Abstract
Arthrodesis using interbody cages has demonstrated high fusion rates. However, permanent cages are exposed to stress-shielding, corrosion, and may require explanation when necessary. Polylactic acid (PLA) bioresorbable cages are developed for avoiding these problems, but significant tissue reaction has been reported with 70/30 PLDLLA in some preclinical animal studies. The objective was to evaluate 96/4 PLDLLA cages in a sheep model over 3 years. Sixteen sheeps underwent one level anterior lumbar interbody fusion using 96/4 PLDLLA cages, filled and surrounded with cancellous bone graft from the iliac crest. Six groups of three animals were killed after 3, 6, 9, 12, 24, and 36 months. Harvested lumbar spine had radiographic, MRI, and CT evaluation and histological analysis. Histological results: cage swelling and slight signs of fragmentation associated to fibrocartilaginous tissue apposition at 3 months; bone remodeling around the cage with direct apposition of the mineralization front at 6 months; active cage degradation and complete fusion around the cage at 9 months; cage fragmentation and partial replacement by bone tissue at 12 months; bone bridges in and around the cage at 24 months; full resorption and intervertebral fusion at 36 months. Radiological results: partial arthrodesis at 3 months; definite peripheral arthrodesis at 6 months; similar aspect at 9 months; significant cage resorption at 12 months; definite inner and outer fusion at 24 months; complete cage resorption and calcification at the location of the cage at 36 months confirmed histological observations. Radiographic, CT scan, MRI, and histological data were consistent for showing progressive resorption of 96/4 PLDLLA, interbody fusion, and bone remodeling, with no significant signs of local intolerance reaction. These results are promising and suggest further development of 96/4 PLDLLA cages.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Interbody cages with bone graft are currently successfully used for spinal fusion [2, 30]. Using cages help maintaining lordosis and neuroforaminal distraction and reduce donor site morbidity when compared to tricortical bone graft [24, 27, 31, 32, 51]. However, reported complications of the use of interbody cages include migration, extrusion, pseudarthrosis, and implant subsidence [21, 25, 51, 54]. Being permanent implants, intervertebral cages remain at the risk of secondary infection, possibly requiring difficult removal. In addition, titanium alloy and stainless steel cages have specific disadvantages including stress-shielding due to excessive rigidity, which leads to bone resorption and osteopenia [19, 43]; corrosion, wear debris due to slight motion before achievement of fusion; and possible allergic reactions [16]. Carbon fibers are radiolucent, MRI-compatible, and better match the elasticity modulus of the bone [9]. However, small debris particles have been reported with carbon fiber cages [38]. Cases of rupture of these cages have also been reported [41].
Bioresorbable polymer implants aim at avoiding these complications with self degrading once their mechanical role is over, after achievement of solid bone fusion [5]. Resorbable implants would also facilitate imaging for assessing fusion [28, 39, 47, 48] and allow progressive transfer of the load to the fusion mass [3]. Currently, the most common resorbable biomaterial used in orthopedic and trauma surgery is polylactic acid (PLA). With limited foreign body reaction [12], biocompatibility with neural tissue [46, 22], nerves [13], bone-like low elastic modulus [11], and possibility of association with osteoinductive molecules such as BMP [40], PLA devices represent a promising class of bioresorbable materials with widespread potential in spinal surgery. In addition, the incidence of infections was comparable between resorbable implants and usual metal implant devices [4].
PLA has two forms: poly-(l-lactide), which can be pure (PLLA form), and poly-(d-lactide), which is systematically associated with poly-(l-lactide) (PDLLA form). Their combination constitutes a stereocopolymers poly-(l,dl lactide) (PLDLLA), with varying ratios of each [50], usually 70/30. Kinetics of resorption and strength retention have been investigated [7, 18, 26, 33, 35, 42, 47]. PLDLLA are considered to degrade faster with more tissue reaction as compared with PLLA implants, for which the degradation process has been described to last for several years. The degree of the material’s crystallinity also interferes in determining the occurrence of late degradation [7, 29]. In addition, the biological (vascularization) and the mechanical environment at the implantation site are also important parameters [16].
The goal of this study was to evaluate a new PLDLLA cage, where the L/DL ratio was set at 96/4, in a large animal model for lumbar interbody fusion. The main hypothesis was that the increased proportion of the PLLA form, when compared to 70/30 PLDLLA, would be a good compromise for degradation and fusion kinetics at the lumbar spine. The sheep model was chosen because of similarities with human spine in term of lamellar bone growth rate and biomechanics [52]. Histological and radiological bone formation and implant degradation as a function of time were investigated.
