Abstract
Purpose
The aim of the study was to evaluate the feasibility of a bioabsorbable cage consisting of magnesium and magnesium phosphate cement (MPC) in a porcine lumbar interbody fusion model.
Methods
Twelve male Ba-Ma mini pigs underwent lumbar discectomy and fusion with an Mg−MPC cage or a PEEK cage at the L3/L4 and L4/L5 level. Computed tomography (CT) scans were made to evaluate the distractive property by comparing average disc space height (DSH) before and at 6, 12, and 24 weeks after the operation. After the lumbar spines were harvested at 6 or 24 weeks after the operation, micro-CT examination was conducted to analyze the fusion rate, and stiffness of motion segments was investigated through mechanical tests. A histological study was performed to evaluate the tissue type, inflammation, and osteolysis in the intervertebral space.
Results
CT scans showed no significant difference between the two groups in average DSH at each time point. Micro-CT scans revealed an equal fusion rate in both groups (0% at 6 weeks, 83.3% at 24 weeks). Both groups showed time-dependent increases in stability, the Mg−MPC cages achieved an inferior stiffness at 6 weeks and a comparable stiffness at 24 weeks. Histologic evaluation showed the presence of newly formed bone in both groups. However, empty spaces were observed at the interface or around the Mg−MPC cages.
Conclusion
Compared with the PEEK cages, the Mg−MPC cages achieved comparable distraction, fusion rate, and spinal stability at 24 weeks after the operation. However, due to inferior stiffness at the early stage and fast degradation, further modification of material composition and design are necessary.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Magnesium phosphate cement (MPC) is a novel biodegradable bone adhesive that could be used to directly conglutinate small fragments of non-loaded bone [1, 2]. However, no research on the use of MPC as an interbody fusion cage is available. Our unpublished results on MPC cages in a porcine lumbar spine interbody fusion model showed intervertebral fusion and conspicuous degradation of MPC at 6 months after implantation. The major drawback of the MPC cage for implantation is its high brittleness. In order to implant an MPC cage in the intervertebral space without cracking, the intervertebral space needs to be made broad enough to accommodate the cage, which is likely to cause damage to the vertebral endplate.
Magnesium is attractive for its degradation ability, elastic modulus similar to that of bone, stimulatory effect on bone growth, and good biocompatibility. Moreover, the fracture toughness of magnesium is greater than that of ceramic biomaterials such as hydroxyapatite [3].
The idea to combine MPC and magnesium in a hybrid cage (Mg−MPC cage) was conceived to ensure adequate initial toughness for operation and gradual degradation and osteoconduction for bone replacement.
This feasibility study was aimed at observing the fusion and degradation performance of the Mg−MPC cage, evaluating the histological and biomechanical properties in a porcine lumbar spine interbody fusion model.
Materials and methods
Materials
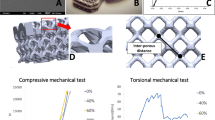
The MPC powder used in this study was composed of magnesium oxide (MgO), ammonium dihydrogen phosphate (NH4H2PO4), and sodium borate (Na2B4O7). The MgO and the NH4H2PO4 were in a molar ratio of 3.8:1. The MgO was prepared by heating basic magnesium carbonate pentahydrate [4MgCO3·Mg(OH)2·5H2O] in a furnace at 1500 °C for 6 h. After cooling and sieving process, the grains in the range of 200 and 300 meshes were kept for further experiment. Deionized water was employed as the cement liquid. The powder-to-liquid (P/L) ratio was 6.25 g/ml. The MPC powder was mixed with deionized water for 2 min to form paste, which was injected into a stainless-steel mold internally covered with magnesium bracket using a pressing device. The magnesium bracket was made of pure magnesium in the integrated molding process, and the purity of magnesium was more than 99%. The magnesium bracket was 20 mm long, 8 mm wide, 6 mm high, and 0.5 mm thick. After setting for 30 min, the Mg−MPC cages were dried at 60 °C for 24 h and sealed with a PE bag. The Mg−MPC cage was a block cage, which was 20 mm long, 8 mm wide, and 6 mm high (Fig. 1a). All the chemicals used for the Mg−MPC cages were purchased from Ningbo Hicren Biotechnology co., Ltd, China. The PEEK cage was a box cage, manufactured by Johnson & Johnson (Johnson & Johnson Medical Devices Companies, USA), which was 15 mm long, 12 mm wide, and 6 mm high, with a 3.5-mm radius central hole (Fig. 1b). The plants were sterilized by low-temperature plasma sterilization prior to the operation.
