Abstract
The study design was to decrease the damage of spinal cord on the experimentally induced acute spinal cord injury in rats. The objective of this study was to evaluate whether recombinant human erythropoietin (rHu-EPO) and methylprednisolone (MPSS) improve neurological function and histopathological changes if systemically administered after traumatic spinal cord injury. This study included 48 rats that underwent experimental SCI. Forty-eight animals were randomly divided into six groups. Animals constituted a moderate compression of 0.6 N that was produced by application of an aneurysm clip at level T3 for 1 min. rHu-EPO (1,000 and 3,000 U (Unit) per kg of body weight i.p.) and MPSS (30 mg/kg) were administered 5 min after injury, and control group was saline treated. (1) Control group (n=8), (2) MPSS group (n=8), (3) rHu-EPO 1,000 U group (n=8), (4) MPSS + rHu-EPO 1,000 U group (n=8), (5) rHu-EPO 3,000 U group (n=8), and (6) MPSS + rHu-EPO 3,000 U group (n=8). The neurological function and histopathology were evaluated at 24 and 72 h. According to the neurological functional test scores significant improvements between the control group and the other groups that had taken medical treatment were observed (P<0.001). Histopathologically severe ischemic findings were observed in the control group. A significant decrease in ischemic damage was detected in MPSS + rHu-EPO 3,000 U group (P<0.001). The most significant neurological functional and histopathological improvements were observed after systemical administration of MPSS + rHu-EPO 3,000 U and rHu-EPO 3,000 U. Furthermore, the MPSS + rHu-EPO 3,000 U group provides the most improved neurological functional and histopathological recovery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Traumatic spinal cord injury (TSCI) occurs frequently and is devastating for the individual patient and costly to the society by requiring substantial long-term health care expenditures. Currently, methylprednisolone (MPSS) administered at high dose within 8 h after injury is the only therapy with some recognized benefit [2, 11], unfortunately, is relatively minor. Any new treatment of TSCI that allows for major recovery of function would be a significant advance in clinical care [11].
It is known that applying MPSS after spinal injury decreases spin lipid peroxidation, stabilizes intracellular and extracellular Ca+2 current, decreases neurofilament degeneration, increases the spinal blood current, decreases Na+ and water containing in lesion, and prevent K+ loss [25].
Erythropoietin (EPO) has recently been shown to play roles in the nervous system in both normal and pathological conditions [4]. EPO and its receptor are expressed in the central and peripheral nervous system, and the expression of both proteins is modulated by hypoxia [1, 4, 6, 17].
Injury of the nervous system provokes a complex cascade of proinflammatory cytokines and other molecules that ultimately result in apoptosis and necrosis of neurons, oligodendrocytes, and endothelial cells [9, 20]. Recent studies have demonstrated that one general response of the brain to injury is the increased local production of the EPO and its receptor [1, 21]. These proteins are members of the cytokine type I superfamily that provide beneficial effects including inhibition of apoptosis, reduction of inflammation, modulation of excitability [3, 17–19], and mobilization and proliferation of neuronal stem cells.
In this pilot study, the degree of improvement was assessed by making histopathological evaluation together with neurological functional test in the rats that were subjected to acute spinal cord injury (SCI), and treated with MPSS and rHu-EPO systemically.
Materials and methods
Animals
Forty-eight Sprague–Dawley rats weighing 200–300 g were used in this study. Animals were housed under standard conditions (22±2°C) in the Animal Research Laboratory of Dicle University (DUSAM). The study protocol was approved by the Animal Research Committee of Dicle University/Turkey. Animals were maintained in a 12-h light/dark cycle with tap water and food freely available [12].
Experimental design
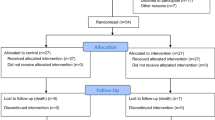
Experimental studies were designed to evaluate acute beneficial effects on behavioral (motor) assessments and histopathological related to the systemic administration of rHu-EPO + MPSS in setting of TSCI. The forty-eight animals were randomly divided into six groups.
-
1.
Control group (n=8): Sham operated group. The cord was clamped for 1-min duration, and single dose saline solution with infusion [0.5 ml/kg/h of intraperitoneal (i.p.)] was given for 15 min, 5 min after injury.
-
2.
MPSS group (n=8): The cord was clamped for 1-min duration, and 30 mg/kg of MPSS with i.p. infusion was given for 30 min, 5 min after injury. After waiting for 15 min, 5.4 mg/kg/h of MPSS was given in 8 h with i.p. infusion.