Materials and methods
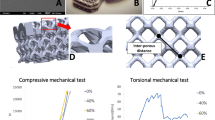
All operative procedures and the animal care complied with the regulations of the legislation for animal research. Sixteen Pre Alps ewes (7 months-old, and 42 kg in average) underwent a left retroperitoneal lumbar approach for single level implantation of the bioresorbable 96/4 PLDLLA cage (PHUSIS-FRANCE) at L3–L4 (Table 1). Muscles of the abdominal wall were opened longitudinally in lateral position. The peritoneum and all retroperitoneal elements were moved medially together for exposuring the lumbar spine. The complete discetomy preserved the posterior longitudinal ligament and the vertebral endplates were reamed until the subchondral bone. The parallelepipedal cage was 22.2 mm long, 9 mm wide, and 9 mm high at one end and 11 mm high at the other end (lordotic cage of 6° angle). The wall thickness was 2.5 mm. It was filled and surrounded with autologous cancellous bone from the iliac crest. The cage was implanted obliquely in order to preserve the common anterior vertebral ligament and to avoid anterior migration. Six groups of two or three animals were sacrificed at 3, 6, 9, 12, 24, and 36 months post-implantation. Oxytetracyclin (30 mg/kg, IV) was administered 15 days and 5 days before sacrifice for labeling bone apposition.
Harvested spinal blocks were X-rayed, and had CT scan (General Electric, volumic acquisition and rebuilding from 1 mm thickness cuts, matrix 512 × 512) and MRI (SIGNA 1 Tesla General Electric, T1 and Fast T2 Fat Sat sagittal and frontal, cuts 3 mm thickness with 0.3 mm gap. Matrix 512 × 512, Fov 20 cm) imaging. Definite fusion was defined as the presence of bone bridges on the CT scan.
The harvested specimens were fixed in 10% buffered formalin, dehydrated in a graded alcohol series, and embedded in polymethylmetacrylate. Two ventro-dorsal parasagittal ground sections were prepared from each specimen using the Donath method for the Exakt system [14]. Histological sections were stained using the modified Paragon method. Qualitative and semi-quantitative analyses of histological inter-body fusion, bone and cell density at the implantation site, degree of tissue differentiation in contact with the cage, mineralization, remodeling, cage resorption, and inflammatory parameters were performed. The assessment of the bone mineralization activity in the interbody space was performed using epifluorescence examination. Observed parameters were quoted 0 to 4 on each histological section (0 = absent, 1 = mild, 2 = moderate, 3 = marked, 4 = very marked or complete) and averaged for each group of animals. The histological analysis was performed according to the NF EN ISO 10993–6 recommendations [1].
Qualitative histopathological examinations (Safranin–Hematoxylin–Eosin-stain) of local and remote tissues (paravertebral muscles and lymph nodes, liver, kidney, and spleen) were performed to determine possible reactions for the degradation products and/or resorption of the material.
