patients indicated that they sought a second surgical opinion prior to surgery. Patients who reported positive (good or excellent) satisfaction with their surgical results were also more likely to indicate that their waiting time to surgery was acceptable (r = 0.74, P < 0.0001). Twenty-eight percent and 26%, respectively, believed they waited too long for imaging or a specialist opinion and from specialist opinion to surgery. However, only 2% of patients indicated that they were prepared to pay to expedite their imaging and/or specialty consult and 26% indicated that they would use friends and/or contacts to expedite clinical and radiologic assessments.
Discussion
In any health care delivery model timely access for those patients that can benefit from spinal surgical treatment is important. The impact of wait time to surgery or a delay to surgery because of factors that can be controlled or improved upon is important to health delivery outcomes. The results of our prospective observational study in this spinal population corroborate the notion that a longer wait to surgery including time spent on the actual surgical waiting list can adversely influence the results of surgery as quantified by patient derived functional outcome measures. Statistical differences in some areas of the patient reported functional improvement was observed in all of the wait time intervals evaluated in the present study which highlights the importance of considering several variables associated with health care delivery. Parameters that appear most affected by a longer wait to surgery included physical function and subjective pain severity measures.
As anticipated, posterior lumbar surgery for degenerative conditions of the lumbar spine can significantly improve patient reported functional outcome. Using generic and disease specific measures, statistical improvements were observed in our study comparing patient pre-operative to post-operative scores. The greatest improvements in patient derived outcome scores were observed in parameters relating to physical aspects of function. Even with surgical treatment, improvements to post-operative SF-36 PCS at last follow-up were still on average 1 SD below age and gender matched national norms. Although spinal surgery appears to have the greatest impact on patient parameters relating to physical aspects of function, improvements in these parameters following surgery also appeared the most affected if there was a longer wait to surgery. Of interest in the various wait time intervals evaluated in the present study, the actual time spent on the surgical waiting list was associated with the greatest impact on patient reported physical function (Hazard’s ratio 3.53 for SF-36 PCS). Although a longer wait for spinal surgery may result in a lower likelihood of improvement following surgery what constitutes an unacceptable or prolonged delay in the wait requires more extensive and ongoing study. In our study, the median time from patient initiated health services contact through to surgery was 196 days. The median time for patients enrolled on the surgical waiting list was 92 days.
A limitation of several studies evaluating the effect of wait time on surgical outcome includes focusing upon the wait time from time of enrollment onto the surgical waiting list [8, 11, 16]. As highlighted in this study, it is important to consider several variables that may be associated in the wait to surgery from the time of patient initiated medical consultation for treatment. Additional study strengths compared to other surgical wait time studies include utilizing functional outcome measures that incorporate the evaluation of patient specific improvement in scores compared to baseline when contrasted to other studies that report an non-patient specific aggregate analysis of mean scores [6, 11, 14]. A limitation of our study is the authors did not evaluate a patient’s potential deterioration during their wait. Ostendorf et al. [16] observed that disease specific scores demonstrated a significant deterioration during the time spent on the surgical waiting list for THR. In addition, the patients were provided a questionnaire regarding their experience with the wait time to surgery administered at the last follow-up and not at the time of surgical booking or initial spinal surgical consultation. This may introduce potential recall bias. Not unexpectedly we observed that patients who were more satisfied with the results of their surgery also reported greater acceptance with the time they had to wait through the course of treatment which is consistent to the observations of Lofvendahl et al. [13]. The presence and extent of clinical physical parameters such as neurologic strength and joint range of motion in addition to radiographic parameters was also not evaluated as the primary outcome measure was patient derived functional outcome. An additional study limitation is the length of follow-up to 1-year.
The generalizability of our study results to other spinal surgical practices warrants discussion. Medical coverage for the patients evaluated in the study was provided by a universal regionally based health provider where individual patients cannot self-refer to a surgeon for a spinal surgical consultation without first consulting a primary care physician who would decide upon whether additional investigations and referrals are warranted. Patients were prioritized on the surgical waiting list at the sole discretion of the operating surgeon and not on the basis of a formalized prioritization system. Surgery was performed at a tertiary university affiliated institution and the spectrum of spinal disorders, type of surgery, and chronicity of pre-operative symptoms to be assessed by tertiary care specialists may vary compared to spinal surgeons involved in primarily community-based practices. In the retrospective series reported by Lofvendahl et al. [13], the authors reported that patients who underwent lumbar surgery in a community-hospital setting had a shorter wait than those undergoing surgery in a tertiary/university-based hospital. In addition, the vast majority of patients who were seen in the spinal surgical clinic of the surgeons involved in our study had radiologic imaging either in the form of a CT scan or MRI scan prior to initial spinal surgical consultation. Concordantly, additional delays to surgery following initial spinal surgical consultation for additional investigations or pre-surgical therapies accounted for fifteen percent of the study cohort.
Utilizing the median wait time as a reference for those patients with either a longer or shorter wait to surgery, we observed that patients with a shorter wait also reported lower pre-operative SF-36 PCS, role physical domain scores, and greater disability on ODI scores. Despite lower baseline SF-36 scores and greater ODI disability, these patients demonstrated a greater improvement in SF-36 scores and ODI disability when compared to those patients that had a longer wait. Although the surgeons involved in the study were blinded to patient functional scores in their surgical prioritization, surgeon selection bias in identifying those patients with a greater self-perceived impact of their spinal condition might in part explain the observation of lower baseline scores in the parameters indicated for the shorter wait group. It is also important to note that the effect of surgery type was controlled for as a co-variate in the statistical model when determining the association between wait time to surgery and the extent of improvement in post-operative functional outcome scores when compared to pre-operative baselines.