-
3.
rHu-EPO 1,000 U (Unit) group (n=8): The cord was clamped for 1-min duration, and single dose of rHu-EPO (1,000 U/kg, i.p.) was given 5 min after injury.
-
4.
MPSS + rHu-EPO 1,000 U group (n=8): The cord was clamped for 1-min duration, 5 min after injury, 30 mg/kg of MPSS with i.p. infusion was given for 30 min as bolus. After waiting for 15 min, 5.4 mg/kg/h of MPSS with i.p. infusion was given for 8 h. Forty minutes after injury, rHu-EPO (1,000 U/kg i.p.) was given once as a bolus.
-
5.
rHu-EPO 3,000 U group (n=8): The cord was clamped for 1-min duration, and rHu-EPO (1,000 U/kg) was given 5 min after injury three successive daily single doses as bolus.
-
6.
MPSS + rHu-EPO 3,000 U group (n=8): The cord was clamped for 1-min duration, and 30 mg/kg of MPSS with i.p. infusion was given for 30 min, 5 min after injury. After waiting for 15 min, 5.4 mg/kg/h of MPSS with i.p. infusion was given for 8 h, and three successive daily single doses of 1,000 U/kg/day of rHu-EPO was given 40 min after injury.
Surgical procedures
Preoperatively imipenem (10 mg/kg of bw) was administered intramuscularly for prophylaxis of infection. The animals were fasted for 12 h before surgery, humanely restrained, and anesthetized with i.p. injection of thiopental sodium [40 mg/kg of body weight (bw)]. Temperatures were maintained throughout the operative procedure by exposing the animal to a heat lamp as needed until they completely recovered from anesthesia. The animals were positioned in the prone position and surgery was performed under sterile conditions. After infiltration of the skin (bupivacaine 0.25%), a complete single level (T3) laminectomy was performed through a 2-cm incision with the aid of a dissecting microscope. Compressive injury was produced by transient extradural application of an aneurysm clip model that produces a moderately severe injury with a distinct vascular component and relatively little hemorrhages [7, 11]. Injuries were induced by the extradural application of a temporary aneurysm clip exerting a 0.6-N closing force on the spinal cord for 1 min. After removal of the clip, the skin incision was closed and the animals were allowed to recover fully from anesthesia and returned to their cages [11].
Neurological evaluation
Neurological function was evaluated 24 and 72 h after injury, according to the criteria of Swimming test [11]. In this assessment, a rat was placed in the center of a round tube of water (40-cm diameter) filled to a depth of 30 cm with a wire mesh ladder attached to the side. The animal was rated 0 when neither hind limb was used for swimming and climbing out, 1 when there was a partial use of the hind limbs, and 2 when both hind limbs were used normally [11].
Histopathological evaluation
After the neuromotor functions of the animals have been assessed by means of swimming test, 24 and 72 h after reperfusion, the animals were killed using thiopental (120 mg/kg, i.p.), and the spinal cords were removed and immediately fixed in 10% formaldehyde. After fixation, transverse sections of spinal cord at the T3 level were embedded in paraffin, cut into 5 μm thick sections, and stained with hematoxylin and eosin. Ischemic lesions were evaluated in a blinded manner by using light microscopy (Olympus BH2). The numbers of ischemic neurons with histological characteristics of abnormal structures [intrastoplasmic vacuolization, shrinkage and hyperdensity of the nuclei (pyknosis), perineuronal large halo, eosinophilic or dark, shrunken cytoplasm with indistinct neuronal processes] were counted in each section [12]. The result of neuronal injury in five randomly selected sections from each animal was evaluated. Sections were evaluated according to the presence and relative abundance of ischemic neurons in ventral gray matter area into three groups: mild injury (5% of motor neurons ischemic), moderate injury (5–20% neuronal ischemic), and severe injury (20% of neurons affected) [4].
Statistics
The statistical analyses were carried out with the SPSS (statistical package for social sciences). Differences in proportions for categorical variables were tested by Kruskal–Wallis one-way ANOVA by ranks for multiple groups. P<0.05 was accepted as significant for statistical comparison. Bonferroni corrected Mann–Whitney U test was used for the comparison between groups as pairs.