Results
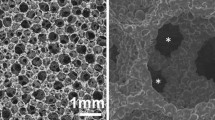
All sheep recovered from anaesthesia uneventfully without signs of neurological deficits. Histological results are summarized in Table 2. Three months after implantation, the cages displayed morphological deformations showing compression of the internal space of the implant by 10–40%, slight undulation of the walls, and limited fragmentation of the material. There was no sign of significant material resorption. However, active peri-implant bone neoformation associated with fibro-cartilaginous tissue was observed. Early centripetal bone in growth ranging from 0 to 60% (Fig. 1) occurred in the inner space of the cage, although no complete bone fusion had taken place. The neuronal and muscle tissues close to the implantation site did not exhibit signs of lesions. Six months following implantation, osteogenesis and bone remodeling around the implants increased. The cages deformations were the same as previously observed and were associated with direct bone-to-implant. Signs of bone fusion were visible outside the implant in all cases. Limited signs of fusion were also observed within the cage. No inflammatory, necrotic, or osteolytic reactions were visible. Fluorescence labeling clearly showed signs of mineralization in direct contact with the cage (Fig. 2). Nine months after implantation, the implant material gradation developed actively. Macro- and micro-particles were visible among macrophages. Fusion occurred at the periphery of the cage in the two animals while noticeable bony growth was seen within the cage in one case. In one ewe, the cage was implanted too much dorsally with direct contact with the dura mater. No local significant inflammatory reaction was reported (Fig. 3). At 12 months post-implantation, deformation and signs of extensive degradation of the implant (fragmentations and erosions) were detected. Approximately 30% of the cage was resorbed and replaced by trabecular bone tissue with structural characteristics similar to those of physiological neighboring bone tissue. The fibro-cartilaginous peri-implant tissue was distinctly thinned. Osteointegration of the cage was associated with pronounced bony growth within the implant without signs of significant inflammatory reaction. Signs of complete interbody arthrodesis were seen within and outside the cage in one animal, and only outside the cage in two animals. At 24 months, resorption of the implant proceeded with more fragmentation. Approximately 40% of the device was resorbed and replaced by trabecular bony tissue. Numerous direct bone-material or fibro-cartilaginous contacts tissue were seen around the implant (Fig. 4). Fusion outside the cage was seen in all cases. Two of the three ewes displayed bone fusion inside and outside the implant. One cage, that was implanted too much dorsally, in direct contact with the dura mater, had a localized and limited granulomatous reaction. No signs of local intolerance were seen around the implant, including the neighboring muscle. At 36 months post-implantation, the two cases exhibited histological fusion in regions of the device, as well as in the periphery of the cage (Fig. 5). In one case, the cage was completely reabsorbed; it was replaced by a fibro-bone marrow tissue containing mesenchymal cells. In the other case, a few remants of the cage were seen, associated with a fibrovascular tissue and bony bridges occupied the space left by the reabsorbed implant. A few macrophages showing blue-stained cytoplasmic inclusions were visible. Within and outside the former cage, the trabecular bone tissue was mature and of similar density as compared to the rest of the vertebral body. Signs of cortical bone formation were seen in one case. Epifluorescence analysis demonstrated mineralization activity in the implanted site, similar to that seen in the rest of the vertebral body. No significant signs of local intolerance reaction were seen either on the implanted site or in the neighboring neuronal or muscle tissues.
Radiological results showed a continuous evolution toward fusion, which was following the histological curse. At 3 months post-implantation, radiological fusion was partial in all cases on standard radiographs; implants remained clearly visible in all cases. CT-scan section showed no bone bridges. At 6 months, radiological intervertebral fusion was definite in all cases on radiographs and CT-scan sections. No specific signal was detected on the MRI in the adjacent bone (Fig. 6). The radiological aspect was similar at 9 months after implantation. At 12 months, the radiological fusion was also definite in all cases in and outside the cage. This was associated with considerable resorption of the cage (Fig. 7). Radiological fusion was definite in all cases after 24 months with confirmed interbody fusion on the CT-scan (Fig. 8). At 36 months, fusion was complete on radiographs and CT scans, with calcification at the site of the degraded cage. The MRI aspect still showed a variation of signal at the location of the former cage; however, adjacent vertebral endplates were physiological (Fig. 9).
Imaging at 36 months post-implantation. All the interbody space is fused with mature bone replacing the fully degraded 96/4 PLDLLA cage (a radiographs, b CT scan); the cage site still had an hydrophilic signal on the MRI (c) with no change of signal in peripheral tissue when compare to adjacent levels
Discussion
The current study investigated lumbar intervertebral fusion using 96/4 PLDLLA cages in an ovine model. In addition to the histological investigation, fusion and tissue response were assessed radiologically. We noted the obvious correspondence between histology and radiology and the absence of material related artifacts. We demonstrated that interbody fusion using 96/4 PLDLLA cages was rapidly achieved, starting around the cage. The “locked pseudarthrosis” area, described as the presence of fibrous tissue with collagen fibers in the fusion zone without enchondral bone formation, when using 70/30 PLDLLA polymer [39], was not encountered in our study. We did not observe a quiescent fibrous tissue layer surrounding the cages and persisting overtime in any of our cases. Direct bone apposition onto the implant was gradually observed. This is in accordance with some previous observations showing direct apposition of bone on the polymeric material with PLDLLA implants and a thin layer of connective tissue with PLLA [6, 23, 43]. By separately analyzing the inner and outer fusion, we observed that peripheral fusion came first, which is in accordance with the notion of radiological sentinel sign for intervertebral fusion [36]. It is likely that the microenvironment (blood supply) is more favorable around than within the cage. We acknowledge that placing autologous bone graft around the cage in addition to within the cage in the protocol made a difference with other animal studies (Table 3). However, the in and out graft is a common procedure in spinal surgery of the anterior column using autologous bone graft, and this had to be taken into account.