Existing strategies to address wait time pose certain advantages and disadvantages. Economic evaluation with prioritization based upon a minimal costs concept by virtue of design places less importance upon clinical impressions of surgical urgency [4]. Surgeon based prioritization is based upon the assumption that a surgeon can accurately predict those patients that may gain the most benefit from surgical intervention. However, physician derived measures of outcome do not necessarily correlate well with patient derived measures of outcome although there are conflicting reports in the literature [1, 12, 17]. Strategies that streamline patients to those surgeons with a shorter surgical waiting list may not necessarily result in improvements in overall surgical outcomes as several factors are important in the successful provision of spinal surgical care [3, 19]. Educational programs directed towards improving health-related quality of life in patients on the surgical waiting list show promise. However, this does not address the underlying issue of the impact of the actual length of wait as it pertains to physical functioning parameters [15]. Medical expert consensus based criteria tools for prioritizing patients on the waiting list for surgery may facilitate a more broad based specialty equity in the access to surgical treatment [5].
In conclusion, a longer wait time to surgery negatively influences the results of posterior lumbar spinal surgery for degenerative conditions as quantified by some patient derived functional outcome measures. The parameters of pain severity and physical aspects of function appear to be the most significantly affected. Although the majority of patients in the present study indicated that the time spent on the surgical waiting list was acceptable, approximately 40% of patients did believe that the time spent on the surgical waiting list negatively impacted their perception of their physical and mental well-being. An ongoing dialogue transcending current infrastructural levels of health care delivery is required to ensure timely access for those patients that can benefit from spinal surgical treatment.
References
Buchanan R, Birch JG, Morton AA et al (2003) Do you see what I see? Looking at scoliosis surgical outcomes through orthopedists’ eyes. Spine 28(24):2700–2704 (discussion 2705)
Charlson M, Szatrowski TP, Peterson J et al (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47(11):1245–1251
Ciampolini J, Hubble MJ (2005) Early failure of total hip replacements implanted at distant hospitals to reduce waiting lists. Ann R Coll Surg Engl 87(1):31–35
Coast J (1993) The role of economic evaluation in setting priorities for elective surgery. Health Policy 24(3):243–257
Conner-Spady BL, Sanmugasunderam S, Courtright P et al (2005) The prioritization of patients on waiting lists for cataract surgery: validation of the Western Canada waiting list project cataract priority criteria tool. Ophthalmic Epidemiol 12(2):81–90
Derrett S, Paul C, Morris JM (1999) Waiting for elective surgery: effects on health-related quality of life. Int J Qual Health Care 11(1):47–57
Deyo RA, Battie M, Beurskens AJ et al (1998) Outcome measures for low back pain research. A proposal for standardized use. Spine 23(18):2003–2013
Garbuz DS, Xu M, Duncan CP et al (2006) Delays worsen quality of life outcome of primary total hip arthroplasty. Clin Orthop Relat Res 447:79–84
Gibson JN, Grant IC, Waddell G (2000) Surgery for lumbar disc prolapse. Cochrane Database Syst Rev 3:CD001350
Gibson JN, Waddell G, Grant IC (2000) Surgery for degenerative lumbar spondylosis. Cochrane Database Syst Rev 3:CD001352
Kelly KD, Voaklander D, Kramer G et al (2000) The impact of health status on waiting time for major joint arthroplasty. J Arthroplasty 15(7):877–883
Lieberman JR, Dorey F, Shekelle P et al (1996) Differences between patients’ and physicians’ evaluations of outcome after total hip arthroplasty. J Bone Joint Surg Am 78(6):835–838
Lofvendahl S, Eckerlund I, Hansagi H et al (2005) Waiting for orthopaedic surgery: factors associated with waiting times and patients’ opinion. Int J Qual Health Care 17(2):133–140
Mahon JL, Bourne RB, Rorabeck CH et al (2002) Health-related quality of life and mobility of patients awaiting elective total hip arthroplasty: a prospective study. Cmaj 167(10):1115–1121
Nunez M, Nunez E, Segur JM et al (2006) The effect of an educational program to improve health-related quality of life in patients with osteoarthritis on waiting list for total knee replacement: a randomized study. Osteoarthritis Cartilage 14(3):279–285
Ostendorf M, Buskens E, van Stel H et al (2004) Waiting for total hip arthroplasty: avoidable loss in quality time and preventable deterioration. J Arthroplasty 19(3):302–309
Suarez-Almazor ME, Conner-Spady B, Kendall CJ et al (2001) Lack of congruence in the ratings of patients’ health status by patients and their physicians. Med Decis Making 21(2):113–121
Weller I, Wai EK, Jaglal S et al (2005) The effect of hospital type and surgical delay on mortality after surgery for hip fracture. J Bone Joint Surg Br 87(3):361–366
Wiese M, Kramer J, Bernsmann K et al (2004) The related outcome and complication rate in primary lumbar microscopic disc surgery depending on the surgeon’s experience: comparative studies. Spine J 4(5):550–556
Acknowledgments
The authors wish to thank Dr. Marjan Vidmar for his assistance with the study statistical analysis. The authors also acknowledge Ms. Lynn Antwi-Boasiako, Ms. Nana Adjei, Dr. Fathi Elkasah, Dr. Moamer Elnagret, Dr. Abdulhamid Elyousfi, and Ms. Olivia Murnaghan for their contribution to this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
A reviewer’s comment on this paper is available at http://dx.doi.org/10.1007/s00586-007-0453-4.
Rights and permissions
About this article
Cite this article
Braybrooke, J., Ahn, H., Gallant, A. et al. The impact of surgical wait time on patient-based outcomes in posterior lumbar spinal surgery. Eur Spine J 16, 1832–1839 (2007). https://doi.org/10.1007/s00586-007-0452-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-007-0452-5