Animals and experimental design
All animal-related procedures were pre-approved by the Animal Ethnics Committee. Twelve male Ba-Ma mini pigs (weight 25–30 kg; average age 6 months) were used for this study with study time points of 6, 12, and 24 weeks after the operation. Each animal underwent extreme lateral interbody fusion (XLIF) with an Mg−MPC cage or a polyetheretherketone (PEEK) cage for control at the levels of L3/L4 and L4/L5. The two kinds of cages were inserted at the L3/L4 or L4/L5 level randomly. A 1-cm transverse process was cut off from the tip of L4 for the autologous bone grafts. PEEK cages were implanted with the central holes filled with autologous transverse process bone grafts. After implantation, titanium plates and screws were applied for fixation. The animals were sacrificed at 6 weeks (n = 6) and 24 weeks (n = 6) after the procedure. The spine specimens of interest were harvested and stored at − 20 °C for further tests.
Computed tomography
CT was performed using a CT scanner (GE, Optima CT 660, USA) before and at 6, 12, and 24 weeks after surgery. Axial cuts with 1-mm slice thickness were made parallel to the intervertebral disc space. At those time points, the anterior, middle, and posterior intervertebral disc space height (DSH) was measured from the middle sagittal view. The average DSH was calculated from anterior, middle, and posterior DSH measurements by the following formula: average DSH = (anterior DSH + middle DSH + posterior DSH)/3 (Fig. 2) [4].
Micro-computed tomography
The surgically treated motion segments were dissected and labeled. The microstructure of specimens was observed with micro-CT (PerkinElmer-Caliper LS, Quantum FX Demo, USA). The fusion rate was analyzed by observing the bony bridging of the discectomy space from the sagittal view of the specimen.
Mechanical tests
Mechanical properties were tested as described previously by Panjabi et al. [5]. The specimens at 6 weeks (n = 6) and 24 weeks (n = 6) after the operation underwent mechanical tests. Three fresh mini pig cadaveric lumbar spines (6 motion segments) were used as control. The specimens were thawed in a 4 °C refrigerator and covered with a polyethylene warp to prevent dehydration. Each motion segment to be tested consisted of a cranial and a caudal lumbar vertebra. The fixation devices were removed. The facet joints and posterior elements of the motion segment were removed prior to testing. The cranial and caudal vertebra were potted in polymethylmethacrylate and fixed on a universal testing machine (Instron, 55MT, USA). Specimens were tested for flexion/extension, right/left lateral bending, and right/left axial rotation sequentially at a constant loading rate (1.0 degree/s) and a maximum torque of 5 Nm. The stiffness was calculated as moment (Nm)/rotation angle (degree). Five consecutive readings were recorded and the last record was used for statistical analysis.
Histology
After the mechanical tests, the specimens were dehydrated in graded ethanol and embedded in plastic films. The specimens were cut into longitudinal sections by precision saw (Leica, SP1600, Germany) and ground into parallel sections of 40-µm thickness. Tissue sections were stained with Giemsa staining and Masson trichrome staining and then observed by light microscope. The intervertebral space was analyzed using a slightly modified protocol from Zdeblick et al. [6]. Briefly, the tissue type at the implant–vertebra interface or around the implant was rated as empty/fibrous tissue/bone; inflammation and osteolysis were rated as yes/no [7, 8]. Histologic evidence of inflammation was defined as the presence of neutrophilic, giant, or mononuclear cells in the tissue adjacent to implants.