Results
Animals receiving saline injections 5 min immediately after aneurysm clip removal suffered a flaccid paraplegia for the first 1 and 3 days after injury. In contradiction, animals receiving either a single dose of rHu-EPO (1,000 U/kg of bw) or MPSS (30 mg/kg) followed by a superior clinical course despite an equivalent clinical score 5 min after clip removal, and the other rHu-EPO received daily injections of 1,000 U/kg of bw for 3 consecutive days.
MPSS + rHu-EPO 1,000 U and 3,000 U treated animals exhibited improvements of motor function by 24 and 72 h (corresponding to movement at all three joints of the hind limb, P<0.001 vs. control). By comparision the control group and the groups received medical treatment were assessed according to the neurological function test scores, statistically significant improvements were observed (P<0.001). When the rHu-EPO 3,000 U group and MPSS + rHu-EPO 3,000 U group compared with control group, the most significant improvement was observed at MPSS + rHu-EPO 3,000 U group (P<0.001) (Table 1).
Histopathologically, various degrees of ischemic neurons were found in all the groups. The control group animals were characterized by a high frequency of necrotic neurons. Nearly all the neurons in this group were ischemic (Fig. 1). Degree of ischemic neurons from MPSS + rHu-EPO 3,000 U group demonstrated a significant decrease when compared with the other groups. When the rHu-EPO 3,000 U group and MPSS + rHu-EPO 3,000 U group were compared with the control group, there was a significant decrease in the ischemic damage (P<0.001). Histopathologically the most significant improvement was observed in MPSS + rHu-EPO 3,000 U group (P<0.001). Sections obtained from MPSS + rHu-EPO 3,000 U group treated animals appeared very different often having mild histological evidence of injury (Figs. 2, 3). Table 2 summarizes the differences in ischemic neurons in all the groups.
Discussion
Recombinant human EPO has been widely used in clinical practice such as anemia associated with renal failure, cancer, and surgery. Recent studies have shown the importance of the neuroprotective effects of EPO [7, 11, 24].
Erythropoietin has not been studied extensively in traumatic or ischemic SCI. EPO has anti-inflammatory and antiapoptotic functions and enables early recovery of function, and prevents motor neuron apoptosis and neurological disability in experimental ischemic SCI [4, 11].
One of the other possible mechanisms of EPO’s neuroprotective effect after TSCI may be the inhibition of excitatory amino acid release. Kawakami et al. proposed that EPO receptor (EPO-R)-mediated inhibition of glutamate release is responsible for the neuroprotective effect in cerebral ischemia [13, 14]. Bernaudin et al. proposed that the EPO/EPO-R system might be implicated in neuroprotective and restructuring processes (such as angiogenesis and gliosis) after ischemia [1, 13]. Thus, it is possible that EPO modulates angiogenesis also in traumatized spinal cord, leading to increased blood flow and tissue oxygenation and thus counteracting expansion of the damaged core of injury [14].
The results of these experiments demonstrate a major neurological benefit associated with the systemic administration of MPSS + rHu-EPO 3,000 U after TSCI produced by transient compression. After the trauma MPSS + rHu-EPO 3,000 U were associated with a markedly superior clinical course of recovery of motor function compared with sham group, characterized by an earlier and more complete normalization of function over a 3-day period of study. Further, injury produced by the aneurysm clip improved significantly within 24 and 72 h after injury, a time at which saline-treated animals remained completely paralyzed. Data obtained from conclusion suggests that much of beneficial effect of MPSS + rHu-EPO 3,000 U treatment occurs within 3 days after injury, as characterized by an earlier recovery of motor function after injury. Thereafter, neurological recovery occurred at the same rate in both saline and rHu-EPO treated animals, despite the dramatic differences observed at the histological level after 3 days.
To date, the only pharmacotherapeutic with demonstrated effectiveness in TSCI is MPSS. This agent must be given within the first 8 h after SCI. However, the beneficial effect is frequently only moderate even in animal models [5]. Ducker et al. [8] have observed better motor improvement in dogs treated with dexamethasone.