Concerning cage degradation and tissue reaction, we observed that the overall original geometry of the 96/4 PLDLLA cages was maintained at 3 and 6 months, with respect to a slight change in shape, that was probably due to the combination of mechanical constraint and swelling of degradation. At 12 months, approximately 30% of the cage was resorbed and no specific inflammatory reaction was seen. Thirty-six months after implantation, the site operated on displayed no signs of significant inflammatory, immunologic, or necrotic reaction.
Some intensive inflammatory tissue response was reported with the use of highly crystalline self-reinforced PGA implants [8, 10, 17, 49]. It was noticeable that the PLA cage in this study was produced with using hydrophilic zinc catalyst in place of the usual hydrophobic stannous octanoate [34], which provides highly crystalline matrix and degradation particles [35].
Chemical composition and L/DL ratio is also a prominent factor influencing tissue response and degradation. Other studies using PDLLA 70/30 cages [15, 20] showed fast degradation associated with an important inflammatory response without allowing definite fusion. Severe foreign body reaction has been using 70/30 PDLLA at the cervical spine in a sheep model [15, 20]. On the other hand, PLA stereoisomers have been shown to generate less soft-tissue reactions [8, 37, 53].
We noted that density of the new bone in the interbody arthrodesis using 96/4 PLDLLA cages was similar in all ways to that of the adjacent vertebral bodies, showing physiological path of mineralization. This is indirectly promising in terms of mechanical quality of the fusion mass; however, our study did not include biomechanical testing and do not allow to state on this point. Since the aim was purely histological with evaluating degradation and fusion, the mechanical issues related to violation of the endplates and cage subsidence were not investigated.
We acknowledge that the study was limited by the number of animals at each retrieval time; however, the number of time points and the long term follow-up did not allow to use more than three large animals per group. In spite of the differences in quality of bone between the sheep and humans, specifically the use of relatively young animals, the promising results in the short and long term incite developing investigations concerning the use of 96/4 PLDLLA as lumbar interbody implant. In addition to the differences in the mechanical environment between sheep and humans, the association with some anterior/posterior spinal instrumentation in human surgery has to be taken into account for interpreting the results of the stand-alone model presented here. However, using bone graft in and around the cage for filling the intervertebral space after discetomy has been inspired from human surgery and improved the realism of the experiment.
Conclusions
The use of 96/4 PLDLLA resorbable cages and autologous bone graft has been shown to lead to appropriate bone fusion at the lumbar spine in the sheep. Gradual resorption of 96/4 PLDLLA demonstrated low potential for foreign body reaction. Specifically, biocompatibility with the dura mater, nervous tissue, and distant organs was confirmed. The promising balance between fusion and degradation of 96/4 PLDLLA intervertebral implants suggests developing this resorbable polymer for spine surgery.