Statistical methods
Measurement data are expressed as mean ± standard deviation. Enumeration data are expressed as number of cases. Statistical analysis was performed using SPSS 19.0 for windows (SPSS Inc., USA). The Student’s t-test, one-way ANOVA, Scheffe’s test, and chi-square test were used to compare the values among groups. P < 0.05 was considered as statistically significant.
Results
Computed tomography
The preoperative average DSH did not show a significant difference between the two groups (P > 0.05). Moreover, there were no significant differences in average DSH between the two groups at 6, 12, and 24 weeks after the operation (P > 0.05; Figs. 3 and 4). No gas accumulation was observed at 6, 12, and 24 weeks after the operation.
Micro-computed tomography
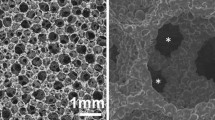
At 6 weeks, both the Mg−MPC cage and the PEEK cage attached to the endplate and newly formed bone tissue was observed to infiltrate into the interface. Cracks and cavities formed on the surface of the Mg−MPC cage, indicating degradation of the Mg−MPC. Both the two groups remained unbridged (Fig. 5).
At 24 weeks, scanning images from the sagittal view revealed the use of an Mg−MPC cage or a PEEK cage led to an equal spinal fusion rate: the fusion rate is 83.3% in both cases (P > 0.05; Table 1). Newly formed bone tissue traversed the Mg−MPC cage to bridge the discectomy space, with the Mg−MPC cage degrading simultaneously (Fig. 6). Due to a fixing system failure, cage rotation and movement were observed in one specimen of the Mg−MPC group and of the PEEK group, respectively, which led to spinal fusion failure.
Mechanical tests
At 6 weeks, both the Mg−MPC group and the PEEK group showed a higher stiffness in all loading directions (flexion and extension, right and left lateral bending, and right and left axial rotation) compared to the negative control (normal lumbar segments) (P < 0.05). Compared with the Mg−MPC group, the stiffness of the PEEK group in flexion and extension and in the lateral bending direction is higher (P < 0.05), indicating that a better spinal stability was achieved in the PEEK group.
At 24 weeks, both the Mg−MPC group and the PEEK group showed a further increase in stiffness compared to the negative control (P < 0.05). Meanwhile, the Mg−MPC group and the PEEK group achieved comparable spinal stability performance in all loading directions (P > 0.05; Figs. 7, 8 and 9).
Histology
Large defects were observed in histological sections of the Mg−MPC cages, which were formed during sectioning due to brittleness.
In the Mg−MPC group, bone tissue started to protrude into the implant–vertebra interface at 6 weeks after the operation. At 24 weeks after the operation the bone growth progressed both in the interface and around the implant. Despite the new bone formation, empty spaces could be observed in the interface or around the Mg−MPC cages due to fast degradation of the implant.
In the PEEK group, at 6 weeks after the operation new bone seemed to be absent and the implants were firmly bonded to the endplates by fibrous tissue. At 24 weeks after the operation, new bone accompanied by fibrous tissue had formed both at the interface and around the implants. The fibrous tissue was observed in large number of tissue sections. (Figures 10 and 11).
The presence of inflammatory cells or a granulomatous response and osteolysis were not evident in either group at any time point.
Discussion
The ideal bioabsorbable materials for cage devices should possess three properties: the capability of degradation during a distinct period, the property not to obscure postoperative radiological estimation of intervertebral fusion, and the stiffness comparable with that of bone. During the degradation process, loading is transferred gradually to the newly formed bone and the cage is replaced with bone. Several previous studies involved animal experiments or clinical trials with bioabsorbable cages [9,10,11,12,13,14,15,16]. Most of these bioabsorbable cages were composed of polylactic acid [9,10,11, 15], which naturally degrades to carbon dioxide and water. Other bioabsorbable substances are polymer–calcium phosphate composites, composites of polyglycolic acid, multiamino acid copolymer/nanohydroxyapatite/calcium sulfate, and multiamino acid copolymer/α-tricalcium phosphate [17,18,19]. Although most of these studies demonstrated successful fusion with these cages, some adverse events were reported. Kandziora et al. [4] showed that poly-L-lactide-co-D, L-lactide (PLDLLA) cages were associated with osteolysis in a sheep model at 12 weeks after the operation. They found a severe foreign body reaction causing osteolysis around the PLDLLA cage. The osteolysis caused skepticism about the value of PLDLLA as an implant.