The very early recovery observed in the aneurysm clip model could depend on a beneficial effect of rHu-EPO on the restoration of adequate blood flow after injury. After experimental TSCI, a profound reduction in spinal cord blood flow occurs, which progressively worsens [10] and may last for 24 h [16]. In a recent study assessing the effects of EPO on the clinical course after subarachnoid hemorrhage in a rabbit model, rHu-EPO treatment dramatically attenuated the intense intracerebral arterial spasm secondary to the irritative effects of blood infused into the subarachnoid space [12]. Further, a single dose of rHu-EPO given peripherally has been shown to preserve autoregulation of cerebral blood flow [22]. Thus, rHu-EPO both actively reduces the cerebral ischemia after hemorrhage by maintaining tissue perfusion, and directly provides neuroprotection for metabolically stressed neurons. The mechanism of this vascular effect has not been directly evaluated, but the potent vascular effects of rHu-EPO noted within the systemic circulation appear to depend on the modulation of inducible nitric oxide syntheses activity [23]. In addition to the constrictive effects of compression on circulation within the spinal cord, injury-related neurological dysfunction itself typically produces severe hypotension and bradycardia in both humans [20] and animals [15], further worsening the effects of neuronal ischemia.
In this study, we applied 1,000 and 3,000 U of rHu-EPO and MPSS intraperitoneal after causing ischemia by applying aneurysm clip for about 1 min to the spinal cord. In reperfusion of the spinal cord that was subjected to ischemia and in treating the later damage, the application of 3 days uninterrupted one dosage (bolus i.p. injection) of rHu-EPO 1,000 and 3,000 U improves the neuromotor functions significantly. The intraperitoneal applications of 1,000 and 3,000 U of rHu-EPO decrease the ischemic damage histopathologically with respect to the control group. When the MPSS + rHu-EPO 3,000 U were compared with the control group, neurologically and histopathologically striking improvements have been observed. Celik et al. have found that different doses of EPO (350, 800, 1,000 U/kg) have improved the motor neural functions and histopathology of rats against the neural damage after ischemic spinal injury in a similar study [4]. The results obtained from our study are found to be similar to that study. However, being different from that work, we have observed that rHu-EPO 3,000 U dosage gives also an improvement on neural functions and histopathology. Gorio et al. have also found that application of 5,000 U of EPO gives improvements on neural functions and pathology in a similar work [11].
In our study, the results of rHu-EPO 1,000 and 3,000 U/kg/day were statistically significant compared to the control group. This result gives parallelism with rHu-EPO, neuromotor function test results with the work of Gorio et al. [11].
In the present study, the differences between the control group, MPSS, MPSS + rHu-EPO (1,000 U/kg), and rHu-EPO (3,000 U/kg) groups were significant, and as a result of neuromotor function test and histopathological data, it has been found that the MPSS + rHu-EPO (3,000 U/kg) was the most effective group. This result can be useful for using new pharmacological agents after experimental spinal injury and give rise to the new research.
As a result, we confirmed the efficiency of rHu-EPO in medical treatment of experimental SCI. We believe that these results will be discussed in further works and rHu-EPO may be used in the treatment of SCI treatment routinely.
References
Bernaudin M, Marti HH, Roussel S, Divoux A, MacKenzie ET, Petit E (1999) A potential role for erythropoietin in focal permanent cerebral ischemia in mice. J Cereb Blood Flow Metab 19:643–651
Bracken MB (2001) Methylprednisolone and acute spinal cord injury: an update of the randomized evidence. Spine 26:S47–S54
Brines ML, Ghezzi P, Keenam S, Agnello D, de Lancrolle NC, Cerami C, Itri LM, Cerami A (2000) Erythropoietin crosses the blood–brain barrier to protect against experimental brain injury. Proc Natl Acad Sci USA 97:10526–10531
Celik M, Gökmen N, Erbayraktar S, Akhisaroglu M, Konakc S, Ulukuş C, Genc S, Genc K, Sagiroglu E, Cerami A, Brines M (2002) Erythropoietin prevents motor neuron apoptosis and neurologic disability in experimental spinal cord ischemic injury. Proc Natl Acad Sci USA 99:2258–2263