References
AFNOR (2005) [Biological evaluation of medical devices - part 6: local effects after implantation]. J Off Repub Fr 70
Agazzi S, Reverdin A, May D (1999) Posterior lumbar interbody fusion with cages: an independent review of 71 cases. J Neurosurg 91:186–192
Alexander JT, Branch CL Jr, Subach BR et al (2002a) Applications of a resorbable interbody spacer in posterior lumbar interbody fusion. J Neurosurg 97:468–472
Alexander JT, Branch CL Jr, Subach BR et al (2002b) Applications of a resorbable interbody spacer via a posterior lumbar interbody fusion technique. Orthopedics 25:s1185–s1189
An YH, Woolf SK, Friedman RJ (2000) Pre-clinical in vivo evaluation of orthopaedic bioabsorbable devices. Biomaterials 21:2635–2652
Bergsma JE, de Bruijn WC, Rozema FR et al (1995a) Late degradation tissue response to poly(l-lactide) bone plates and screws. Biomaterials 16:25–31
Bergsma JE, Rozema FR, Bos RR et al (1995b) In vivo degradation and biocompatibility study of in vitro pre-degraded as-polymerized polyactide particles. Biomaterials 16:267–274
Bostman O, Pihlajamaki H (2000) Clinical biocompatibility of biodegradable orthopaedic implants for internal fixation: a review. Biomaterials 21:2615–2621
Brantigan JW, Steffee AD (1993) A carbon fiber implant to aid interbody lumbar fusion. Two-year clinical results in the first 26 patients. Spine 18:2106–2107
Casteleyn PP, Handelberg F, Haentjens P (1992) Biodegradable rods versus Kirschner wire fixation of wrist fractures. A randomised trial. J Bone Joint Surg Br 74:858–861
Chen C, Chueh J, Tseng H et al (2003) Preparation and characterization of biodegradable PLA polymeric blends. Biomaterials 24:1167–1173
Ciccone WJ 2nd, Motz C, Bentley C et al (2001) Bioabsorbable implants in orthopaedics: new developments and clinical applications. J Am Acad Orthop Surg 9:280–288
de Medinaceli L, al Khoury R, Merle M (1995) Large amounts of polylactic acid in contact with divided nerve sheaths have no adverse effects on regeneration. J Reconstr Microsurg 11:43–49
Donath K, Breuner G (1982) A method for the study of undecalcified bones and teeth with attached soft tissues. The Sage–Schliff (sawing and grinding) technique. J Oral Pathol 11:318–326
Eindorf T, Pflugmacher R, Koch C et al (2005) Spinal fusion with bioresorbable cages—severe degradation effects. Eur Spine J 14:S20
Gogolewski S (2000) Bioresorbable polymers in trauma and bone surgery. Injury 31(Suppl 4):28–32
Hoffmann R, Krettek C, Hetkamper A et al (1992) [Osteosynthesis of distal radius fractures with biodegradable fracture rods. Results of two years follow-up]. Unfallchirurg 95:99–105
Hollinger JO, Battistone GC (1986) Biodegradable bone repair materials. Synthetic polymers and ceramics. Clin Orthop 290–305
Kanayama M, Cunningham BW, Haggerty CJ et al (2000) In vitro biomechanical investigation of the stability and stress-shielding effect of lumbar interbody fusion devices. J Neurosurg 93:259–265
Kandziora F, Pflugmacher R, Scholz M et al (2004) Bioabsorbable interbody cages in a sheep cervical spine fusion model. Spine 29:1845–1855
Kuslich SD, Danielson G, Dowdle JD et al (2000) Four-year follow-up results of lumbar spine arthrodesis using the Bagby and Kuslich lumbar fusion cage. Spine 25:2656–2662
Lundgren D, Nyman S, Mathisen T et al (1992) Guided bone regeneration of cranial defects, using biodegradable barriers: an experimental pilot study in the rabbit. J Craniomaxillofac Surg 20:257–260
Mainil-Varlet P, Rahn B, Gogolewski S (1997) Long-term in vivo degradation and bone reaction to various polylactides. 1. One-year results. Biomaterials 18:257–266
McAfee PC (1999a) Interbody fusion cages in reconstructive operations on the spine. J Bone Joint Surg Am 81:859–880
McAfee PC, Cunningham BW, Lee GA et al (1999b) Revision strategies for salvaging or improving failed cylindrical cages. Spine 24:2147–2153
Merloz P, Minfelde R, Schelp C et al (1995) [In vitro study of the properties of bioresorbable lactic acid polymer materials]. Rev Chir Orthop Reparatrice Appar Mot 81:433–444
Onesti ST, Ashkenazi E (1998) The Ray threaded fusion cage for posterior lumbar interbody fusion. Neurosurgery 42:200–204
Pihlajamaki H, Kinnunen J, Bostman O (1997) In vivo monitoring of the degradation process of bioresorbable polymeric implants using magnetic resonance imaging. Biomaterials 18:1311–1315
Pistner H, Gutwald R, Ordung R et al (1993) Poly(l-lactide): a long-term degradation study in vivo. I. Biological results. Biomaterials 14:671–677