MPC has attracted much attention as a potential biodegradable bone implant material. The main components of MPC are magnesium oxide (MgO) and acid ammonium phosphates, particularly ammonium dihydrogen phosphate (NH4H2PO4). MPC powders react in the presence of water to form HN4MgPO4·6H2O (struvite) as the final product [2]. Yu et al. [20] assessed the toxicology and biocompatibility of MPC through the UDS test, Ames test, and micronuclei test and also evaluated degradation and osteogenesis in a rabbit femur condyle defect model. The results showed MPC was safe since it did not induce DNA damage or gene mutations. As regards the implantation test, the MPC implant formed direct bonds with the host bone and exhibited good degradation at 6 months after surgery. Our previous studies on a pure MPC cage also showed intervertebral fusion and conspicuous degradation of MPC at 6 months after implantation in a porcine lumbar spine interbody fusion model. However, the major drawback of the pure MPC cage as an implant is its high brittleness, prompting further modification to increase the toughness.
Magnesium is the fourth most abundant cation in the human body, with approximately half of the total physiological magnesium stored in bone tissue [3]. The elastic modulus and compressive yield strength of magnesium are closer to those of natural bone, while the fracture toughness of magnesium is greater than that of ceramic biomaterials such as hydroxyapatite [3]. In addition, magnesium exerts stimulatory effects on the growth of new bone tissue [21, 22]. The major drawback of magnesium as an implant is the quick corrosion in the high chloride environment at physiological pH (7.4–7.6), losing mechanical integrity before the tissue has sufficiently healed. Moreover, magnesium produces hydrogen gas in the corrosion process that is not likely to be dealt with by the host tissue immediately [21]. Daentzer et al. [23] investigated a bioabsorbable cage consisting of magnesium and polymer (poly-ε-caprolactone, PCL) in an ovine cervical model. The postoperative lateral radiographs showed gas accumulation in front of the disc space in 50% of the sheep. The gas completely disappeared within the next 3 weeks. In this study, no gas accumulation was observed at 6, 12, and 24 weeks after the operation, because the amount of magnesium in the hybrid cage was small, so hydrogen gas could easily be dealt with by the host tissue.
To our knowledge, this study is the first attempt to use MPC and magnesium as an interbody fusion cage to assist intervertebral fusion in vivo. The magnesium was employed to compensate for the lack of toughness in the MPC cage. Compared to a pure MPC cage, the hybrid Mg−MPC cage could be easily placed into the intervertebral space without fragmentation during the operation.
Cages should retain interbody distraction and resist against subsidence into the adjacent vertebra to guarantee bony fusion of a desired quality. The distractive properties of cages have been investigated in some experiments. Kandziora et al. [4] showed that a PLDLLA cage and autologous tricortical iliac crest bone graft developed a remarkable loss of DSH during an observation period of 12 weeks in a sheep cervical spine fusion model due to degradation of the implant and gradual graft collapse, respectively. Jiya et al. [16] assessed clinical and radiologic outcomes of the PLDLLA cage compared with the PEEK cage, demonstrating the PEEK cage group had a lower subsidence rate. Our study demonstrated both PEEK cages and Mg–MPC cages were able to distract intervertebral disc spaces beyond their baseline measure at 6 weeks after the operation. However, the average DSH decreased significantly in both groups at 12 and 24 weeks after the operation. Too rigorous preparation of the endplates might leave a mechanically weaker spongious bone bed to cages, thus promoting subsidence in both groups. Moreover, the decrease in DSH in the Mg–MPC group resulted partly from degradation.