Constantini S, Young W (1994) The effects of methylprednisolone and the ganglioside GM1 on acute spinal cord injury in rats. J Neurosurg 80:97–111
Dame C, Juul SE, Chiristensen RD (2001) The biology of erythropoietin in the central nervous system and its neurotrophic and neuroprotective potential. Biol Neonate 79:228–235
Digicaylioglu M, Lipton SA (2001) Erythropoietin-mediated neuroprotection involves cross-talk between Jak2 and NF-KappaB signalling cascades. Nature (London) 412:641–647
Ducker TB, Kindt GW, Kempe LG (1971) Pathological findings in acute experimental spinal cord trauma. J Neurosurg 35:700–708
Dusart I, Schwab ME (1994) Secondary cell death and the inflammatory reaction after dorsal hemisection of the rat spinal cord. Eur J Neurosci 6:712–724
Fehlings MG, Tator CH, Linden RD (1989) The effect of nimodipine and dextran on axonal function and blood flow following experimental spinal cord injury. J Neurosurg 71:403–416
Gorio A, Gokmen N, Erbayraktar S, Yılmaz O, Madaschi L, Cichetti C, Di Giulio AM, Vardar E, Cerami A, Brines M (2002) Recombinant human erythropoietin counteracts secondary injury and markedly enhances neurological recovery from experimental spinal cord trauma. Proc Natl Acad Sci USA 99:9450–9455
Grasso G, Buemi M, Alafaci C, Sfacteria A, Passalacqua M, Sturiale A, Calapal G, De Vico G, Piedimonte G, Salpietro FM, Tomasello F (2002) Beneficial effects of systemic administration of recombinant human erythropoietin in rabbits subjected to subarachnoid hemorrhage. Proc Natl Acad Sci USA 99:5627–5631
Kaptanoglu E, Solaroglu I, Okutan O, Surucu HS, Akbiyik F, Beskonakli E (2004) Erythropoietin exerts neuroprotection after acute spinal cord injury in rats: effect on lipid peroxidation and early ultrastructural findings. Neurosurg Rev 27:113–120
Kawakami M, Sekiguchi M, Sato K, Kozaki S, Takahashi M (2001) Erythropoietin receptor-mediated inhibition of excitotoxic glutamate release confers neuroprotection during chemical ischemia. J Biol Chem 276:39469–39475
Mayorov DN, Adams MA, Krassioukov AV (2001) Telemetric blood pressure monitoring in conscious rats before and after compression injury of spinal cord. J Neurotrauma 18:727–736
Rivlin AS, Tator CH (1978) Regional spinal cord blood flow in rats after severe cord trauma. J Neurosurg 49:844–853
Sadamoto Y, Igase K, Skanaka M, Sato K, Otsuka H, Sakaki S, Masuda S, Sasaki R (1998) Erythropoietin prevents place navigation disability and cortical infarction in rats with permanent occlusion of the middle cerebral artery. Biochem Biophys Res Commun 253:26–32
Sakanaka M, Wen T-C, Matsuda S, Masuda S, Morishita E, Nagao M, Sasaki R (1998) In vivo evidence that erythropoietin protects neurons from ischemic damage. Proc Natl Acad Sci USA 95:4635–4640
Sasaki R, Masuda S, Nagao M (2000) Erythropoietin: multiple physiological functions and regulation of biosynthesis. Biosci Biotechnol Biochem 64:1775–1793
Sekhom LH, Fehlings MG (2001) Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine 26:S2–S12
Siren AL, Knerlich F, Poster W, Gleiter CH, Bruch W, Ehrenreich H (2001) Erythropoietin and erythropoietin receptor in human ischemic/hypoxic brain. Acta Neuropathol (Berl) 101(3):271–276
Springborg JB, Ma X, Rochat P, Knudsen GM, Amtorp O, Paulson OB, Juhler M, Olsen NV (2002) A single subcutaneous bolus of erythropoietin normalizes cerebral blood flow autoregulation after subarachnoid haemorrhage in rats. Br J Pharmacol 153:823–829
Squadrito F, Altavilla D, Squadrito G, Campo GM, Arlotta M, Quadrito C, Saitta A, Caputi AP (1999) Recombinant human erythropoietin inhibits ÝNOS activity and reverts vascular dysfunction in splanchnic artery occlusion shock. Br J Pharmacol 127:482–488
Xu J, Kim G, Chen S, Yan P, Ahmed SH, Ku G, Bechman JS, Xu X M, Hsu CY (2001) İNOS and nitrotyrosine expression after spinal cord injury. J Neurotrauma 18:523–532
Zileli M, Özer F (1997) Pharmacological treatment in spinal cord injuries. In: Zileli M, Özer F (eds) Spinal cord and spine surgery, 1st edn. Saray, Izmir, 466 pp
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Çetin, A., Nas, K., Büyükbayram, H. et al. The effects of systemically administered methylprednisolone and recombinant human erythropoietin after acute spinal cord compressive injury in rats. Eur Spine J 15, 1539–1544 (2006). https://doi.org/10.1007/s00586-006-0091-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-006-0091-2