Ray CD (1997) Threaded titanium cages for lumbar interbody fusions. Spine 22:667–679
Regan JJ, Yuan H, McAfee PC (1999) Laparoscopic fusion of the lumbar spine: minimally invasive spine surgery. A prospective multicenter study evaluating open and laparoscopic lumbar fusion. Spine 24:402–411
Rish BL (1989) A critique of posterior lumbar interbody fusion: 12 years’ experience with 250 patients. Surg Neurol 31:281–289
Rokkanen PU, Bostman O, Hirvensalo E et al (2000) Bioabsorbable fixation in orthopaedic surgery and traumatology. Biomaterials 21:2607–2613
Schwach G, Coudane J, Engel R et al (2002) Influence of polymerization conditions on the hydrolytic degradation of poly(dl-lactide) polymerized in the presence of stannous octoate or zinc-metal. Biomaterials 23:993–1002
Schwach G, Vert M (1999) In vitro and in vivo degradation of lactic acid-based interference screws used in cruciate ligament reconstruction. Int J Biol Macromol 25:283–291
Shah RR, Mohammed S, Saifuddin A et al (2003) Comparison of plain radiographs with CT scan to evaluate interbody fusion following the use of titanium interbody cages and transpedicular instrumentation. Eur Spine J 12:378–385
Smit TH, Muller R, Van Dijk M et al (2003) Changes in bone architecture during spinal fusion: three years follow-up and the role of cage stiffness. Spine 28:1802–1808
Togawa D, Bauer TW, Brantigan JW et al (2001) Bone graft incorporation in radiographically successful human intervertebral body fusion cages. Spine 26:2744–2750
Toth JM, Estes BT, Wang M et al (2002a) Evaluation of 70/30 poly (l-lactide-co-dl-lactide) for use as a resorbable interbody fusion cage. J Neurosurg 97:423–432
Toth JM, Wang M, Scifert JL et al (2002b) Evaluation of 70/30 D,L-PLa for use as a resorbable interbody fusion cage. Orthopedics 25:s1131–s1140
Tullberg T (1998) Failure of a carbon fiber implant. A case report. Spine 23:1804–1806
Tunc DC (1996) In vivo degradation and biocompatability study of in vitro pre-degraded as-polymerized polylactide particles. Biomaterials 17:2109–2112
van Dijk M, Smit TH, Burger EH et al (2002a) Bioabsorbable poly-l-lactic acid cages for lumbar interbody fusion: three-year follow-up radiographic, histologic, and histomorphometric analysis in goats. Spine 27:2706–2714
van Dijk M, Smit TH, Sugihara S et al (2002b) The effect of cage stiffness on the rate of lumbar interbody fusion: an in vivo model using poly(l-lactic Acid) and titanium cages. Spine 27:682–688
van Dijk M, Tunc DC, Smit TH et al (2002c) In vitro and in vivo degradation of bioabsorbable PLLA spinal fusion cages. J Biomed Mater Res 63:752–759
van Dijk M, van Diest PJ, Smit TH et al (2005) Four-year follow-up of poly-l-lactic acid cages for lumbar interbody fusion in goats. J Long Term Eff Med Implants 15:125–138
Viljanen J, Kinnunen J, Bondestam S et al (1995) Bone changes after experimental osteotomies fixed with absorbable self-reinforced poly-l-lactide screws or metallic screws studied by plain radiographs, quantitative computed tomography and magnetic resonance imaging. Biomaterials 16:1353–1358
Warden WH, Friedman R, Teresi LM et al (1999) Magnetic resonance imaging of bioabsorbale polylactic acid interference screws during the first 2 years after anterior cruciate ligament reconstruction. Arthroscopy 15:474–480
Weiler A, Helling HJ, Kirch U et al (1996) Foreign-body reaction and the course of osteolysis after polyglycolide implants for fracture fixation: experimental study in sheep. J Bone Joint Surg Br 78:369–376
Weiler A, Hoffmann RF, Stahelin AC et al (2000) Biodegradable implants in sports medicine: the biological base. Arthroscopy 16:305–321
Weiner BK, Fraser RD (1998) Spine update lumbar interbody cages. Spine 23:634–640
Wilke HJ, Kettler A, Claes LE (1997) Are sheep spines a valid biomechanical model for human spines? Spine 22:2365–2374
Wuisman PI, van Dijk M, Smit TH (2002) Resorbable cages for spinal fusion: an experimental goat model. J Neurosurg 97:433–439
Zdeblick TA, Phillips FM (2003) Interbody cage devices. Spine 28:S2–S7
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lazennec, J.Y., Madi, A., Rousseau, M.A. et al. Evaluation of the 96/4 PLDLLA polymer resorbable lumbar interbody cage in a long term animal model. Eur Spine J 15, 1545–1553 (2006). https://doi.org/10.1007/s00586-006-0145-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-006-0145-5