Assessment of fusion was frequently based on radiographs or histology. Toth et al. [24] introduced a fusion scoring system by using high resolution radiographs. Zdeblick et al. [6] devised a grading scale to analyze the histologic fusion results. The two methods have been widely applied to analyze fusion rates in animal experiments [4, 19]. In this study, micro-CT was applied to estimate the fusion rate. Micro-CT could estimate the bony growth, the trabecular structure of newly formed bone, the degradation of implants, and even osteolysis. At 24 weeks after the operation, the newly formed bone tissue was observed to bridge the discectomy space through cracks in the Mg–MPC group, while the Mg–MPC cages degraded increasingly.
Compared to Mg–MPC cages, the PEEK cages showed higher stiffness in the flexion, extension, and lateral bending directions at 6 weeks after the operation. In addition to the large amount of fibrous tissue that is likely to increase the spinal stiffness, the autograft bone in the central hole of the PEEK cages may lead to quicker bone growth, improving the stability at the early stages. Other studies also revealed using bone graft was likely to affect the interbody fusion [25]. Li et al. [19] observed that titanium cages packed with autologous iliac crest bone grafts in the central hole could achieve quicker fusion than polycaprolactone-tricalcium phosphate (PCL-TCP) cages without a central hole. With the knowledge gained from these results, further research is recommended to investigate if adding a central hole in the Mg–MPC cage, which could be filled with bone grafts, can help achieve quicker fusion as well as better stability.
The histological study revealed that both the Mg–MPC cage and the PEEK cage did not behave well in terms of osseointegration, that is, empty spaces were observed at the implant–vertebra interface or around the implant due to relatively rapid degradation of the Mg–MPC cage, while the PEEK cages were surrounded by large amounts of fibrous tissue which may be a result of a foreign body reaction. The rapid degradation seems to be another possible cause of the insufficient stability at the early stage in the Mg–MPC group. The degradation rate of the bioabsorbable implants is related to the material composition, the structure, and the degradation environment [26]. Therefore, the degradation of the Mg−MPC cage could be improved by modification of the material composition or the structure of the implant.
The limitations of this study include the limited numbers of animals enrolled in each group and the time points chosen for evaluation. The follow-up period does not allow for a description of the performance of Mg–MPC cages in the long term. In addition, due to different designs of the two kinds of cages, whether the bone grafts were used, and the degradation of the Mg–MPC cages, we couldn’t take an appropriate approach to make a quantitative analysis of the tissue type, particularly the newly formed bone tissue between the two groups. Moreover, in order to create enough space to accommodate the cages, the endplates were prepared too large in the two groups, which could induce interference in the evaluation of the distractive properties of the two kinds of cages.
Conclusion
In this feasibility study, we demonstrated that in contrast to PEEK cages, the Mg−MPC cages achieved comparable distraction, fusion rate, and spinal stability at 24 weeks after the operation. However, due to the inferior stiffness at the early stage and fast degradation, further modification of material composition and design are necessary. Moreover, the drawbacks mentioned above in this study should be improved.
References
Waselau M, Samii VF, Weisbrode SE, Litsky AS, Bertone AL (2007) Effects of a magnesium adhesive cement on bone stability and healing following a metatarsal osteotomy in horses. Am J Vet Res 68 (4):370–378. https://doi.org/10.2460/ajvr.68.4.370
Wu F, Wei J, Guo H, Chen F, Hong H, Liu C (2008) Self-setting bioactive calcium-magnesium phosphate cement with high strength and degradability for bone regeneration. Acta Biomater 4 (6):1873–1884. https://doi.org/10.1016/j.actbio.2008.06.020
Staiger MP, Pietak AM, Huadmai J, Dias G (2006) Magnesium and its alloys as orthopedic biomaterials: a review. Biomaterials 27 (9):1728–1734. https://doi.org/10.1016/j.biomaterials.2005.10.003
Kandziora F, Pflugmacher R, Scholz M, Eindorf T, Schnake KJ, Haas NP (2004) Bioabsorbable interbody cages in a sheep cervical spine fusion model. Spine (Phila Pa 1976) 29 (17):1845–1855; discussion 1856
Panjabi MM (1988) Biomechanical evaluation of spinal fixation devices: I. A conceptual framework. Spine (Phila Pa 1976) 13 (10):1129–1134
Zdeblick TA, Ghanayem AJ, Rapoff AJ, Swain C, Bassett T, Cooke ME, Markel M (1998) Cervical interbody fusion cages. An animal model with and without bone morphogenetic protein. Spine (Phila Pa 1976) 23 (7):758–765; discussion 766
Anderson JM, Rodriguez A, Chang DT (2008) Foreign body reaction to biomaterials. Semin Immunol 20 (2):86–100. https://doi.org/10.1016/j.smim.2007.11.004
Trindade R, Albrektsson T, Tengvall P, Wennerberg A (2016) Foreign Body Reaction to Biomaterials: On Mechanisms for Buildup and Breakdown of Osseointegration. Clin Implant Dent Relat Res 18 (1):192–203. https://doi.org/10.1111/cid.12274
van Dijk M, Smit TH, Burger EH, Wuisman PI (2002) Bioabsorbable poly-L-lactic acid cages for lumbar interbody fusion: three-year follow-up radiographic, histologic, and histomorphometric analysis in goats. Spine (Phila Pa 1976) 27 (23):2706–2714. https://doi.org/10.1097/01.brs.0000035300.81730.33
Lanman TH, Hopkins TJ (2004) Early findings in a pilot study of anterior cervical interbody fusion in which recombinant human bone morphogenetic protein-2 was used with poly(L-lactide-co-D,L-lactide) bioabsorbable implants. Neurosurg Focus 16(3):E6
Frost A, Bagouri E, Brown M, Jasani V (2012) Osteolysis following resorbable poly-L-lactide-co-D, L-lactide PLIF cage use: a review of cases. Eur Spine J 21 (3):449–454. https://doi.org/10.1007/s00586-011-2002-4
Tunc DC, van Dijk M, Smit T, Higham P, Burger E, Wuisman P (2004) Three-year follow-up of bioabsorbable PLLA cages for lumbar interbody fusion: in vitro and in vivo degradation. Adv Exp Med Biol 553:243–255
van Dijk M, Tunc DC, Smit TH, Higham P, Burger EH, Wuisman PI (2002) In vitro and in vivo degradation of bioabsorbable PLLA spinal fusion cages. J Biomed Mater Res 63 (6):752–759. https://doi.org/10.1002/jbm.10466
Daentzer D, Willbold E, Kalla K, Bartsch I, Masalha W, Hallbaum M, Hurschler C, Kauth T, Kaltbeitzel D, Hopmann C, Welke B (2014) Bioabsorbable interbody magnesium-polymer cage: degradation kinetics, biomechanical stiffness, and histological findings from an ovine cervical spine fusion model. Spine (Phila Pa 1976) 39 (20):E1220-1227. https://doi.org/10.1097/BRS.0000000000000507
Pflugmacher R, Eindorf T, Scholz M, Gumnior S, Krall C, Schleicher P, Haas NP, Kandziora F (2004) [Biodegradable cage. Osteointegration in spondylodesis of the sheep cervical spine]. Chirurg 75 (10):1003–1012. https://doi.org/10.1007/s00104-004-0884-y
Jiya T, Smit T, Deddens J, Mullender M (2009) Posterior lumbar interbody fusion using nonresorbable poly-ether-ether-ketone versus resorbable poly-L-lactide-co-D,L-lactide fusion devices: a prospective, randomized study to assess fusion and clinical outcome. Spine (Phila Pa 1976) 34 (3):233–237. https://doi.org/10.1097/BRS.0b013e318194ed00
Chunguang Z, Yueming S, Chongqi T, Hong D, Fuxing P, Yonggang Y, Hong L (2011) Evaluation of bioabsorbable multiamino acid copolymer/alpha-tri-calcium phosphate interbody fusion cages in a goat model. Spine (Phila Pa 1976) 36 (25):E1615-1622. https://doi.org/10.1097/BRS.0b013e318210ca32
Ren C, Song Y, Xue Y, Yang X, Zhou C (2017) Evaluation of Bioabsorbable Multiamino Acid Copolymer/Nanohydroxyapatite/Calcium Sulfate Cage in a Goat Spine Model. World Neurosurg 103:341–347. https://doi.org/10.1016/j.wneu.2017.04.005
Li Y, Wu ZG, Li XK, Guo Z, Wu SH, Zhang YQ, Shi L, Teoh SH, Liu YC, Zhang ZY (2014) A polycaprolactone-tricalcium phosphate composite scaffold as an autograft-free spinal fusion cage in a sheep model. Biomaterials 35 (22):5647–5659. https://doi.org/10.1016/j.biomaterials.2014.03.075
Yu Y, Wang J, Liu C, Zhang B, Chen H, Guo H, Zhong G, Qu W, Jiang S, Huang H (2010) Evaluation of inherent toxicology and biocompatibility of magnesium phosphate bone cement. Colloids Surf B Biointerfaces 76 (2):496–504. https://doi.org/10.1016/j.colsurfb.2009.12.010
Witte F, Kaese V, Haferkamp H, Switzer E, Meyer-Lindenberg A, Wirth CJ, Windhagen H (2005) In vivo corrosion of four magnesium alloys and the associated bone response. Biomaterials 26 (17):3557–3563. https://doi.org/10.1016/j.biomaterials.2004.09.049
Zreiqat H, Howlett CR, Zannettino A, Evans P, Schulze-Tanzil G, Knabe C, Shakibaei M (2002) Mechanisms of magnesium-stimulated adhesion of osteoblastic cells to commonly used orthopaedic implants. J Biomed Mater Res 62 (2):175–184. https://doi.org/10.1002/jbm.10270
Daentzer D, Floerkemeier T, Bartsch I, Masalha W, Welke B, Hurschler C, Kauth T, Kaltbeitzel D, Hopmann C, Kujat B, Kalla K (2013) Preliminary results in anterior cervical discectomy and fusion with an experimental bioabsorbable cage - clinical and radiological findings in an ovine animal model. Springerplus 2:418. https://doi.org/10.1186/2193-1801-2-418
Toth JM, Wang M, Scifert JL, Cornwall GB, Estes BT, Seim HB, 3rd, Turner AS (2002) Evaluation of 70/30 D,L-PLa for use as a resorbable interbody fusion cage. Orthopedics 25 (10 Suppl):s1131-1140
Steffen T, Tsantrizos A, Fruth I, Aebi M (2000) Cages: designs and concepts. Eur Spine J 9 Suppl 1:S89-94
Wei J, Jia J, Wu F, Wei S, Zhou H, Zhang H, Shin JW, Liu C (2010) Hierarchically microporous/macroporous scaffold of magnesium-calcium phosphate for bone tissue regeneration. Biomaterials 31 (6):1260–1269. https://doi.org/10.1016/j.biomaterials.2009.11.005
Acknowledgements
This work was supported by the National Natural Science Foundation of China (No. 51372276, No. 51772328, and No. 81702121), the Scientific Research Project of Capital Health Development (2018-4-5014), the Clinical Research Support Fund of Chinese PLA General Hospital (2017FC-TSYS-2006) and the Major Project of Military Logistics (AWS17J004).
Funding
The National Natural Science Foundation of China (No. 51372276, No. 51772328, and No. 81702121), the Scientific Research Project of Capital Health Development (2018-4-5014), the Clinical Research Support Fund of Chinese PLA General Hospital (2017FC-TSYS-2006), and the Major Project of Military Logistics (AWS17J004) were received to support this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and animal rights
All applicable international, national, and institutional guidelines for the care and use of animals were followed. All procedures performed in studies involving animals were in accordance with the ethical standards of the institution at which the studies were conducted.
Conflict of interest
All authors declare that they have no potential conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, X., Zhang, Y., Wang, Y. et al. Biological performance of a bioabsorbable magnesium–magnesium phosphate cement interbody fusion cage in a porcine lumbar interbody fusion model: a feasibility study. Eur Spine J (2024). https://doi.org/10.1007/s00586-024-08387-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00586-024-08387-3